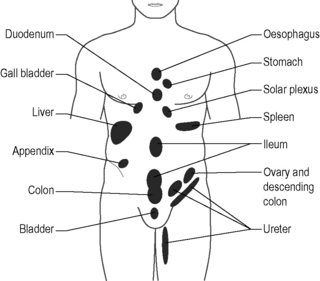
7.6 Connective tissue manipulation Loose connective tissue contributes to superficial and deep fascia, the intermuscular septa. It surrounds blood vessels and nerves, and provides a framework for most organs. It is the layer of tissue between the skin and the muscle, and has also been referred to as connective tissue proper (Ebner 1975). More recently, this tissue has been termed areolar connective tissue (Langevin et al. 2009). In addition to binding structures and holding them in their anatomical spaces, areolar connective tissue stores fat and helps the body conserve heat. The matrix of areolar connective tissue aids in tissue repair by depositing collagenous fibers and forming scar tissue. Finally, nutrients travel from the blood vessels through this tissue to individual cells as well as carrying metabolites away from the cells towards the blood and lymph vessels. The structure of connective tissue is physiologically dependent upon vascularity and blood supply, and is influenced by suprarenal hormones. The fibroblasts and the mast cells in connective tissue have an inverse relationship with suprarenal cortical hormones. That is, a decrease in secretion of these hormones will result in an increase in fibroblastic and mast cell activity, resulting in a water-retaining effect on the tissues (Ebner 1975; Holey 1995). When connective tissue becomes dysfunctional, the problems that arise are in proportion to the support the tissues provide when they are healthy. Several different terms have been used to describe connective tissue restrictions and/or dysfunction. According to Maigne (1995) cellulagia is defined as: ‘neurotrophic manifestations that include subcutaneous tenderness and thickening.’ It can be detected by using the ‘pinch-roll’ test, in which a fold of skin is rolled between the fingers causing pain, with the clinician noting thickening. Ebner (1975) used the term trophic edema to describe thickened hypersensitive loose connective tissue. The terms panniculosis and fibrositis have also been used to describe dysfunctional connective tissue (Travell & Simons 1993; Kotarinos 2008) involving inflammatory hyperplasia of the white fibrous tissue. This chapter uses the term subcutaneous panniculosis to describe thickened connective tissue that is sensitive upon pinch rolling (i.e. dysfunctional connective tissue). In addition to presenting as thickened or dense upon skin rolling, areas of subcutaneous panniculosis may show vasomotor, pilomotor, and sudomotor reactions, increased subcutaneous fluid, and atrophy or hypertrophy of the underlying muscles (Chaitow 1988). Underlying muscle atrophy is the resultant effect of the thickened tissue interfering with proper functioning of sodium–potassium pumping mechanisms in muscles (Ebner 1975). Panniculosis can cause local nociceptive pain via the peripheral nervous system, and it is hypothesized to cause referred pain in distant locations through the central nervous system (Bischof & Elmiger 1963; Fitzgerald & Kotarinos 2003). Several mechanisms have been identified to explain how dysfunction develops in the subcutaneous tissue. These are as the result of visceral referred pain, in tissue superficial to myofascial trigger points, in the cutaneous distribution of inflamed peripheral nerves, and superficial to areas of joint dysfunction. The viscerosomatic reflex is a reflex in which somatic manifestations occur in response to visceral disturbances. More specifically, the visceral–cutaneous reflex is a phenomenon where disturbances or disease in visceral organs refer pain along the distribution of somatic nerves which share the same spinal segment as the sensory sympathetic fibers to the organ affected (Head 1893; Janig 1996). The visceral–cutaneous reflexes have been studied by many and are commonly referred to as Head’s zones, Chapman’s reflexes, or Mackenzie’s zones (Fig. 7.6.1). The reflex is initiated by afferent impulses from visceral receptors, then impulses travel to the dorsal horn of the spinal cord, synapse with interconnecting neurons, and connect with sympathetic and peripheral motor efferents, resulting in sensory changes in the blood vessels and skin (and also muscle and viscera) (Bischof & Elmiger 1963; Arendt-Nielsen et al. 2008). If the pathological visceral afferent stimulation becomes chronic, neurogenic plasma extravasation will occur in the skin, thereby causing vasoconstriction in the periphery, hyperesthesia, and thixotropic changes. In more recent literature, three plausible neural mechanisms have been identified in animal models to explain visceral–cutaneous reflexes. Takahashi (1996) noted that plasma extravasation occurred as a result of antidromic stimulation of C-fibers in spinal nerves. It is noted that with unilateral stimulation changes in the skin can occur unilaterally or bilaterally. Studies suggest that the actual mechanism may be a combination of the three described processes, as noted by Wesselmann and Lai (1997). One potential mechanism is described because dichotomizing sensory neurons have a branch to both the uterus and to the skin. Uterine inflammation could cause excitation of the visceral branch of the afferent neuron, leading to antidromic activation of the somatic branch, causing neurogenic plasma extravasation. Wesselmann also hypothesized that visceral afferent neurons may excite cutaneous afferent neurons. The result of this spinal mechanism is antidromic activation of cutaneous afferent fibers, again resulting in plasma extravasation. It was suggested that the sympathetic postganglionic nerve terminals must be intact, demonstrated by a decrease in plasma extravasation when the anterior spinal root was not intact (Wesselmann & Lai 1997). Similarly, basic science studies (Beal 1985) have shown that somatic disturbances cause visceral changes, otherwise known as the somatovisceral reflex (Sato 1995). Travell and Simons (1993) reported a strong association between active myofascial trigger points and subcutaneous connective tissue restrictions. Dermographia/fibrositis commonly occurs most often over muscles of the back of the neck, shoulders and torso, and less frequently over limb muscles. In panniculosis, the subcutaneous tissue exhibits increased viscosity suggestive of thixotropy. Travell and Simons proposed that the connective tissue restrictions may be related to sympathetic nervous system activity involving mechanisms operating in the underlying myofascial trigger points. Treating the panniculosis can relieve myofascial trigger point activity and/or make the underlying myofascial trigger point more responsive to treatment. Travell and Simons identified the need for designed studies to evaluate the relationship between myofascial trigger point activity and overlying panniculosis. The ‘pinch-roll’ test (of the subcutaneous tissue in the territory of a peripheral nerve) is commonly accepted as a clinical indicator of inflamed neural tissue. Referred pain is accompanied by hyperalgesia of the skin and subcutaneous tissues in the involved dermatomes. This hyperalgesia or hypersensitivity can be revealed by gently grasping a fold of skin between the thumbs and forefingers, lifting it away from the trunk and rolling the subcutaneous surface against itself in a pinch and roll fashion. The entire dermatome may be affected, or only partial tissue changes may be noted (Maigne 1996; Beco 2004). Robert Maigne coined the term ‘cellulagia’ when reporting that intervertebral joint dysfunction causes neurotrophic reflexes. Cellulagia can occur in the skin innervated by the corresponding nerve roots and in tissue superficial to areas of vertebral dysfunction (Maigne 1996). Connective tissue manipulation results in both local mechanical effects and hypothesized reflexive effects. The mechanical effects of the manual therapy technique include vasodilation, improved tissue mobility, decreased nocigenic chemicals, autonomic reactions (favorable and unfavorable), decreased hyperalgesia and improved tissue integrity (Holey 1995). Reflexively, it has been proposed that CTM stimulates a response in the sympathetic terminal reticulum in the skin. The impulse is then carried through the autonomic nervous system (ANS), through the sympathetic trunk and spinal cord, down the efferent autonomic root cells, to the segmental sympathetic ganglion or neighbor, and the diseased organ (Ebner 1975).
Viscerosomatic reflex
Superficial to muscles with myofascial trigger points
Dermatomes of inflamed neural structures
Superficial to areas of joint dysfunction
Physiology of connective tissue manipulation (CTM)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree