Complications of musculoskeletal trauma are distressingly common. Some complications are a consequence of the injury itself and may be unavoidable, whereas others are iatrogenic and potentially preventable. Regardless of the etiology of the complication, prompt recognition and appropriate treatment lessen the impact of the complication and improve the outcome.
I. SYSTEMIC INFLAMMATORY RESPONSE SYNDROME
A. Systemic inflammatory response syndrome (SIRS) is a condition occurring after trauma or sepsis characterized by multiple organ dysfunction and appears to be mediated by the acute inflammatory response. The magnitude of SIRS is correlated with the severity of injury, as well as the magnitude of surgery performed in the first 2 days after injury.1 SIRS is mediated by proinflammatory cytokines released by damaged tissue. Although the degree of the inflammatory response is generally proportionate to the amount of trauma, genetic susceptibility to an exaggerated response has been shown to be present in patients with a specific single nucleotide polymorphism.2 SIRS has many manifestations ranging from occult hypoxemia due to mild pulmonary dysfunction to fatal multiorgan dysfunction (MOD).3 SIRS is diagnosed when two or more of the following four criteria are present (SIRS score)4:
- Body temperature is below 36°C or greater than 38°C.
- Pulse is greater than 90 beats per minute.
- Respiratory rate is greater than 20 breaths per minute; or arterial partial pressure of carbon dioxide is less than 4.3 kPa (32 mm Hg).
- White blood cell count is less than 4,000 cells per mm3 (4 × 109 cells per L) or greater than 12,000 cells per mm3 (12 × 109 cells per L); or the presence of greater than 10% immature neutrophils (band forms).
Fat embolism syndrome (FES) and the adult respiratory distress syndrome (ARDS) are other clinical manifestations of similar phenomenon that are related to SIRS. FES may be one of the etiologic factors contributing to SIRS, whereas ARDS is now recognized as the “final common pathway” of the pulmonary consequences of SIRS. FES is generally a self-limited pulmonary disease that usually occurs within 3 days of a fracture. The diagnosis of FES is suspected if the following symptoms and signs are present in a patient with a fracture5–7:
- Disturbances of consciousness (i.e., confusion, delirium, coma)
- Tachycardia and dyspnea
- History of hypovolemic shock
- Petechial hemorrhages
Any combination of the above symptoms may be present in patients with isolated or multiple fractures. Patients with major long bone fractures are particularly at risk and should be monitored for occult hypoxemia with continuous, noninvasive pulse oximetry.8 When hypoxia is documented, supplemental oxygen is provided. Patients with hypoxia should be evaluated for coagulopathy and monitored for pulmonary, renal, and hepatic dysfunction that may develop in full-blown SIRS.
Patients presenting with signs and symptoms of SIRS are generally not considered to be candidates for immediate stabilization of their orthopaedic injuries. Instead, in these circumstances, “damage-control” methods are employed to provide provisional stabilization of fractures, with a delay of definitive fixation until the patient is considered physiologically stable. A more detailed discussion of this topic is given in Chapter 2.
B. Pertinent laboratory findings
- Thrombocytopenia (platelet count <150,000) and hypoxemia (arterial oxygen tension [PaO2] <60 mm Hg) are the most clinically useful diagnostic tests. Hypoxemia itself is very common in trauma patients and may or may not suggest pulmonary compromise.8 Elevated interleukin 6 (IL-6) levels are associated with SIRS, and this is a useful marker to follow in patients with multiple injuries.9 Patients with multiple injuries and elevated IL-6 levels seem to be at increased risk for complications following surgery, and when possible, nonemergent orthopaedic procedures should be deferred until the abnormal systemic inflammatory response has resolved.3
- Electrocardiographic changes may be present and include tachycardia, a prominent S wave on lead I, a prominent Q wave on lead II, a shift in the transition zone to the left, arrhythmias, inverted T waves, depressed RST segments, and a right bundle branch block. Serial electrocardiograms are useful.
- Increased serum lipase is indicative of FES, but is of little practical value because of the impact of blunt trauma on this laboratory parameter.
- Chest roentgenographic changes, when present, are patchy pulmonary infiltrates. The clinical manifestations of fat embolism usually precede these changes. The pulmonary findings become more severe in those patients who meet the criteria for ARDS.
C. Recommended treatment
- Respiratory support is the cornerstone of prevention and treatment of SIRS, ARDS, FES, and MOD. It is provided to keep the PaO2 between 50 and 100 mm Hg. Patients with ARDS and MOD usually need prolonged ventilatory support with continuous positive airway pressure. Renal dialysis may be necessary in the MOD group. In patients with isolated fractures who are physiologically stable, early (within 24 hours) fixation of femur fractures helps limit the incidence of this complication.7,10 Guidelines supporting early fracture fixation include normalization of base deficit, coagulation function, and absence of evidence of SIRS.11
- Shock is treated as outlined in Chapter 2, I.A.3.
- Coagulopathy is monitored and treated with fresh frozen plasma and/or cryoprecipitate. Platelet counts should ideally be maintained above 50,000 per mL.
II. NERVE COMPRESSION SYNDROMES
A. Acute carpal tunnel syndrome (CTS, median nerve entrapment at the wrist)
- The diagnosis of chronic CTS is suspected with a history of pain, tingling, and numbness in the first three digits; the symptoms are usually worse at night. Acute CTS can occur following distal radial fracture or carpal fracture/dislocation. When occurring as a complication of trauma, the condition may develop and progress rapidly. Acute CTS must be recognized and treated emergently, first with fracture or dislocation reduction and then with carpal tunnel release if symptoms do not immediately resolve (see Chapter 21).
B. Ulnar nerve compression at the elbow (“tardy” ulnar nerve palsy, acute ulnar palsy) is commonly associated with fractures and dislocations about the elbow in children as well as adults. Acute ulnar neuropathy following injury is most often the result of iatrogenic damage such as injury occurring during pinning of a supracondylar fracture in a child, or retraction during internal fixation of a distal humerus fracture in an adult.
- An early diagnostic sign is the inability to separate the fingers (interosseous weakness). There is usually decreased sensation in the fourth and fifth fingers. Light pressure on the cubital tunnel may reproduce the pain. Nerve conduction studies show a slowing of the ulnar nerve conduction velocity as it crosses the elbow (see Appendix F). However, this test is not useful diagnostically until at least 3 weeks after injury.
- If symptoms are minimal, ulnar nerve compression is managed with observation and passive range of motion of the fingers. Surgical therapy consists of exploration, neurolysis, and possible transposition of the ulnar nerve beneath the flexor muscle mass anterior to the medial epicondyle when the pattern of injury or fracture permits. This treatment usually stops any progressive neuropathy but does not guarantee complete regression of the neurologic symptoms or signs.
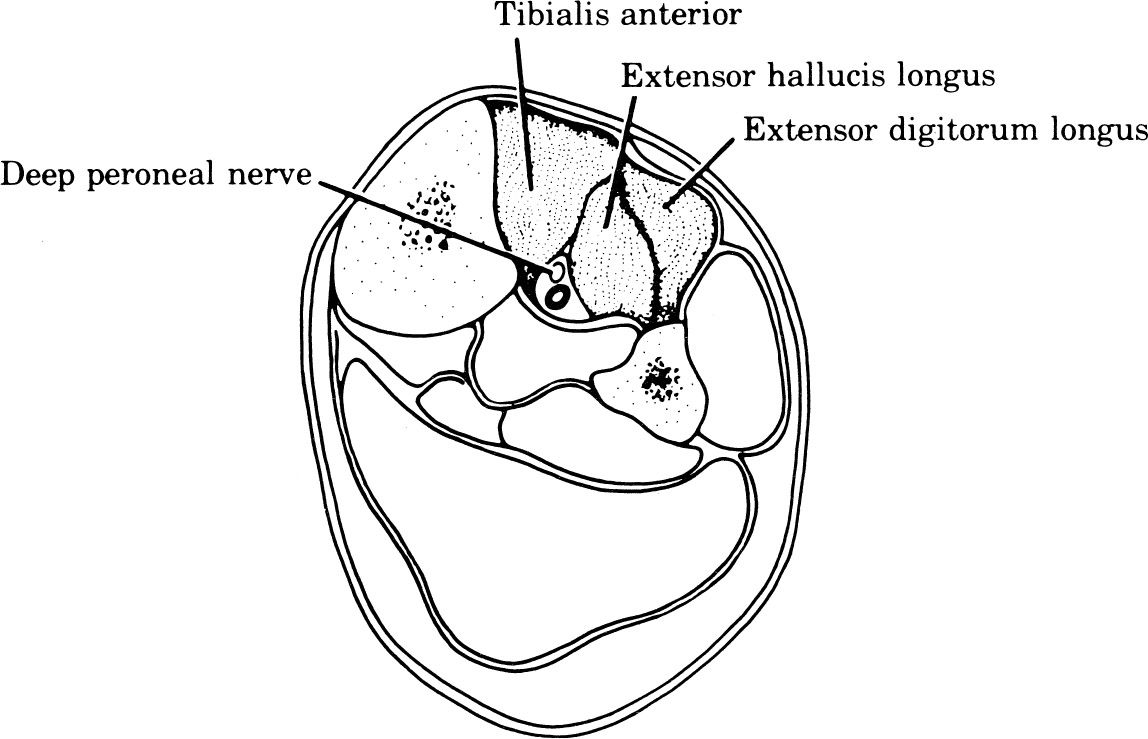
C. Peroneal nerve palsy may be due to the compression of the common peroneal nerve in the area of the fibular head or as the nerve enters the anterior compartment. Apparent peroneal palsy may also be a manifestation of more proximal injury to the peroneal division of the sciatic nerve. Thus peroneal palsy may be a complication of hip or pelvic fracture/dislocation.
- Diagnosis is often based on the motor loss, which includes weakness of dorsiflexion of the ankle and toes as well as eversion of the foot. History of a hip, tibia, ankle, or foot injury is likely. Pain is usually on the lateral aspect of the leg and dorsal aspect of the foot. Pressure over the nerve trunk may cause local pain as well as radiation into the sensory distribution of the nerve. Pressure over the nerve as it courses around the proximal fibula results from patient positioning in the operating room or intensive care unit or from poorly applied splints.
- Treatment. Associated hip, knee, or ankle dislocations are emergently reduced. If there is an operable cause, neurolysis is indicated. During the recovery stage, a lateral shoe wedge or plastic ankle-foot orthosis maintains eversion of the foot. Tendon transfer may be appropriate for some patients with a permanent foot drop.
D. Sciatic nerve neuropraxia can accompany hip dislocation or fracture dislocation (acetabular fracture). Note that some sciatic palsies may present as an isolated peroneal palsy, as discussed above.
- The main differentiating factor in the diagnosis of a sciatic neuropathy is an L5 or S1 root injury resulting from pelvic or spine fracture. A sciatic neuropathy must be suspected when multiple neurologic (L5–S3) segments are involved. A helpful differentiating test is straight-leg raising just short of discomfort; pain caused by a sciatic neuropathy is increased by internal rotation and relieved by external rotation of the hips. This reaction is not seen with lumbar radiculopathies.
- Treatment is aimed at the cause of the sciatic neuropathy, and the neuropathy itself is treated with observation. If the sciatic nerve is known to be damaged and is not improving, neurolysis may be indicated. In general, the tibial portion of the nerve recovers well, but the peroneal portion does not.12 This may be related to the fact that it is the peroneal portion that lies against the pelvis as it exits through the greater sciatic foramen.
III. COMPARTMENT SYNDROMES. A compartment syndrome is defined as “a condition in which increased pressure within a space compromises the circulation to the contents of that space.”13 Although most commonly applied to the osteomyofascial compartments of the extremities, compartment syndrome can occur in the abdomen and in major muscle groups about the spine and pelvis. Other terms that have been used to describe compartment syndrome are Volkmann ischemia, local ischemia, traumatic tension in muscles, impending ischemic contracture, exercise ischemia, exercise myopathy, anterior tibial syndrome, medial tibial syndrome, rhabdomyolysis, and calf hypertension. Compartment syndrome following trauma is most common in men under the age of 35 with fractures of the tibia or forearm.14
A. Locations
1. In the upper extremity, typical locations include the volar and dorsal compartments of the forearm (Fig. 3-1).There are also several intrinsic compartments of the hand.
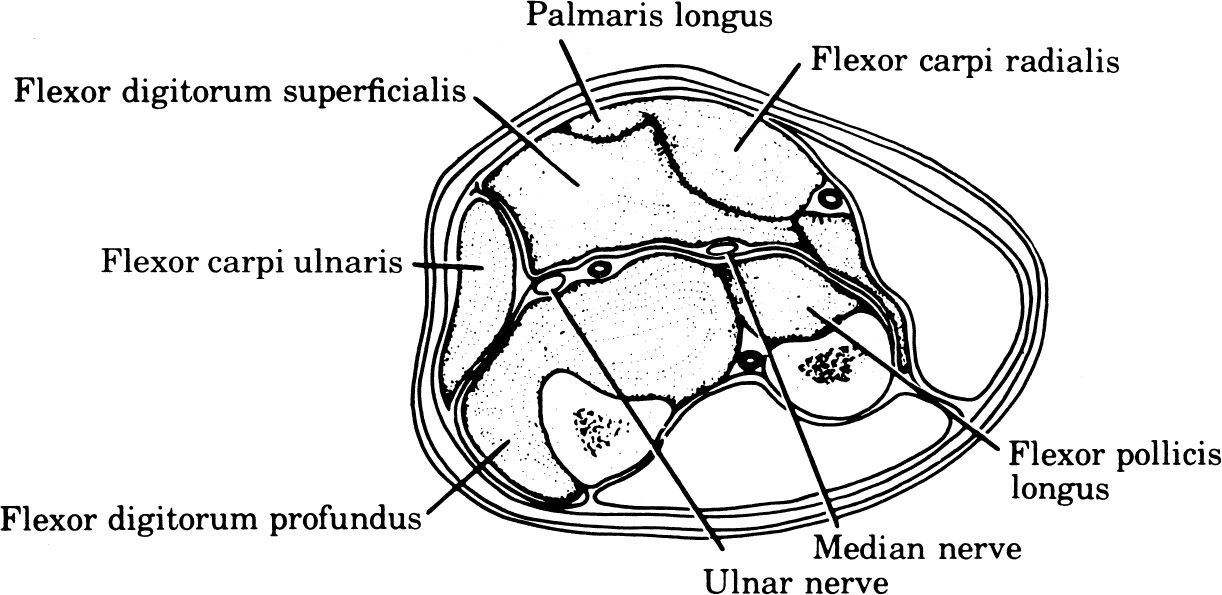
Figure 3-1. Volar compartment syndrome of the forearm. Symptoms and signs of weakness of finger and wrist flexion, pain on finger and wrist extension, hypesthesia of the volar aspect of the fingers, and tenseness of the volar forearm fascia.
2. In the lower extremity, typical locations include the anterior, lateral, superficial posterior (gastrocnemius, soleus), and deep posterior compartments of the leg (Figs. 3-2 and 3-3). Compartment syndromes are also seen in the thigh, arm, buttocks (gluteal), and foot compartments.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








