INTRODUCTION
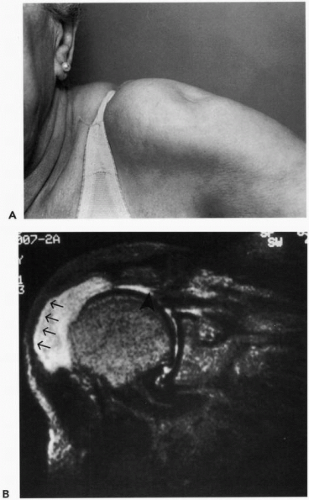
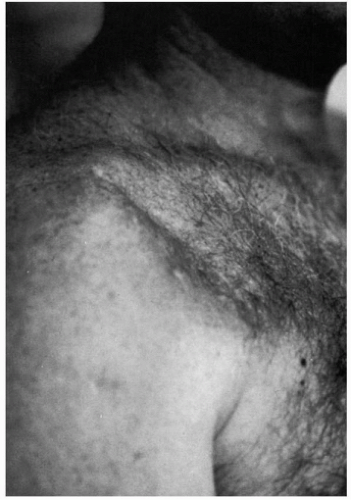
Injuries to the deltoid muscle occur relatively infrequently compared with other, more common shoulder disorders such as those involving the rotator cuff. Regardless of the cause, these injuries can often result in significant shoulder dysfunction. An understanding of the functional anatomy of the deltoid and the mechanisms of injury can help to minimize iatrogenic causes and enable the formulation of optimal treatment strategies.
ANATOMY AND FUNCTION
The importance of the deltoid in providing active elevation of the arm is readily appreciated when considering the compromised function associated with pathologic conditions affecting this muscle. Approximately 60% of the strength in abduction and elevation in both the coronal and scapular planes, respectively, is attributed to the deltoid, as determined after anesthetic block of the axillary nerve. Progressive loss of muscle force with increased abduction and early fatigue further compromises shoulder function in such individuals.
16Some reports cite sporadic cases of functional elevation of the arm in patients with isolated and complete paralysis of the deltoid.
3,
19,
36,
58 Preservation of active elevation was attributed to the compensatory action of the rotator cuff, pectoralis major, trapezius, and serratus anterior muscles.
3 Despite the ability to raise the unweighted arm, considerable deficits in abduction strength occurred in addition to abnormal scapulohumeral mechanics, impairment of humeral extension, and early fatigability.
3,
19,
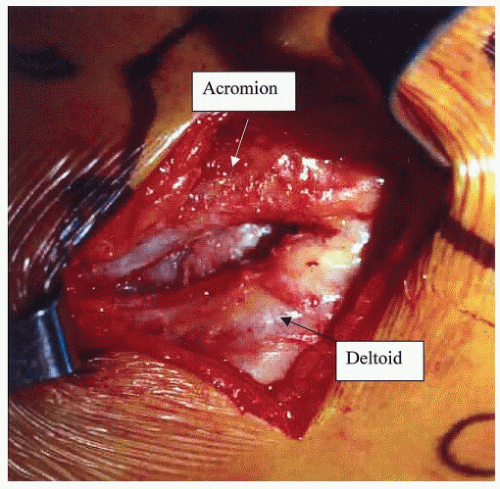
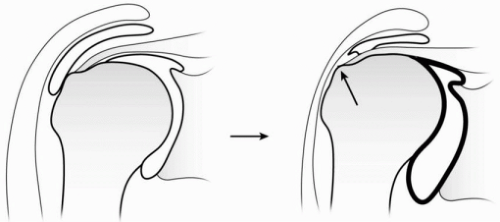
58Anatomically, the deltoid comprises three distinct heads: the anterior, the middle, and the posterior portions, which vary in both structure and function. Its extensive origin forms a horseshoe-type configuration arising from the distal one-third of the clavicle, the acromion, and the lateral one-third of the spine of the scapula. Distally, the muscle converges to insert on the deltoid tuberosity of the middiaphysis of the humerus. Its broad origin, which is derived from the mobile scapula and clavicle, affords the deltoid a mechanical advantage by allowing the muscle to maintain its resting length at various arm positions. The bipennate structure of the large middle head contributes to abduction strength through contraction of its fibers at an angle to the line of pull, which also serves to maintain muscle fiber resting length and improve efficiency. In contrast, muscles with a parallel fiber arrangement such as the anterior and posterior deltoid, by virtue of their structural configuration, result in considerably decreased strength during contraction.
21Differences in activity of the deltoid’s three portions, relative to arm position, have also been observed through electromyographic analysis.
57 The anterior and middle heads remain active at all angles of abduction and in multiple planes (coronal, scapular, and parasagittal), whereas the posterior deltoid, also an important shoulder extensor, contributes to elevation when the arm is above 110 degrees.
57 Abduction in the coronal rather than scapular plane effects a relative increase in posterior deltoid function and a decrease in anterior deltoid activity.
31 When the arm is in abduction, the posterior deltoid functions as a secondary external rotator, and its clinical importance is increased in patients with massive rotator cuff tears involving the infraspinatus tendon. Its function as a secondary external rotator is greatest with the arm posterior to the plane of the scapula and at 90 degrees of abduction.
Neural innervation is afforded by the axillary nerve, which takes a circuitous path before entering the deltoid muscle. It arises from the posterior cord of the brachial plexus and courses across the inferolateral border of the subscapularis approximately 3 to 5 mm medial to the musculotendinous junction.
37 It passes inferior to the glenohumeral axillary recess and exits the quadrangular space where it divides into two trunks. The posterior trunk splits and innervates the teres minor and posterior deltoid before terminating as the superior lateral cutaneous nerve. The anterior trunk winds around the humerus and innervates the remaining deltoid muscle. It becomes subfascial and intramuscular at a point between the anterior and middle heads.
13 It is generally located one-third the distance from the lateral acromion to the deltoid tuberosity, which in most patients is 4.4 cm from the lateral acromion.
Cause
Although a host of disorders can affect the function of the deltoid, this chapter focuses on lesions isolated to the axillary nerve and those affecting the musculotendinous integrity of the deltoid. For the purpose of completeness,
Table 34-1 has been included and represents a comprehensive list of causative factors that can contribute to deltoid muscle dysfunction.



 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access