CHAPTER 18 Correction of Mal-United Intra-Articular Distal Radius Fractures with an Inside-Out Osteotomy Technique
Rationale and Basic Science Pertinent to the Procedure
The benefits of early correction of mal–united extra–articular distal radius fractures are well known.1 Obviously, when the mal–union affects also the joint surface the altered mechanics2 will lead to rapid radiocarpal osteoarthritis in young active individuals.3–5 Although this articular disruption calls for immediate correction, there are just a few papers that deal with the problem.4,6–8 Recently, Ring et al.8 reported good results by using a direct open approach. The technique is difficult, however, and there is a risk of causing additional damage due to the limited access to the joint space through a capsulotomy incision. Furthermore, devascularization of the fracture fragments due to detachment from their soft–tissue attachments is possible.
We have performed an open osteototomy for correction of mal–united intra–articular distal radius fractures several times. We have been limited to performing relatively simple osteotomies (i.e., single longitudinal or coronal osteotomy, or simple transverse) due to the previously described difficulties. Our main concern, however, was the difficulty in visualizing the articular reduction. In effect, once the mal–united fragment was reduced (elevated) the narrow radiocarpal space prevented an adequate assessment of the joint congruity without extreme manipulation of the wrist. The surgeon must solely rely on fluoroscopy to assess the reduction, even though fluoroscopy has been shown to be unreliable with regard to evaluating any articular gap or step–off under the best of circumstances.9
Inspired by the experience with laparoscopy, in which carbon dioxide is used in place of fluid—and by the invaluable informal comments by other colleagues who were performing parts of arthroscopic ganglion resection without fluid irrigation (personal communication, doctors Atzei and Luchetti of Italy and doctors Zaidemberg and Perotto of Argentina)—we were inspired to perform wrist arthroscopy without infusing fluid (i.e., the dry technique).10 This proved to be crucial to the execution of the technique described in this chapter. An intra–articular inside–out osteotomy11 of distal radius mal–unions hinges on use of the “dry” arthroscopic technique, which is therefore also presented in detail (along with some technical tips).
Contraindications
There are no absolute contraindications to this technique, provided the cartilage is not worn out.11 We have no experience with osteotomies older than three months. It is possible that the presence of cartilage degeneration or arthrofibrosis might impede the arthroscopic procedure, but we have no data to support or refute this. A loss of articular cartilage would preclude this operation, in which case we would then opt for an osteochondral graft12 or a partial wrist arthrodesis.13,14 We would therefore recommend a diagnostic arthroscopy in cases older than three months prior to proceeding with an osteotomy.
Surgical Technique
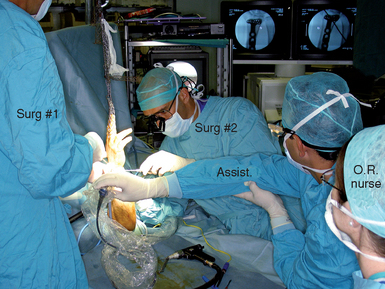
The surgical technique is similar to a standard wrist arthroscopy save that irrigation fluid is not used during the procedure. It is of note, however, that this technique is more cumbersome and complicated than the average wrist arthroscopy. First, it requires an open exposure of the distal radius for plate fixation of the fragments in addition to the arthroscopic–assisted osteotomy. Second, it requires alternating the hand from a suspended position to flat on the operating table. Third, fluoroscopy is used periodically during the procedure—which is facilitated by placing the hand flat. The osteotomes and probes used need to be sturdier than the average arthroscopic instruments (Figure 18.1).
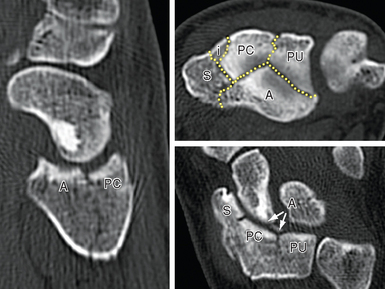
Finally, the assistance of another experienced surgeon is integral to the procedure (Figure 18.2). It is important that everyone on the surgical team be prepared and familiar with their assigned role in order to minimize operating time. It is helpful for the surgeon to preplan the osteotomies beforehand based on a review of the preoperative X–rays and if possible of the original fracture films. The author has found a good–quality preoperative CT scan to be invaluable, since the intraoperative view of the joint can be quite confusing due to the disruption (Figure 18.3).
The hand is then placed on traction from a bow with a custom–made system that allows one to easily change the hand from a horizontal to a vertical position while maintaining a sterile field.11 The standard 3−/,4 and 6–R portals are developed. Transverse 1–cm skin incisions are preferred on the dorsum of the wrist because they heal with a minimal scar. To avoid lacerating any nerve or tendon, a superficial skin incision is made with a #15 blade. A hemostat is used to widen the portal to permit the smooth entrance of the osteotomes and other necessary instruments (Figure 18.1). Apart from dorsal portals, a volar radial (VR) portal is always used. If a Henry incision is planned, the portal is developed as recommended by Levy and Glickel.15 Otherwise, we follow the technique of Doi et al. or of Slutsky16,17 (Figure 18.4). The quality of the articular cartilage over the adjacent scaphoid and lunate is assessed along with exploration of the midcarpal joint if there is any doubt as to the integrity of the interosseous ligaments.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree