The objective of containment treatment in Perthes disease is to hold the femoral head in the acetabulum during the period of “biologic plasticity” while necrotic bone is resorbed and living bone is restored through the process of “creeping substitution.” This article identifies the various methods of containment and the technical aspects of each method. Choice of method depends on the experience of the surgeon and the psychosocial needs of the patient and family. Failure is more commonly a result of inappropriate patient selection for a particular method, delay in management, or technical errors rather than to the method that was selected.
The objective of containment treatment in Perthes disease is to hold the femoral head in the acetabulum during the period of “biologic plasticity” while necrotic bone is resorbed and living bone is restored through the process of “creeping substitution.” This prevents lateral migration of the femoral head and thereby avoids flattening while the necrotic bone is being replaced with living bone. To be successful, it is best to initiate containment while the femoral head is still round. This is during the period of preventive intervention that was identified in the preceding article on principles of containment treatment elsewhere in this issue. During the late fragmentation stage, containment may not be possible because of hinged abduction. Hinge abduction in the fragmentation stage requires different strategies for treatment other than containment. Also, containment is no longer beneficial after the fragmentation stage, or when the femoral head is already enlarged, partially healed, and permanently deformed.
The dilemma in Perthes disease is that some patients do not require treatment, but outcomes are better when the decision to treat is made early in the course of the disorder. During these early stages it is difficult to classify the severity of involvement by current systems of classification.
Age at onset
For clarity of definition, two issues should be emphasized. First, it should be noted that it is the age at onset of symptoms that is to be taken into consideration and not the age at presentation to the surgeon. Second, chronologic age has been used in almost all natural history studies and this sometimes causes confusion. A child who has had his eighth birthday is older than 8 years of age and can also be considered younger than 9 years of age. This is similar to the description of a 2-month old infant who would be considered older than zero but younger than 1 year of age. After the first birthday he or she will be older than 1 year but younger than 2 years.
The child’s age at onset of symptoms can provide guidance to initial planning in many cases. Long-term studies indicate that untreated children 9 years and older at onset of symptoms have a poor prognosis regardless of extent of involvement of the capital femoral epiphysis. Also, before lateral pillar collapse, children 8 years and older (or with bone age older than 6 years in boys) have improved outcomes following surgical intervention compared with nonoperative treatments. Children younger than 5 years at onset have a low risk of early osteoarthritis. Some children in this age group do develop poor radiographic outcomes, but the prognosis is similar whether these younger children are treated by observation or by surgical containment. Growth disturbances rather than femoral head collapse may contribute to some of these poor results in younger children, but growth disturbance may not be influenced by containment. Therefore, children younger than 5 years rarely benefit from treatment other than brief limitation of activities for symptomatic management. Children between 5 and 8 years at onset should be contained early in the course of disease when the extent of femoral head involvement is clearly greater than 50% (Catterall 3–4). Other cases in the 5- to 8-year age group may be observed to determine whether the hip will spontaneously remain contained or whether lateral migration (eccentration) develops.
Lateral migration
Lateral migration is associated with poor outcomes. For this reason, the authors recommend containment between the ages of 5 and 8 years as soon as lateral migration is identified. When early lateral migration is identified in this age group, containment is advisable before development of femoral head deformity and hinge abduction. For patients 8 years or older at onset of symptoms, containment is recommended as soon as the diagnosis is confirmed rather than waiting for signs of lateral migration, because the prognosis is poor for children in this age group.
Lateral migration
Lateral migration is associated with poor outcomes. For this reason, the authors recommend containment between the ages of 5 and 8 years as soon as lateral migration is identified. When early lateral migration is identified in this age group, containment is advisable before development of femoral head deformity and hinge abduction. For patients 8 years or older at onset of symptoms, containment is recommended as soon as the diagnosis is confirmed rather than waiting for signs of lateral migration, because the prognosis is poor for children in this age group.
Methods of containment
It is our opinion that all forms of containment can be successful when containment is initiated early in the course of disease and the principles of that particular method of containment are followed appropriately. There are advantages and disadvantages of almost all forms of containment. When a method of containment is selected for an individual patient, it is generally best to stay with that method rather than changing later in the course of disease. Some of the current literature includes outcomes of containment methods that were selected after the initial method of containment failed. This article identifies the various methods of containment and the technical aspects of each method. Choice of method depends on the experience of the surgeon and the psychosocial needs of the patient and family. Failure is more commonly a result of inappropriate patient selection for a particular method, delay in management, or technical errors rather than to the method that was selected.
Bed Rest and Range of Motion Treatment
Bed rest and physiotherapy can improve range of motion in most patients. However, this is considered noncontainment treatment and has not improved outcomes. Treatment to restore range of motion without containment surgery has been less successful than containment surgery in children 8 years and older. Terjesen and colleagues considered treatment with bed rest and range of motion to represent the natural history of untreated Legg-Calvé-Perthes disease. Decreased hip motion early in the course of disease is generally caused by muscle, owing to the subchondral fracture. In later stages, deformity of the femoral head or true muscle contracture may limit movement. Thus, limitation of motion before femoral head deformity may represent a symptom of severity rather than a cause of pathologic progression.
Pain relief by bed rest may reduce muscle spasm, but does little to prevent deformity of the femoral head. Successful range of motion treatment may indicate milder Perthes disease, especially in younger children. Failed range of motion treatment may indicate more severe Perthes disease with persistent muscle spasm and subsequent femoral head deformity. Thus, physical therapy and bed rest may select only the milder cases whereas moderate to severe patients are subjected to delayed containment treatment. Bed rest and range of motion therapy may help relieve symptoms in preparation for containment treatment, but the authors do not recommend bed rest and physical therapy as a form of definitive treatment for Perthes disease.
Containment by Casts and Bracing
The outcomes of Petrie casts and bracing combined with limited ambulation have been successful when used for prolonged periods. Containment can be achieved by nonoperative methods when the braces or casts include the thigh and leg with hip abduction and moderate internal rotation. This must be maintained until the fragmentation stage is complete, all necrotic bone has been resorbed, and there is early subchondral bone formation. The time for this to occur is 12 to 18 months from onset of symptoms depending on the age of the child. One advantage of this method is that hospitalization is not required. The major disadvantage is the limited mobility and prolonged treatment time.
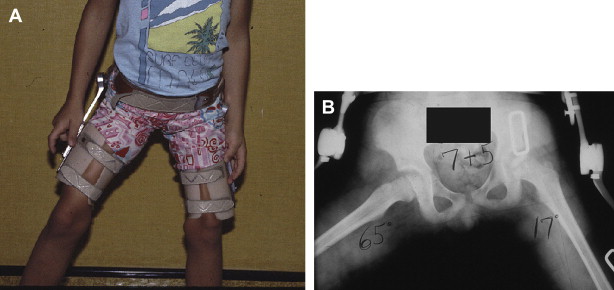
Petrie casts or a custom lower extremity A-frame orthotic can hold the lower extremities in wide abduction and slight internal rotation with the knees slightly flexed ( Fig. 1 ). These can be removed for bathing, but can also be removed inappropriately by the patient. Limited ambulation may be possible when the knees are included for proper containment, but community mobility requires a wheelchair with removable side arms. Tilting the lower extremities is necessary to enter standard doorways. This lengthy treatment is difficult in a mobile society when both parents may be working outside the home and patients are no longer admitted to pediatric rehabilitation hospitals for treatment of Perthes disease. Another disadvantage is that patients may become noncompliant and then choose surgery in later stages of femoral head collapse when surgical containment may be less successful.

Ambulatory brace treatment for Perthes disease has declined in use for a number of reasons. Primarily, the outcomes of ambulatory bracing have been inferior to surgical containment for patients older than 8 years at onset. Reasons for inferior outcomes may include noncompliance during prolonged brace treatment, braces that fail to control abduction, or concerns about behavioral sequelae ( Fig. 2 ). The Atlanta Scottish Rite abduction orthosis and weight-relieving abduction braces have largely been abandoned because studies have shown little improvement compared with the natural history of Perthes disease. Weight-relieving braces that do not contain the hip may promote subluxation and increase pressure on the lateral aspect of the femoral head.
For children younger than 8 years at onset, the outcomes of brace treatment and surgical containment are approximately equal. Before the age of 5 years, treatment may not influence outcome. For children aged 6 to 8 years, Herring and colleagues reported a slight trend toward improved outcomes of bracing and surgery compared with no treatment, but this difference was not statistically significant. There was no difference in the 6-year to 8-year age group between treatment with braces or surgery.
Restoration of range of motion is necessary before a brace or cast can be expected to contain the hip in Perthes disease. Petrie casts can be applied in the clinic with gradually increasing abduction. It is recommended that casts be removed every 6 to 8 weeks for 24 to 48 hours to restore range of motion to the knees before another cast is applied. Alternatively, traction with bed rest or with slings and springs may be used to restore motion. Oral anti-inflammatory medications may also be helpful, but the role of physical therapy is questionable. After range of motion has been restored, full-time bracing is required except for bathing purposes. This must be continued for 12 to 18 months until all dense, necrotic bone has been resorbed. This indicates the end of the fragmentation stage and beginning of re-ossification. It is safe to discontinue bracing at this stage even though the femoral head is not fully re-ossified.
In summary, it is the authors’ opinion that cast and brace treatment may improve outcomes in the age group of 5 to 8 years at time of onset. The method should include restoration of motion followed by immobilization of the leg, knee, and thigh in abduction with limited weight bearing. This should be continued for approximately 12 to 18 months. It is not recommended to attempt this form of containment with the intention of performing surgery if braces or casts fail. That would delay definitive containment until later stages when any method of containment would be less effective.
Containment by Proximal Femoral Varus Osteotomy
There have been numerous reports of containment by proximal femoral varus osteotomy since Axer reported this method in 1965. When compared with the Salter and other rotational pelvic osteotomies, the outcomes are approximately equal. Both procedures should be performed in the early stages of disease but the rotational pelvic osteotomies require a spherical femoral head and full range of motion preoperatively. The proximal femoral varus osteotomy may be less suitable for children 9 years and older because remodeling is unreliable.
Proximal femoral varus osteotomy can be performed when range of motion is moderately restricted because it shortens the femur, reduces joint reaction forces, and medializes the direction of those forces. Another advantage of femoral varus osteotomy is that it is a familiar procedure for most pediatric orthopedic surgeons. Abnormal venous congestion in the proximal femur is relieved by proximal femoral osteotomy, but the effect on rate of healing of the femoral head may be variable. Joseph and colleagues noted acceleration of healing when proximal femoral varus osteotomy was performed early in the course of disease.
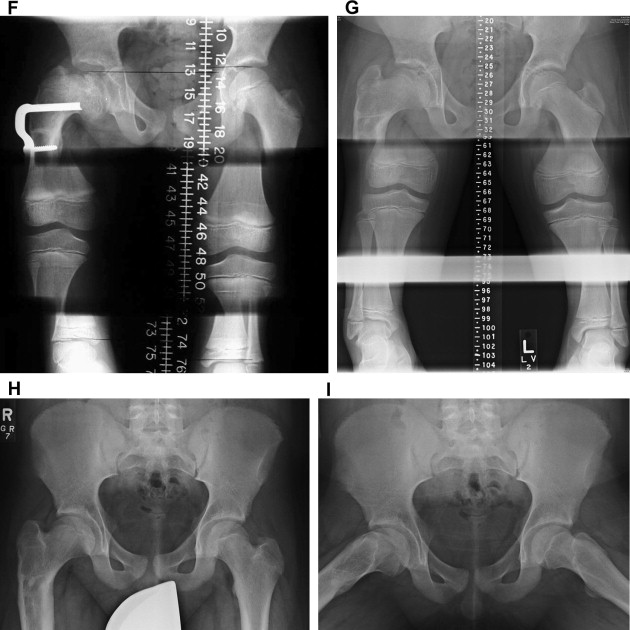
The major disadvantage of proximal femoral varus osteotomy is the potential for residual shortening with coxa brevis and trochanteric prominence. This is more likely to occur when the patient is 8 years or older. Abductor limp and femoral shortening in the early postoperative period may cause concern for parents. However, these resolve in most patients because of remodeling and growth stimulation ( Fig. 3 ). Growth disturbance of the femoral neck in Perthes disease is the most likely cause of persistent coxa brevis instead of inadequate remodeling in children younger than 8 years. When a Salter osteotomy or shelf procedure is performed, shortening and trochanteric prominence are uncommon. This may be because proximal femoral varus osteotomy creates varus and shortening that are more problematic when growth disturbances develop. Attention to technical details and appropriate selection of patients can minimize the risks of shortening and coxa vara.

The authors consider proximal femoral varus osteotomy a useful form of containment for children who meet the criteria for containment, as previously noted. The major technical considerations are to restore at least 30° of abduction in extension before surgery, and to preserve a neck-shaft angle of 110° with the desired neck-shaft angle being approximately 115°.
Additional technical considerations include the following:
- 1.
Perform no more than 20° of varus. Kim and colleagues noted that 15° of varus is sufficient.
- 2.
Perform opening wedge osteotomy to reduce limb length discrepancy.
- 3.
Add approximately 15° of extension to the osteotomy to help contain the anterior aspect of the femoral head and to reduce the flexion effect caused by the oblique plane osteotomy.
- 4.
Do not derotate the femur because this leads to an externally rotated gait similar to a femur fracture that heals in an externally rotated position.
- 5.
Medially translate the distal fragment to avoid developmental genu valgum. To do this properly, a fixation implant that allows medialization of the femoral shaft should be used.
- 6.
Perform trochanteric apophysiodesis to reduce trochanteric prominence.
- 7.
When the patient is 8 years or older and 20° of varus is required to contain the hip, then consider a limited amount of varus combined with a Salter osteotomy, pelvic rotational osteotomy, or shelf procedure to provide additional containment. Combined osteotomies will avoid remodeling concerns in the older child. Triple innominate osteotomy may provide greater containment of the femoral head than Salter innominate osteotomy.
- 8.
Postoperative immobilization may be unnecessary if excellent range of motion is restored before surgery. When the osteotomy is performed without preliminary restoration of motion, postoperative immobilization in a spica cast is recommended for 4 to 6 weeks to allow resolution of muscle spasm.
- 9.
Avoid excessive abduction in a postoperative cast (if used) because this may contribute to avascular necrosis and growth disturbance.
Containment by Salter Osteotomy
The Salter osteotomy is a transverse osteotomy of the pelvis along a line from the sciatic notch to just above the anterior inferior iliac spine. The acetabulum is then rotated laterally and anteriorly using the pubic symphysis as a hinge. This improves anterolateral coverage of the femoral head in the area most commonly affected in Perthes disease. The rotation of the osteotomy also displaces the acetabulum medially and increases the lever arm of the abductor muscles, thereby reducing the abductor force required to stabilize the hip.
Salter reported improved outcomes following this osteotomy for Perthes disease compared with a group of similar untreated control patients. Other investigators have also reported improved outcomes following a Salter osteotomy. Investigators who compared innominate osteotomy to proximal femoral osteotomy found similar outcomes when appropriate treatment principles were followed.
The authors consider the Salter osteotomy a useful form of containment for Perthes disease when patients are properly selected and the procedure is performed correctly. The most important considerations are to perform the procedure while the femoral head is round or almost round and to obtain a full or almost full range of motion before surgery. Stevens and colleagues advised that the osteotomy should be performed within 8 months of onset of symptoms. When a 30° wedge of bone is inserted anterolaterally, the anterior coverage of the femoral head can be improved by approximately 25° and lateral coverage of the femoral head by approximately 15°.
Additional technical considerations include the following:
- 1.
Residual contractures of the adductor muscle are released by subcutaneous tenotomy.
- 2.
An essential component of the procedure is to release the tendinous portion of the psoas muscle at the pelvic brim.
- 3.
The proximal or iliac segment should be stabilized so the movement occurs through the acetabular segment by rotation at the symphysis pubis.
- 4.
The osteotomy should remain closed posteriorly.
- 5.
Placing the involved lower extremity in the position can facilitate opening the osteotomy site in the correct orientation.
- 6.
The distal fragment should be displaced anteriorly approximately 1.0 to 1.5 cm to allow maximum pubic symphysis rotation and provide anterior coverage of the femoral head.
- 7.
A triangle of bone approximately 30° to 35° in shape is secured in the osteotomy site with 2 to 3 large threaded Steinmann pins.
- 8.
The Steinmann pins should be large enough to provide stability and avoid breakage.
- 9.
A postoperative cast is not required when the child is 6 years or older and can cooperate with toe-touch weight bearing for 4 to 6 weeks postoperatively.
- 10.
The Steinmann pins are removed 8 to 10 weeks postoperatively.
Containment by Shelf Procedures
Shelf acetabuloplasty is a procedure where the margin of the acetabulum is extended to provide more coverage for the femoral head. This increases the weight-bearing surface of the anterior, lateral, and/or posterior portions of the acetabulum. Shelf procedures do not change the orientation of the acetabulum so there is no change in the biomechanics of the hip except for the increased distribution of forces from the enlarged surface area. The Chiari osteotomy has some similarity to shelf procedures because it also increases the area of support for the femoral head. However, the Chiari osteotomy displaces the hip medially and superiorly and reduces the compression forces acting across the hip joint. The interposed capsule undergoes fibrous metaplasia and transforms into fibrocartilaginous tissue. Although the Chiari osteotomy has been used for containment to prevent femoral head deformation, it has primarily been recommended as a salvage procedure for advanced Perthes disease when the femoral head is extruded or incongruent.
Several investigators have reported improved outcomes with containment by shelf acetabuloplasty. Improved outcomes have also been reported with shelf acetabuloplasty for more advanced cases of Perthes disease with containable subluxation, and in patients 9 years and older. One advantage of the shelf acetabuloplasty is preservation of limb length without excessive trochanteric prominence. Another advantage is long-term improved coverage of the enlarged femoral head that develops following Perthes disease. In children 8 years and older at time of shelf acetabuloplasty, the shelf is gradually incorporated into the growing pelvis without restricting range of motion at skeletal maturity. This procedure can also be performed in children as young as 5 years without interfering with growth of the lateral acetabular margin.
The authors consider shelf acetabuloplasty a useful form of containment for Perthes disease when patients are properly selected and the procedure is performed correctly. The bone graft should be placed in close contact with the joint capsule with sufficient autologous bone graft to buttress the extended margin of the acetabulum. The authors prefer the slotted acetabular augmentation described by Staheli and Chew. In this procedure, the reflected head of the rectus femoris is dissected and left attached posteriorly. The capsule is thinned and cleared of all tissue. Using radiographic imaging, a narrow slot is created just proximal to the labrum. This slot is expanded anterolaterally and posterolaterally and then deepened in an oblique upward direction of approximately 15°. The cortical strips from the iliac crest are inserted into the slot. A properly developed slot will firmly hold the strips in place directly against the hip capsule and protrude far enough to establish a center-edge angle of approximately 45°. The reflected head of the rectus femoris is sutured over the top of the cortical strips to hold them firmly against the hip capsule. The outer table of the ilium is elevated proximal to the slot without damaging the slot. Copious cancellous bone is packed against the lateral ilium proximal to the cortical strips that form the shelf. This provides a buttress of bone to support the shelf. A postoperative spica cast is not always necessary if the graft is secure and the child is cooperative with toe-touch weight bearing.
Additional technical considerations include the following:
- 1.
Place the graft near the joint line but above the growth area of the labral rim. Superiorly placed grafts tend to resorb.
- 2.
Avoid penetration of the joint while preparing the slot. A sufficiently oblique upward angle will prevent this and also ensure proper positioning of the cortical strips.
- 3.
The breadth of the slot from anterior to posterior should follow the curve of the capsule and should be sufficiently long to provide anterior, posterior, and lateral coverage.
Containment by the Triple Pelvic Osteotomy
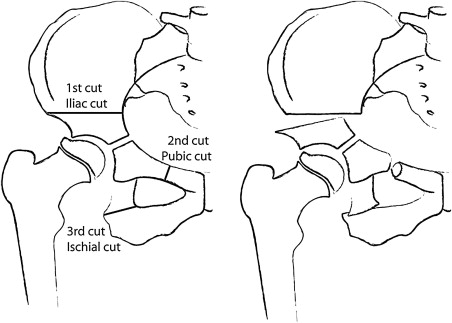
The triple pelvic osteotomy combines the transverse osteotomy of Salter with complete osteotomies of the superior pubic ramus and ischium ( Fig. 4 ). This allows greater mobility of the acetabulum without interfering with growth of the triradiate cartilage. When a section of bone is removed from the ischium, or when the ischial and pubic osteotomies are close to the acetabulum, the acetabular fragment can be medialized to reduce the joint reaction forces.