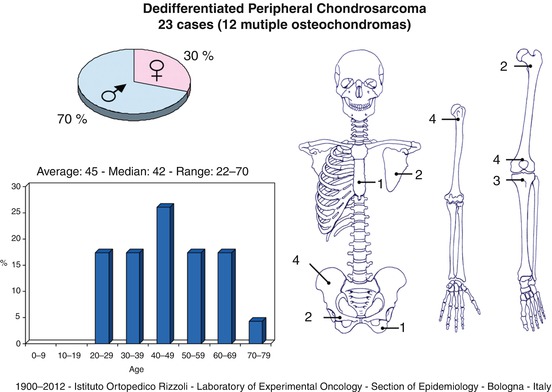
Location: Proximal femur, pelvis, and proximal humerus.
Clinical: On a history of long duration with moderate symptoms, a rapid progression of pain and swelling occurs. Pathologic fractures frequent.
Imaging: On x-ray: (1) old cartilaginous lesion: moderate expansion of the bone with thickened, scalloped cortex, with many calcifications; (2) new lesion: destroying the cortex, involving the soft tissues, and dissolving the calcifications, with ill-defined margins. Three different features are as follows: (a) pathologic fracture in a new aggressive lytic lesion canceling preexisting calcifications of an intensely radiopaque old cartilaginous lesion, (b) usual chondrosarcoma aspect with a small high-grade lytic lesion, (c) typical high-grade sarcoma feature with small remnants of chondrosarcoma. On CT, two lesions of different density, matrix, and enhancement. On MRI, two different signal intensities on T1 and T2.
Histopathology: Two types of tissues: (1) low-grade cartilaginous tumor and (2) high-grade malignancy like UPS, OS, FS. The transition is sharp.
Course and Staging: Fast growth, high risk of recurrence with inadequate surgery, and high rate of metastases, often observed at diagnosis. Usually, stage IIB or III.
Treatment: Wide or radical resection. Chemotherapy protocols of OS have been used with effectiveness. Often, an amputation is necessary to obtain adequate margins. Poor prognosis.
Key Points
Clinical | Symptoms rapidly increasing. Pathologic fracture possible |
Radiological
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





