Congenital Knee Dislocation
Charles E. Johnston II
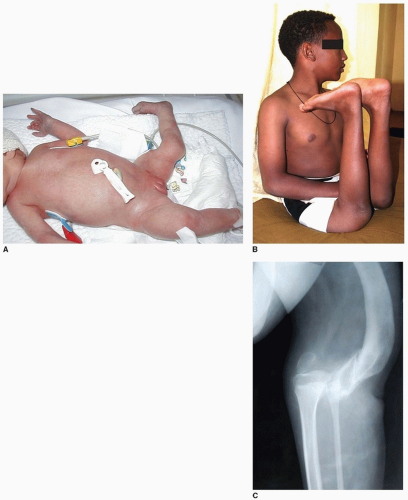
Few orthopedic deformities present with such obvious and dramatic abnormality as congenital dislocation of the knee (CDK). The newborn nursery may request an evaluation for an infant with “the knee on backward” (Fig. 34-1A), while a neglected case may have to ambulate on all fours due to fixed hyperextension of the knees, which can approach 90 degrees (Fig. 34-1B, C). The deformity is rare, being only 1/100 as common as congenital hip dislocation, but CDH as well as ipsilateral foot deformity are well documented to occur simultaneously with CDK (Fig. 34-2).
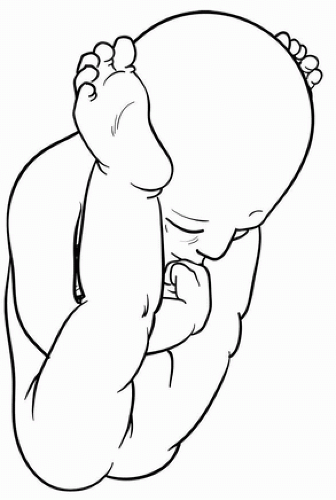
Associated chromosomal abnormalities and laxity syndromes, such as Larsen, Beals, or Ehlers-Danlos syndrome, are common. Underlying neurologic conditions such as arthrogryposis or spinal dysraphism can be seen with CDK, implicating a lack of fetal movement due to paralysis or myofibrosis as an etiology. Quadriceps fibrosis and atrophy, the major obstacles to a well-functioning knee in a more severe CDK, are characteristic. In the absence of an obvious neuromuscular condition, abnormal in utero position of the extremities, with the hip hyperflexed and the knee hyperextended and unable to flex, may be noted prenatally on ultrasound (Fig. 34-3).
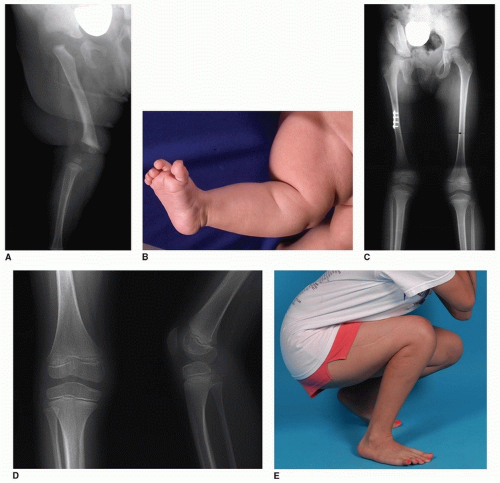
Although the knee may be stiff and impossible to flex, ligamentous laxity is well known as a paradoxical feature accompanying CDK and is responsible for the long-term instability and disability from this condition, though such laxity is frequently underappreciated. Insufficiency of the anterior cruciate ligament (ACL) due to elongation or congenital absence is typical of bilateral syndromic CDK and should be addressed as part of the comprehensive surgical management (see below). Isolated or unilateral CDK (with or without ipsilateral CDH) is more stable following reduction, with an ACL that is present and functional, leading to the designation of “stiff” CDK for the unilateral, teratologic variety (Fig. 34-2), as opposed to the “lax” bilateral syndromic variety. The latter are more easily reduced but often have debilitating instability, which heretofore has been probably undertreated.
INDICATIONS AND PREOPERATIVE PLANNING
Surgical treatment—open reduction of the knee with femoral shortening—is indicated for cases that do not respond to nonoperative techniques. Previously advocated for infants as young as 6 months of age, surgery should be delayed until such time as the surgeon feels the femur is robust enough to achieve meaningful internal fixation of a shortening osteotomy. In bilateral cases, procedures should probably be staged for reasons of anesthesia time and blood loss in very young children. Knees responding to conservative measures to obtain reduction may still require operative stabilization for recurrent instability/subluxation secondary to hyperlaxity.
At presentation, the degree of passive flexion of the knee should be noted, and it may be immediately apparent that the condition is relatively mild when the knee can be flexed and reduced with gentle stretching of the quadriceps. Contracture is assessed by applying gentle traction to the tibia and attempting to flex the knee. Concentric reduction can be deduced if the tibia will engage the distal femur and translate posteriorly with traction and flexion, and the sense of a stable articulation is palpated. In simple hyperextension deformity (grade 1), treatment by knee manipulation and flexion, maintained by a long-leg cast or splint, is sufficient. Conversely, an unstable articulation prevents any concentric flexion of the knee; the tibia will subluxate laterally and proximally on the
distal femur as more vigorous flexion is attempted, indicating irreducibility and a grade 3 dislocation (Fig. 34-4). Fibrosis and shortening of the quadriceps mechanism are easily palpated in the irreducible deformity. Other findings in irreducible CDK include obliteration of the suprapatellar pouch and contracture or fixation of the iliotibial (IT) band and hamstring tendons, which are subluxated and bowstrung anterior to the femoral condyles.
distal femur as more vigorous flexion is attempted, indicating irreducibility and a grade 3 dislocation (Fig. 34-4). Fibrosis and shortening of the quadriceps mechanism are easily palpated in the irreducible deformity. Other findings in irreducible CDK include obliteration of the suprapatellar pouch and contracture or fixation of the iliotibial (IT) band and hamstring tendons, which are subluxated and bowstrung anterior to the femoral condyles.
Historically, the treatment of an irreducible CDK included a V-Y quadricepsplasty to lengthen the contracted quadriceps mechanism, along with mobilization of other periarticular shortened
structures (IT band, hamstrings) permitting knee flexion and reduction (1). A description of this method can be found in the previous edition of this monograph (2). This approach is no longer recommended as the extensive soft-tissue dissection of the quadriceps mechanism leads to further scarring/fibrosis of the muscle, which in turn leads to progressive extension contracture, redislocation, and weakness. In addition, acute knee flexion intraoperatively produces extreme tension over the anterior knee and patellar surface, leading to skin necrosis and wound dehiscence, or else the acceptance of less than desirable degree of flexion permitting less tenuous wound closure. Last but not least, no attempt to perform posterior capsulorrhaphy is contemplated in the traditional approach, which in the laxity/syndromic cases especially is a serious oversight. Open reduction of a congenital hip dislocation would never omit a formal capsulorrhaphy—why should a congenital knee dislocation due to hyperlaxity syndromes be treated any differently?
structures (IT band, hamstrings) permitting knee flexion and reduction (1). A description of this method can be found in the previous edition of this monograph (2). This approach is no longer recommended as the extensive soft-tissue dissection of the quadriceps mechanism leads to further scarring/fibrosis of the muscle, which in turn leads to progressive extension contracture, redislocation, and weakness. In addition, acute knee flexion intraoperatively produces extreme tension over the anterior knee and patellar surface, leading to skin necrosis and wound dehiscence, or else the acceptance of less than desirable degree of flexion permitting less tenuous wound closure. Last but not least, no attempt to perform posterior capsulorrhaphy is contemplated in the traditional approach, which in the laxity/syndromic cases especially is a serious oversight. Open reduction of a congenital hip dislocation would never omit a formal capsulorrhaphy—why should a congenital knee dislocation due to hyperlaxity syndromes be treated any differently?
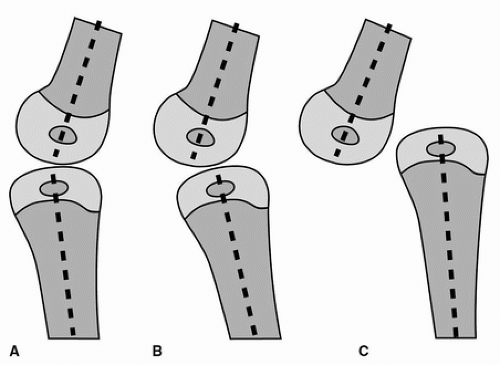 FIGURE 34-4 Classification of CDK. A. Grade 1, hyperextension. B. Grade 2, subluxation. C. Grade 3, irreducible dislocation. |
To avoid complications and poor functional outcome from the V-Y quadricepsplasty, femoral shortening with more limited arthrotomy and posterior capsulorrhaphy is now the recommended procedure (discussed below), assuming that nonoperative management fails.
NONOPERATIVE TREATMENT
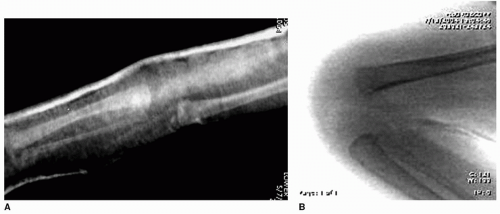
Nonoperative treatment should begin as soon as possible in infancy and is appropriate up to 12 months of age. A manipulative technique that combines manual traction on the tibia and gentle flexion of the knee is begun, with the position maintained by an anterior plaster slab from the groin to the dorsum of the foot. Such a slab is actually easier to apply and maintain with good coaptation than is a long-leg cast in an infant. Forceful manipulation is contraindicated to avoid pressure necrosis or fracture separation of the cartilaginous epiphyses. If trained physical therapists
are available, serial manipulations with splinting in increased flexion can be performed daily until the knee will flex beyond 90 degrees. Radiographic confirmation of the reduction is mandatory (Fig. 34-5). Once the knee can be flexed to 90 degrees, a plastic splint can maintain this position and be removed for range of motion exercises. If the patient has ipsilateral CDH, once the knee can be reduced to such a position, a Pavlik harness can be applied to treat the hip dislocation while simultaneously maintaining the knee reduction.
are available, serial manipulations with splinting in increased flexion can be performed daily until the knee will flex beyond 90 degrees. Radiographic confirmation of the reduction is mandatory (Fig. 34-5). Once the knee can be flexed to 90 degrees, a plastic splint can maintain this position and be removed for range of motion exercises. If the patient has ipsilateral CDH, once the knee can be reduced to such a position, a Pavlik harness can be applied to treat the hip dislocation while simultaneously maintaining the knee reduction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree