Deepening Trochleoplasty
David Dejour
Justin W. Griffin
Paulo Saggin
David R. Diduch
DEFINITION
Trochlear dysplasia is a pathologic condition occurring in approximately 3% of the population but up to 96% of those with recurrent patellar instability.9 The condition is one in which structural abnormalities of the femoral trochlea results in patellar instability.
Trochlear dysplasia is a flattened, shallow or even convex trochlear groove, providing inadequate bony restraint for the patella, and possibly, a “supratrochlear spur” or bump that deflects the patella laterally.8
Depth and morphology of the trochlea is both necessary and sufficient in combination with soft tissue restraints to provide a stable patellofemoral articulation. The aim of surgery is to restore this relationship.10
Currently, sulcus-deepening trochleoplasty as described by David Dejour is for correction of the trochlear morphology and is one option for addressing high-grade trochlear dysplasia2 in patients presenting with patellar dislocation.
ANATOMY
The normal trochlea has an intricate three dimensional shape located in the anterior aspect of the distal femur. The trochlea is composed of two facets divided by the trochlear sulcus, a longitudinal groove that varies in length and mediolateral position.9
The lateral facet is higher than the medial facet (extends further in the anteroposterior [AP] plane) and extends more proximally up the femur.3
The normal trochlear sulcus extends proximally from the intercondylar notch until it meets and is level with the anterior cortex of the femur. Distally, the medial and lateral facets extend to the point of becoming the femoral condyles at the sulcus terminalis.
The trochlea guides patellar tracking with the opposing patellar surface following the trochlear groove.
The medial patellofemoral ligament (MPFL) is an extraarticular ligament that attaches from the patella medial surface to the femur posterosuperior to the medial femoral epicondyle (9.5 mm proximal and 5.0 mm posterior to the center of the medial femoral epicondyle).14 The MPFL is the primary soft tissue restraint to lateral patellar dislocation.
Patellar stability depends on bony and soft tissue architecture. In full extension, soft tissue restraints are dominant. The patella normally engages within the trochlear groove by 30 degrees of flexion. With trochlear dysplasia, the dysmorphic trochlea is unable to guide the patella, resulting in tilt and ultimately dislocation. The dysplastic trochlea also forces the medial retinacular ligaments (ie, the MPFL) to take on a greater role.
Trochlear dysplasia describes a trochlear groove, which is shallow or even convex. The abnormal shape of the trochlea often is accompanied by a superolateral bump or supratrochlear spur best viewed on a lateral x-ray or computed tomography (CT) scan.6
The larger the supratrochlear spur, the greater the reaction force pushing the patella out of the groove.
PATHOGENESIS
The etiology of trochlear dysplasia remains unclear. It is unknown at this time whether trochlear shape is present throughout one’s lifetime or changes over time. Some authors have suggested a genetic origin of trochlear dysplasia.11,12 However, to date, there are no prospective studies looking at trochlear development and dysplasia.
Other authors have suggested a developmental process whereby a lateralized patella due to malalignment or other causes may lead to abnormal development of the trochlear groove.20 Consensus opinion would suggest trochlear dysplasia is a primary abnormality that increases during growth in the setting of malalignment.
Patellar dislocation is the result of lack of bony or soft tissue constraint of the patella within the trochlear groove. Recurrent patellar instability often results when soft tissue constraints (ie, MPFL), dynamic muscular constraints, or osseous restraints fail. Patellar instability may be acute or chronic in nature.13
NATURAL HISTORY
The overall risk of patients presenting with a history of dislocations for a recurrent dislocation is 50% over a 2- to 5-year period.5
Younger patients (younger than 18 years old) and females also tend to have a higher risk of recurrent dislocation.
Nonsurgical treatment in patients with underlying anatomic predisposing factors leading to instability has a recurrent dislocation rate near 43% versus a 20% redislocation rate in those patients without predisposing factors.4
A combination of other predisposing factors, including increased tibial tuberosity-trochlear groove (TT-TG), patella alta, vastus medialis obliquus (VMO) dysplasia, MPFL attenuation, and rotational malalignment, may also be present in the setting of trochlear dysplasia.2
In the setting of trochlear dysplasia, many patients present after having failed prior realignment or soft tissue procedures. This demonstrates the contribution of bony abnormality to recurrent dislocation.13
PATIENT HISTORY AND PHYSICAL FINDINGS
Trochlear dysplasia should be considered in any patient with a history of recurrent patellar instability. The history of dislocations should be ascertained, including details
regarding the first dislocation as well as treatment and surgeries to date.
History should include evaluation for possible osteochondral injury.
It should be ascertained whether the patient is largely concerned about pain or instability. Most patients with recurrent instability from trochlear dysplasia do not experience generalized anterior knee pain between episodes.
The type of activities and frequency in which dislocation occurs should be queried.
Lower extremity alignment should be noted as well as the presence of an effusion. A thorough knee examination should be performed.2
Several clinical tests have been described that focus on examination of patellar tracking and concomitant patella pathology.
General active and passive tracking should be evaluated.
Tenderness about the medial patella and MPFL insertion should be elicited.19
Patellar apprehension—should be evaluated at full extension. A positive test is pathognomonic for patellar instability.
Quadrant test—the patella should passively translate between one and two quadrant widths of the patella with the knee extended.
Moving patellar apprehension test—involves pushing the patella laterally as the knee is passively brought into flexion.1 Comparison is made to the opposite knee for amount of patellar translation and degree of flexion at which the patella is firmly stable within the trochlear groove.
A “J sign” refers to lateral patellar deviation during terminal knee extension as the patella exits the proximal groove and reflects patella alta and/or high-grade trochlear dysplasia.
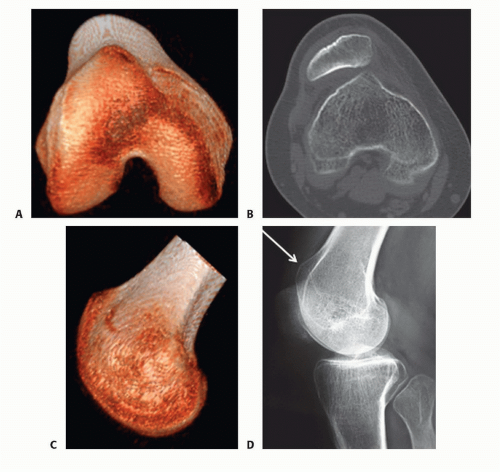
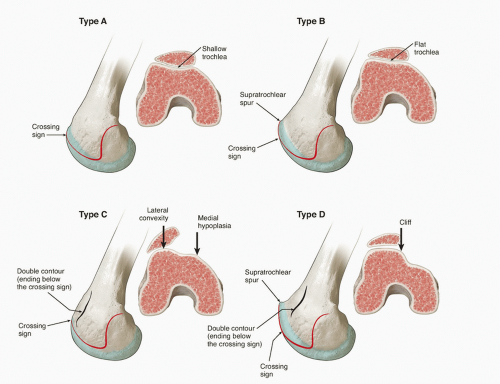
FIG 1 • Dysplastic trochlea demonstrating a supratrochlear bump on CT imaging (A-C). Supratrochlear spur demonstrated on the lateral view (arrow) (D).
Patella grind or compression test should be performed to rule out articular degeneration, although this does have a high rate of false positives.
Patellar tilt test—the examiner’s thumb attempts to flip the lateral edge of the patella upward, slightly off the lateral trochlear facet to horizontal. This is compared to the opposite knee as are all of these tests.
No physical examination tests are available specifically for trochlear dysplasia.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs including weight-bearing posteroanterior (PA), true lateral, and axial patellar views at 30 to 45 degrees of flexion should be obtained.2,6,8,9 The lateral radiograph is the key image.
Evaluation of the lateral radiograph includes identification of several important features:
Crossing sign—radiographic line of the trochlear sulcus as it crosses the projection of the femoral condyles. This represents the location at which the deepest part or floor of the trochlear sulcus reaches the same height as the femoral condyles. Hence, at this point, the trochlea is flat and at the same level as the anterior borders of the trochlear facets.
In normal knees, the radiographic line representing the base of the trochlear groove merges with the anterior femoral cortex proximally at the end of the groove. However, in dysplastic trochlea, it can be several millimeters in front of the cortex representing the supratrochlear bump.6
Supratrochlear spur—a pronounced, superolateral bony bump or projection at the top of the dysplastic trochlea that sits well anterior to the femoral cortex (FIG 1).
Double contour sign—represents the hypoplastic medial facet seen in profile compared to the taller lateral facet and even the base of the trochlear groove, as both sit higher or more anterior.
Caton-Dechamps ratio can be calculated to evaluate for patella alta and need for distalization of the tibial tubercle. This is the distance from the distal articular surface of the patella to the tibial plateau, divided by the length of the articular surface of the patella.
Merchant (axial) views at 45 degrees of flexion allow for general characterization of patellar shape and tilt as well as morphology of the groove, although this does vary with the degree of knee flexion. Knee flexion of 30 degrees is ideally recommended as greater degrees of flexion will underestimate dysplasia.3
Sulcus angle—from the point of the bottom of the trochlear groove, two lines are drawn connecting to the most superior point of each facet and the subtended angle measured. Normal is typically 138 degrees. A sulcus angle over 145 is indicative of dysplasia. Severely dysplastic trochlea may show very high angles or are unmeasurable (over 180 degrees or convex).
It is important to understand that simply observing a flattened trochlear groove on a Merchant x-ray view is a small part of diagnosing trochlear dysplasia and that evaluation of the supratrochlear bump or spur sitting anterior to the femoral cortex is most important and the feature to which surgical treatment is directed for a groove-deepening procedure.
Classification can be based on characteristic morphology using both standard imaging and advanced cross-sectional imaging (CT scan or MRI) as described by Dejour and Le Coultre7 (FIG 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree