The challenge of confirming the diagnosis of prosthetic hip infection is two-fold. First, the presentation of the patient with a prosthetic hip infection often has limited or few subjective complaints and physical findings, nonconfirmatory inflammatory laboratory markers, and negative culture results. Second, there has not been consistent agreement of the definition of prosthetic join infection. Recent work by the Musculoskeletal Infection Society has created a new uniform definition for research and clinical use that may improve the ability to accurately diagnose prosthetic hip infections individually and share data among different sites for research collaboration.
Key points
- •
The diagnosis of prosthetic hip infection involves multiple modalities, including an initial clinical evaluation, appropriate laboratory studies, and intraoperative assessment.
- •
Arthrocentesis should be performed in all patients with suspected prosthetic joint.
- •
A minimum of three, optimally up to six cultures of the periprosthetic tissue should be obtained to aid in the diagnosis of prosthetic joint infection.
- •
Although ESR and CRP remain the standard of care in serum laboratory diagnosis of prosthetic joint infection, other biomarkers are under investigation.
- •
Newer diagnostic techniques, such as sonication and molecular analysis, may be helpful in the diagnosis of prosthetic joint infection.
Introduction
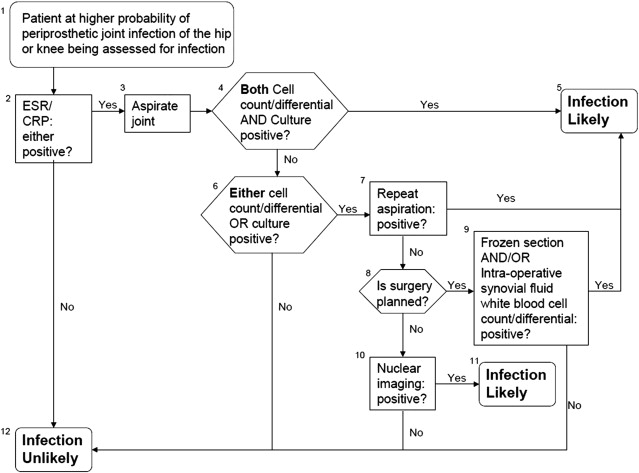
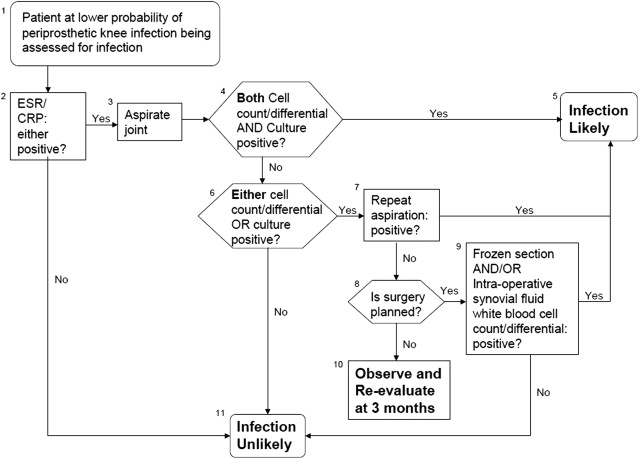
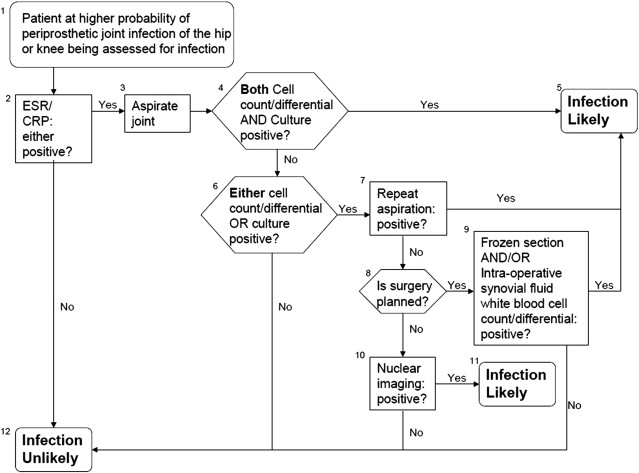
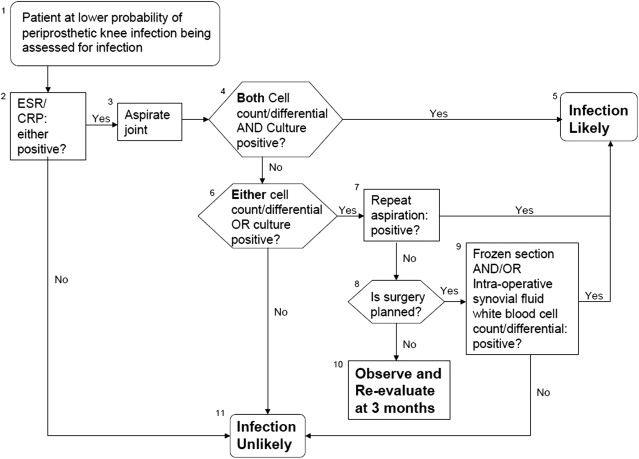
The appropriate diagnosis of a prosthetic hip infection is a critical first step to successful management and functional recovery of the patient. The challenge of confirming the diagnosis is two-fold. First, the presentation of the patient with a prosthetic hip infection often has limited or few subjective complaints and physical findings, nonconfirmatory inflammatory laboratory markers, and negative culture results. Secondly, there has not been consistent agreement of the definition of prosthetic join infection. Different authors and institutions have used many combinations of blood tests, histologic analysis, synovial fluid, and tissue culture results and clinical findings to define the presence of infection. Recent work by the Musculoskeletal Infection Society has created a new uniform definition for research and clinical use. This may improve the ability to accurately diagnose prosthetic hip infections individually and share data among different sites for research collaboration. The incidence of prosthetic hip infection has remained at approximately 2% for the last past several years. By following consistent diagnosis criteria established for hip and knee infections, we may actually see an increase in the number of identified prosthetic hip infections ( Figs. 1 and 2 ).
Introduction
The appropriate diagnosis of a prosthetic hip infection is a critical first step to successful management and functional recovery of the patient. The challenge of confirming the diagnosis is two-fold. First, the presentation of the patient with a prosthetic hip infection often has limited or few subjective complaints and physical findings, nonconfirmatory inflammatory laboratory markers, and negative culture results. Secondly, there has not been consistent agreement of the definition of prosthetic join infection. Different authors and institutions have used many combinations of blood tests, histologic analysis, synovial fluid, and tissue culture results and clinical findings to define the presence of infection. Recent work by the Musculoskeletal Infection Society has created a new uniform definition for research and clinical use. This may improve the ability to accurately diagnose prosthetic hip infections individually and share data among different sites for research collaboration. The incidence of prosthetic hip infection has remained at approximately 2% for the last past several years. By following consistent diagnosis criteria established for hip and knee infections, we may actually see an increase in the number of identified prosthetic hip infections ( Figs. 1 and 2 ).
Clinical examination
The clinician evaluating a patient with a possible prosthetic hip infection must be aware of the vast array of signs and symptoms that may be present. The most common complaint is pain in the hip area (buttock, lateral hip, groin, or thigh). The symptom of pain associated with this inflammatory process is usually present at all times, but may be most noticeable while the patient is inactive or at rest. Activity usually has little effect on the pain, but may distract the patient from its presence and intensity for brief periods of time. A complete clinical history including questions about the presence of comorbid conditions, history of previous infections and subsequent management, history of poor wound healing, and information about any current symptoms should be obtained. While the clinician is obtaining history from the patient, it is important to ask about the history of the surgical procedure. Specifically, surgical records that can inform the clinician about the length of surgery, type of implant that was used, and if there were intraoperative challenges that resulted in prolonged surgical time. Any history of perioperative infections (such as urinary tract or pneumonia, wound infections, or others that may have caused transient bacteremia) should also be noted. All pertinent medical records should be obtained and reviewed, including prior history and physical assessments, operative reports, and any relevant diagnostic studies including previous culture results.
A thorough physical examination should be performed, paying close attention to the surgical incision, including evaluation of drainage or the presence of a sinus tract. Areas of tenderness about the hip reflecting sites of inflammation or abscesses should also be evaluated. Range-of-motion of the hip may or may not be affected; however, stiffness of the joint is a common finding for those patients with an infection.
Radiographs of the prosthetic joint are routinely ordered to evaluate for the presence of findings consistent with infection (progressive radiolucent lines, osteolysis, or periosteal new bone formation). The use of additional radiographs is of limited value. Specifically, nuclear imaging (labeled-leukocyte imaging combined with bone or bone marrow imaging, F-18 fluorodeoxyglucose-positron emission tomography [FDG-PET] imaging, or gallium imaging) may be of benefit but limited information supports their routine use. Furthermore, with variability in imaging studies special expertise may be required for these particular images. Magnetic resonance imaging is another diagnostic test that has the potential to be helpful, but this has not been definitively established.
Inflammatory markers, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), are essential laboratory tests to be included in the diagnostic evaluation of a patient suspected of having a prosthetic joint infection. Greidanus and colleagues performed a prospective study on patients being evaluated before revision surgery. Schinsky and colleagues performed preoperative evaluation in 235 painful total hip arthroplasties. The studies performed in the work-up of this population included ESR, CRP, fluid aspiration for white blood cell (WBC) count, intraoperative frozen section analysis of patients from the joint tissue, and permanent histopathologic examination of this tissue. When the CRP and ESR were both elevated above their normal ranges, the sensitivity and specificity were 91% and 95%, respectively, and the positive predictive value and negative predictive value were 83% and 91%, respectively. In contrast, if the ESR was less than 30 mm/h and the CRP less than 10 mg/dL, the specificity for asepsis was 100%. The value of the ESR and CRP has been reported by other investigators. Alternative biomarkers for diagnosis of prosthetic joint infection are under investigation, including interleukin-6, synovial CRP, and synovial alpha-defensin.
Blood cultures (two sets) should be performed in patients with systemic symptoms including fever, acute onset of symptoms, or if a concomitant infection is present that would make the presence of a bloodstream infection more likely. The presence of bacteremia can aid in the identification of the offending pathogen to tailor antibiotic therapy, and may also change the clinical management of the patient.
Aspiration of the hip should be performed if prosthetic joint infection is suspected and one or both of the inflammatory markers are elevated. The aspiration should be performed using strict aseptic technique in a clinic setting or intraoperatively just before incision of the joint capsule. The synovial fluid should be sent for cell count and differential, and aerobic and anaerobic cultures. Additional cultures for atypical causes of infection (acid-fast bacilli, fungi, and so forth) should not be obtained routinely; however, these may be of value in certain patient populations. The synovial WBC count should be interpreted in reference to the time from prosthesis implantation. The absolute number of WBCs that correlate with a prosthetic joint infection and the percent of WBCs that are present that are polymorphonuclear cells (PMNs) are reported to range from 1700 cells/mL to approximately 4200 cells/mL if the joint is more than 6 months postoperative. A patient who is less than 6 months from surgery and is suspected of having a prosthetic joint infection generally has a higher number of WBCs present. The percent of PMN cells present in the synovial fluid differential is also helpful to aid in the diagnosis. A value of greater than 80% has been shown to indicate the presence of infection. Schinsky and colleagues also demonstrated that in the presence of elevated ESR and CRP, the optimal cut-point for prosthetic hip infection was a synovial fluid WBC count of greater than 3000 cells/mL. Synovial fluid WBC counts have been shown to be variable in failed metal-on-metal hip implants, making interpretation of synovial fluid analysis difficult in this patient population.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





