Custom Acetabular Components for Acetabular Revision
Douglas A. Dennis
Raymond H. Kim
David N. Conrad
Case Example
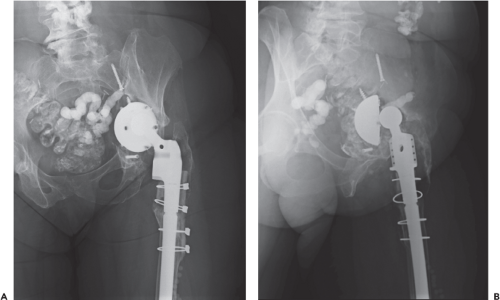
LT is a 63-year-old female who developed disabling posttraumatic osteoarthritis secondary to a traumatic hip dislocation and underwent a primary cemented total hip arthroplasty (THA) in 1977. Because of polyethylene wear and osteolysis, she developed both femoral and acetabular component loosening, with a subsequent femoral component revision in the mid-1980s and an acetabular component revision in the early 1990s. Her left THA functioned well until 2001 when she developed a periprosthetic infection, which was treated with a two-stage exchange arthroplasty. At that time, substantial acetabular bone loss was encountered which was managed with morselized allografting and a jumbo acetabular component. Her revision THA functioned well until 2007 when she presented with a 2-month history of progressive left hip discomfort. Examination of her radiographs demonstrated substantial superior and medial migration of the acetabular component with a likely underlying pelvic discontinuity (Fig. 115.1). Laboratory studies and a hip aspirate were negative for infection. A thin-cut computed tomography (CT) scan was obtained to confirm the pelvic discontinuity and assess the magnitude of periacetabular bone loss. Given the massive periacetabular
osteolysis, pelvic discontinuity, and lack of adequate bone stock to support a traditional noncustom revision component, plans were made for acetabular reconstruction with a custom triflanged acetabular component (CTAC).
osteolysis, pelvic discontinuity, and lack of adequate bone stock to support a traditional noncustom revision component, plans were made for acetabular reconstruction with a custom triflanged acetabular component (CTAC).
Introduction
Current treatment options for massive acetabular defects encountered in revision THA are numerous but often associated with inconsistent clinical results and substantial complication rates. These reconstructive options include reconstruction with jumbo acetabular components (1), bipolar hemiarthroplasty (2), use of acetabular impaction bone grafting (3), massive structural allografts (4,5,6), oblong acetabular components (7,8,9), modular trabecular metal cups with augments (10,11,12), and noncustom acetabular reconstruction rings (4,13,14). Difficulties associated with these methods in patients with massive periacetabular bone loss have included loss of fixation, component fracture, hip instability, and gait alterations caused by failure to restore functional hip biomechanics (1,4,5,6,7,8,9). Another implant option designed to limit these failure mechanisms is a CTAC. This chapter describes the indications, design methods, surgical technique, results, and complications of the CTAC used to reconstruct massive acetabular defects in revision THA.
Indications and Contraindications
Patients may incur massive periacetabular bone loss with or without a pelvic discontinuity for a variety of reasons. The most common cause is periprosthetic osteolysis associated with component loosening with migration secondary to excessive polyethylene wear. Periacetabular bone loss in revision THA has been classified by Paprosky (Table 115.1) (15) and the Academy of Orthopedic Surgery (AAOS; Table 115.2) (16). These classifications are based on the severity of bone loss and ability to obtain implant fixation. Generally, traditional means of acetabular reconstruction other than CTACs are appropriate for Paprosky classes I to IIIA and AAOS classes I and II. The presence of massive periacetabular bone loss (Paprosky 3B and AAOS III & IV) that precludes the ability to obtain a stable acetabular reconstruction with a revision hemispherical component is the primary indication for the use of a CTAC (17,18,19,20,21,22). The use of bulk allograft and impaction grafting with traditional acetabular components in these cases has demonstrated failure rates as high as 36% in some series (3,4,5,6). The ability of these allografts to incorporate and withstand physiologic loads is questionable and is a likely cause for the unacceptably high failure rates.
The development of thin-cut spiral CT scans and multiplanar image reconstruction has revolutionized the use of custom arthroplasty components. With these three-dimensional (3D) images, surgeons working in conjunction with implant manufacturers, are able to create a custom component that bridges the periacetabular bone loss, obtains immediate stable fixation on bone distant from the deficient acetabulum (ilium, ischium, and pubis), and restores hip biomechanics. Although various bone grafting procedures can be utilized with this technique, these components do not rely up on bone graft for initial or long-term fixation. However, in cases in which adequate pelvic bone quality to obtain screw fixation on bone distant from the acetabulum does not exist, or in the setting of persistent infection, use of a CTAC is contraindicated. A relative contraindication for use of these devices are cases with a pelvic discontinuity in which osteolysis has created large gaps (>1 cm) between opposing bone surfaces. Although the authors have successfully treated such cases with bone grafting in conjunction with implantation of a CTAC, their highest failure rates have occurred in this clinical situation.
Table 115.1 Paprosky Classification of Acetabular Defects | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 115.2 AAOS Classification of Acetabular Defects | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Preoperative Planning
As with any arthroplasty evaluation, the initial step in management is a thorough history and physical examination. The history should include the reason for initial arthroplasty, as well as the reason for any subsequent revision procedures. A detailed investigation for infection is essential including an erythrocyte sedimentation rate and C-reactive protein. Since patients requiring a CTAC have typically incurred multiple previous operative procedures, it is also wise to perform a hip aspiration for culture and cell count analysis. Previous operative records should be reviewed to note the operative exposure used, any complications or unusual techniques involved, and to determine the type, size, and fixation method of the currently implanted components. Careful examination should be performed including inspection of the skin for the presence of fluctuance, warmth, erythema, and the location and condition of previous skin incisions. The neurovascular status of the limb must be assessed as well as the symmetry of leg lengths. Lastly, the motor function of the lower extremities must be evaluated, particularly the function of the abductor musculature, as this can be predictive of future postoperative problems with hip instability. In cases where the competence of the abductor musculature is in question, the surgeon should be prepared with options including a constrained liner, or a dual mobility articulation as large heads alone may not be adequate to prevent dislocation if the abductors are deficient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree