Chapter 4 Diagnosis
Introduction
A diverse range of clinicians practise CAM across the globe, each with varying levels of education and disparate methods of practice. While noticeable differences in service delivery are expected between CAM disciplines, there is no reason why CAM practitioners cannot practise consistently within each specialisation. A method to improve practice consistency within the field of CAM is DeFCAM (in particular, the application of diagnostic reasoning and the formulation of CAM diagnoses). The purpose and rationale for using CAM diagnoses in clinical practice is elucidated throughout this chapter, followed by examples of how these diagnoses can be structured and documented in order to ameliorate client care, enhance clinical outcomes and facilitate the professionalisation of CAM. First though, it is important to understand what the term ‘diagnosis’ represents.
Defining diagnosis
A diagnosis is a statement that identifies the nature or cause of a given phenomenon.1 What this definition highlights is that diagnosis is not a term limited to the healthcare sector, but a phrase used in any industry, including the automotive, engineering and computing sectors. One factor distinguishing a diagnosis made by a health professional to one formulated by a non-health-related discipline is the human element. Even though this element is shared by the health occupations, each healthcare profession interprets diagnosis differently. A medical diagnosis, for instance, is the identification of a specific disease or pathological condition based on a presenting pattern of signs and symptoms. By contrast, a nursing diagnosis is a statement that defines a human response to an actual or potential health problem that nurses can recognise and treat. A nutrition diagnosis is a ‘food and nutrition professional’s identification and labelling of an existing nutrition problem that the food and nutrition professional is responsible for treating independently’.2 The key point that emerges from each of these definitions is that diagnoses are profession-specific, that is, each profession has a particular knowledge base and skill set to competently formulate and treat specific types of diagnoses. In other words, while a nurse may be qualified to generate and treat nursing diagnoses, in most cases they would not be able to competently formulate or treat nutritional or medical diagnoses. Put simply, nurses make nursing diagnoses, dieticians make nutrition diagnoses.
Rationale for diagnosis
From an affirmative position, clinical diagnoses may help to focus a practitioner’s attention towards the cause of a client complaint. This argument supports one of the philosophical principles of CAM, that is, addressing the aetiology of the presenting condition. Through a better understanding of the cause of an illness, a clinical diagnosis can assist the clinician to create a more specific and pertinent treatment plan and, in effect, hasten the attainment of positive client outcomes. The treatment approach for an individual presenting with general fatigue, for instance, would be comparatively less specific, less individualised and potentially less effective than a plan for a client diagnosed with hypothyroidism and, as such, would inevitably hinder clinical progress. As well as the benefits to the client and CAM practitioner, clinical diagnoses can also help to improve interprofessional communication by providing a common language that is understood by most CAM and orthodox practitioners.
Factors affecting diagnostic accuracy
Other than the benefits mentioned above, clinical diagnosis also provides a clear and transparent link between assessment and treatment. It is not surprising, therefore, that misdiagnosis can lead to delayed or inappropriate clinical management and/or unnecessary disease progression that result in an increased risk of client morbidity and/or mortality. Even though the rate of misdiagnosis is uncertain in most countries due to the paucity of valid and reliable data, a German study of 100 randomly selected patients who died in hospital in 1999–2000 sheds some light; it reported a rate of misdiagnosis of eleven per cent.3 The global impact of misdiagnosis on all-cause morbidity and mortality has also been poorly investigated, although the social consequences are somewhat clearer, with more than twenty-one per cent of new public and private sector medical indemnity claims made in Australia in 2005–06 attributed to diagnostic error.4 Recognising and addressing the many determinants of diagnostic accuracy may help to minimise the risk of adverse events, as well as the subsequent risk of litigation against CAM practitioners.
Personal factors relate to practitioner self-confidence, beliefs, preferences, stress coping strategies and short-term memory capacity.5 The effect on clinical performance of alcohol, illicit drugs and/or excessive fatigue is a good case in point. A practitioner directly affected by these elements may, for instance, have difficulty retaining and processing information, which could lead to higher rates of diagnostic error and potentially delay client progress.
Among the extrinsic influences of diagnostic accuracy are the environmental elements. These refer to the availability of diagnostic resources, type of clinical setting, time constraints and interruptions or distractions. Resource access is a particular concern for most CAM practitioners, as many do not have access to subsidised investigations or have the skills or competencies required to perform these tests (at least not in Australia). Without access to certain investigations, or access to clinicians who have the capacity to perform these tests, some practitioners may have difficulty in establishing a diagnosis or determining the possible causes of the presenting complaint.
Adding to these factors are a number of elements that may further increase the risk of misdiagnosis in CAM practice, determinants that include limited access to diagnostic tools, variability of professional educational standards and limited interprofessional communication.6 The effect of training and education on diagnostic competency, in particular, has been recently highlighted in a survey of 617 Australian CAM practitioners. The study found that most clinicians used Western and CAM diagnostic techniques that they had received training in, except for the interpretation of pathological and radiological tests, of which one-third of practitioners had not received any training, even though they interpreted these tests in clinical practice.7 This is of concern, as adequate training is needed to develop sufficient competency in diagnostic skills8 in order to reduce the risk of misinterpretation and misdiagnosis.
Training in a variety of diagnostic tests has also been shown to be positively related to practitioner confidence in identifying clients requiring referral (p<0.05),7 which again highlights the probable association between inadequate education and increased risk of client harm. Thus, given that thirty-four per cent of patients were reported by Grace et al7 to have occasionally or never been assessed by a doctor prior to a CAM consultation, and that many CAM practitioners may not have the necessary skills, tools, confidence or competency to accurately diagnose or refer, suggests that some groups of clients may be at greater risk of being misdiagnosed and of receiving delayed or inappropriate treatment.
The process of diagnostic reasoning
Diagnostic reasoning, which is a ‘dynamic thinking process that … leads to a diagnosis that best explains the symptoms and clinical evidence in a given clinical situation’,9 may help clinicians to bridge the gap between assessment and diagnosis. Given that assessment and diagnosis are closely linked, however, with both steps informing each other, it is important to acknowledge that diagnostic reasoning is not a process limited to the third phase of DeFCAM, but it is another essential component of clinical assessment.
Guiding CAM practitioners through the process of diagnostic reasoning needs to take into account a number of important elements. Experience, for instance, is one factor that can influence the adopted style of diagnostic reasoning, as well as the quality of client outcomes. Even so, expertise takes time to acquire and, depending on the opportunities that present to the practitioner, experience may not necessarily lead to the development of an effective or efficient reasoning process. This is because a theoretical foundation needs to inform the process. Therefore, a factor that may greatly improve the outcomes of diagnostic reasoning, and one that does not discriminate between novice and expert clinicians, is the adoption of an appropriate critical thinking framework.
Apart from assisting CAM practitioners to better understand how healthcare professionals with different levels of expertise formulate clinical diagnoses, diagnostic reasoning models enable practitioners to recognise how to acquire, combine and process information to improve diagnostic accuracy,10,11 and thereby to solve clinical problems. In fact, Groves et al11 have shown that clinicians who follow a clear and streamlined diagnostic reasoning process and who interpret data correctly demonstrate greater diagnostic accuracy than practitioners who adopt a less efficient reasoning approach. The vast number of diagnostic reasoning models available to educators and practitioners of CAM (Table 4.1), as well as the frequent use of jargon within these frameworks, may make the selection of an appropriate model difficult.
Table 4.1 Examples of diagnostic reasoning models
| Bowen (2006) process12 | Data acquisition, problem representation, hypothesis generation, illness script selection, and final diagnosis |
| Clinical reasoning process (Groves et al 2003)11 | Identify relevant information, data interpretation, data integration, hypothesis generation, hypothesis testing, and working diagnosis |
| Clinical thinking process (Bates 1995)13 | Identify abnormal findings, cluster data, localise findings, interpret data, generate hypotheses, test hypotheses, and define problem |
| Diagnostic strategy (Murtagh 2007)14 | Determine probability diagnosis, potentially serious disorders, possible pitfalls, masquerading conditions, and patient hidden agendas |
| Hermeneutical model (Ritter 2003)15 | Pattern recognition, similarity recognition, common-sense understanding, skilled know-how, senses of salience, deliberative rationality, data gathering, and cue interpretation |
| Hypothesis-driven strategy (Szaflarski 1997)16 | Problem identification, hypothesis generation, hypothesis evaluation, hypothesis analysis, hypothesis assembly, and final diagnosis |
| Information processing model (Ritter 2003)15 | Data collection, further cue acquisition, formulation of possible solutions, problem identification, hypothesis generation, cue interpretation, and hypothesis evaluation |
| Nagelkerk (2001) process17 | Formulate competing diagnoses, order diagnostics, and select a diagnosis |
| Nursing diagnostic model (Perry 2008)18 | Data validation, data clustering, data interpretation, identification of client needs, and formulation of nursing diagnosis |
| Participative decision-making model (Ballard-Reisch 1990)19 | The diagnostic phase of the model consists of two stages – information gathering, and information interpretation |
| Zunkel et al (2004) model9 | Data collection, data synthesis, and hypothesis formation |
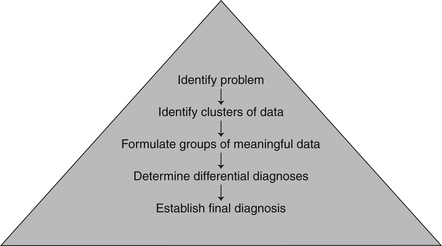
In order to simplify matters, diagnostic reasoning frameworks can be categorised into two main styles, that is, models based on inductive or deductive reasoning. Inductive reasoning, which guides the Hermeneutical, nursing diagnostic and Zunkel et al9 models, is a bottom-up reasoning approach by which specific data are developed into generalisations. As illustrated in Figure 4.1, the approach refers to the processing of specific symptoms and observations acquired during clinical assessment into meaningful clusters of information. These clusters are then continuously grouped into larger and more meaningful chunks of data until an appropriate diagnosis or range of differential diagnoses are generated. In clinical terms, this style of reasoning may progress as follows: succeeding the completion of a client assessment, specific symptoms such as pyrexia and malaise can be clustered together to represent any number of infectious or oncological disorders. When another cluster of data is added to the equation, such as dysuria and increased urine odour, the new chunk of information portrays greater meaning. In this example, the two clusters of data suggest that a urological condition may be present. Additional information from a urinalysis and urine culture can then be used to either support or dismiss a diagnosis of symptomatic bacteriuria.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree