(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
A prospective registration of 1,300 patients demonstrated a low complication rate of 3.5 % for the dorsiflexion method for anterior ankle arthroscopy. This compares favorably to other methods. The historical approach of using routine distraction is not only unnecessary, but it is related with a higher complication rate. It should be considered a method from the past. When it comes to posterior ankle arthroscopy by means of the two-portal hindfoot approach, it was shown to be safe with a complication rate comparing favorable to that of anterior ankle arthroscopy.
Ankle arthroscopy is a safe method with a low complication rate.
The historical approach of using routine distraction must be considered a method of the past.
Introduction and changing of instruments in the dorsiflexed position is the main reason for the low complication rate related to this technique.
5.1 Introduction
In the field of minimal invasive foot and ankle surgery, significant progress has been made over the last 25 years. Arthroscopy of the ankle joint has become an important diagnostic and therapeutic tool for the detection and management of posttraumatic and chronic problems. Although the anatomy of the ankle is rather complex, ankle arthroscopy is generally perceived as “no problem surgery.” The procedure allows direct visualization of all intracapsular structures resulting in decreased morbidity and rapid rehabilitation when compared to arthrotomy or a medial malleolar osteotomy (Van Dijk and Van Bergen 2008).
Up to 1984, the ankle joint was found difficult to approach by means of an arthroscope. Burman even found the ankle joint unsuitable for arthroscopy, because of its narrow joint space and the large-sized nature of instrumentation used for the procedure (Burman 1931). The percentage of complications was high. Sprague mentioned 24.6 % complications in the pre-distraction era (Sprague et al. 1989). In 1984, routine (invasive) distraction of the ankle joint was advocated by Guhl, Martin, Barber, and others (Guhl and Schonholtz 1993; Guhl 1986, 1988; Martin et al. 1989; Barber et al. 1990; De Leeuw et al. 2010) (Fig. 5.1). The percentage of complications dropped to 13.6 % (Sprague et al. 1989). Following studies reported complication rates ranging from 7.6 to 10 % (Amendola et al. 1996; Ferkel et al. 1996, 2001; Unger et al. 2000). The average of published complication rates is 10.7 %, which indicates a significant risk of complication in ankle arthroscopy (Table 5.1). To reduce this number, a closer look at technique and procedure is required.
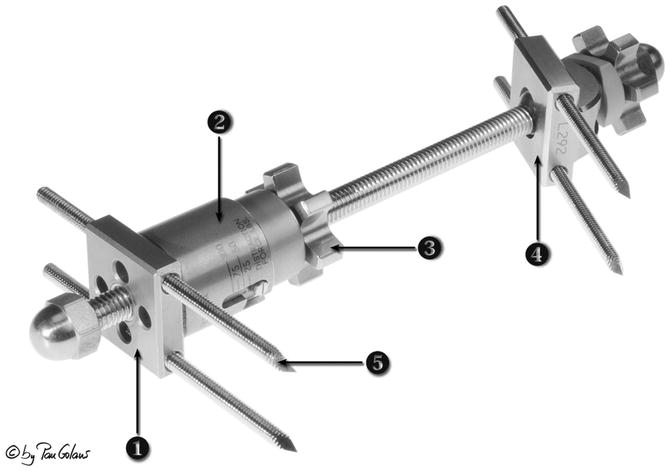
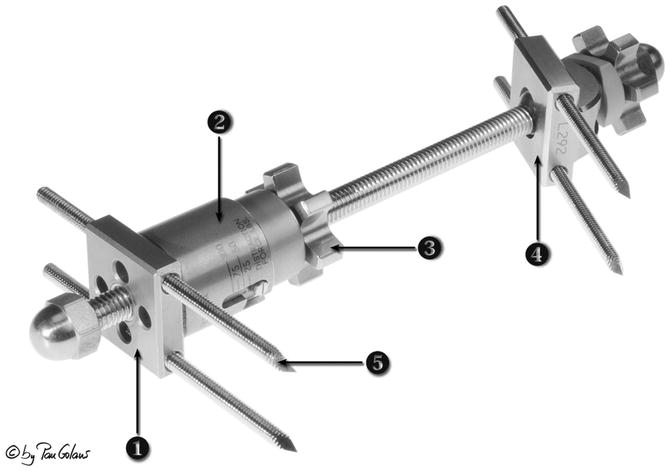
Fig. 5.1
Invasive distractor developed by James F. Guhl (1988). 1. Proximal pivot attachment. 2. Strain gauge. 3. Distraction knob. 4. Distal pivot attachment. 5. Pin (With kind permission of © Pau Golanó 2013)
Table 5.1
Summarized literature on complications in ankle arthroscopy
Author | Year | Journal | No. of patients | No. of complications | % | Neurol. | Deep infection | Superf. infection | CRPS | Instr. breakage | Sinus tract/delayed wound healing | Nerves involved |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Guhl | (1986) | Orthopedics | 62 | 5 | 8 | 1 | – | 1 | – | – | 3 | Unknown |
Guhl | (1988) | Arthroscopy | 131 | 13 | 10 | 4 | – | 2 | – | 2 | – | Sural n. 3 neuroma 1 |
Sprague et al. | (1989) | Book | 201 | 35 | 17.4 | 5 | 3 | 1 | 1 | 4 | Sural n. 3; saphenous n.1; neuroma 1 | |
Martin et al. | (1989) | Am J Sports Med | 58 | 9 | 15 | 5 | 2 | 2 | – | – | – | Unknown |
Barber et al. | (1990) | Foot Ankle | 53 | 9 | 17 | 3 | 1 | 2 | 1 | – | 2 | Superf. peroneal n. 3 |
Ferkel et al. | (1996) | Arthroscopy | 612 | 55 | 9 | 27 | 2 | 8 | 1 | 2 | 1 | Superf. peroneal n. 15; sural n. 6; saphenous n. 5; deep peroneal n. 1 |
Amendola et al. | (1996) | Arthroscopy | 79 | 6 | 7.6 | 3 | – | – | – | – | 3 | Superf. peroneal n.1; deep peroneal n. 2 |
Unger et al. | (2000) | Unfallchirurg | 155 | 14 | 9 | 3 | 3 | 2 | – | – | 4 | Superf. peroneal n. 3 |
Acta Orthop Traumatol Turc | 32 | 2 | 6 | – | – | – | 1 | 1 | – | – | ||
Foot Ankle Surg | 30 | 6 | 20 | 2 | 1 | 1 | – | – | – | Sural n. 2 | ||
J Foot Ankle Surg | 251 | 20 | 8.0 | 9 | – | 8 | – | – | – | Superficial peroneal n. 5; sural n. 1; deep peroneal n. 2; saphenous n. 1 | ||
J Bone Joint Surg | 189 | 16 | 8.5 | 7 | 1 | 1 | 2 | – | – | Tibial n. 4; sural n. 3 | ||
Total | 12 | 1,853 | 190 | 10.3 | 3.7 % | 0.6 % | 1.6 % | 0.3 % | 0.3 % | 0.9 % |
Author | Year | Journal | No. of patients | No. of complications | % | Neurol. | Deep infection | Superf. infection | CRPS | Instr. break. | Sinus tract/delayed wound healing | Nerves involved |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Zengerink and Van Dijk | (2012) | Knee Surg Sports Traumatol Arthrosc | 1,305 | 5 | 3.5 | 25 = 1.9 % | 2 = 0.15 % | 7 = 0.5 % | 1 = 0.07 % | 1 = 0.07 % | 7 = 0.5 % | Deep peroneal n. 5; sural n. 3; superficial peroneal n. 12; saphenous n. 3; tibial n. calc branch 2 |
5.2 Complications Related to Approach
Most frequent indications for anterior ankle arthroscopy involve treatment of anterior ankle impingement (bony spurs, ossicles, as well as soft tissue), osteochondral defects and loose bodies. Other indications are synovectomy, arthroscopic treatment of instability, and arthroscopic-assisted ankle arthrodesis. For treatment of posterior ankle and hindfoot problems, a two-portal approach was developed and first published in 2000 (Van Dijk et al. 2000). Indications for posterior ankle arthroscopy are treatment of posterior ankle impingement, osteochondral defects, loose bodies and ossicles, synovectomy, capsulectomy, subtalar arthrodesis and groove deepening for recurrent peroneal tendon dislocation.
Within the spectrum of complications, neurological injury is most frequently described. Nerve lesions as well as neuromas are mentioned (Sprague et al. 1989; Guhl 1986, 1988; Barber et al. 1990; Amendola et al. 1996; Ferkel et al. 1996, 2001; Freedman and Barron 1998; Takao et al. 2001). Vascular injuries and false aneurysms occur (Darwish et al. 2004; Mariani et al. 2001; O’Farrell et al. 1997; Salgado et al. 1998) (Fig. 5.1). Infections and synovial fistula have been reported (Guhl 1986, 1988; Martin et al. 1989; Barber et al. 1990; Ferkel et al. 1996, 2001; Unger et al. 2000). Complications related to invasive distraction are ligament injuries, pin tract infections, and stress fractures (Sprague et al. 1989; Ferkel et al. 1996). Furthermore, instrument breakage (Fig. 5.2), complex regional pain syndrome (CRPS), compartment syndrome, thromboembolitic complications, and painful scars have been reported (Guhl 1988; Barber et al. 1990; Unger et al. 2000). Even iatrogenic excision of the distal fibula has been described (Schmidt and Reddy 1999). The most underreported complication of all is cartilage injury, which occurs iatrogenic or during treatment for osteochondral defects.
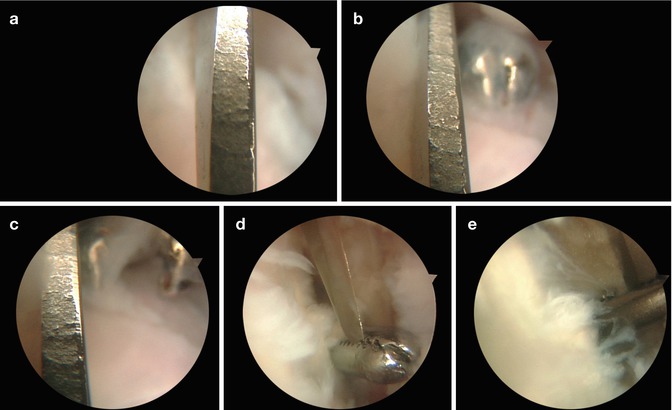
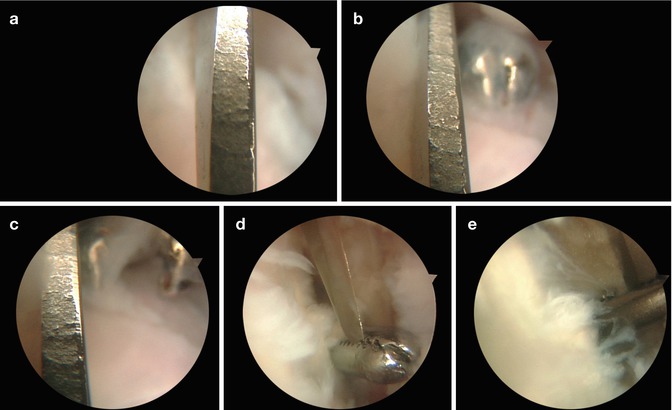
Fig. 5.2
Intra-bursal view of the retrocalcaneal space in a patient with chronic retrocalcaneal bursitis. The scope is in place through the posterolateral portal. On making the posteromedial portal, the tip of the knife has broken off. (a) Once the broken tip is recognized, “freeze” your position in order not to lose the “corpus delectum.” At this moment, do not use inflow through the scope. Using suction through the arthroscope can help. Introduce a small grasper (b, c). Grab the proximal or distal end of the broken knife. In this case the tip is captured (d, e). Grabbing the broken tip in the middle will make it difficult to remove through the portal
In the 1990s, the author developed in Amsterdam the dorsiflexion method in which the arthroscope and instruments are positioned in the “anterior working area.” Routine distraction is not used in this method but can be applied when indicated (Barber et al. 1990). We determined the complication rate for anterior ankle arthroscopy related to the dorsiflexion method for anterior ankle arthroscopy and the complications related to hindfoot endoscopy. To gain insight in the etiology of complications, we also determined the relationship between specific indications, surgical characteristics, and the number and type of complications that occurred. To answer these questions, we reviewed all ankle arthroscopies performed at our hospital since 1987 and clinically reexamined patients in which a complication had occurred. Apart from the prospective complication registration system patient records, outpatient charts and operative reports were reviewed. Patients with a complication were asked to visit our hospital for clinical examination and assessment of permanent damage (Zengerink and Van Dijk 2012).
An overall complication rate of 3.5 % in 1,305 procedures was found. In 1.9 % a neurological complication occurred (Table 5.2). All nerve injuries could be related to portal placement. Age was a significant risk factor for the occurrence of complications. Most complications were transient and resolved within six months.
Table 5.2
Patient characteristics of patients with a complication
No. | Age | Gender | Side | Daycare | Duration | FU | A/P | Indication | Treatment | Complication | Nerve involved | Residual complaints | AOFAS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 | 26 | F | R | – | 45 | 17 | A | Soft tissue impingement | Removal of ant. soft tissue | Neurological | Deep peroneal n. | + | 100 |
2 | 33 | F | L | – | 115 | 16 | A | Ant. osteochondral defect | ECD of lateral talar ocd | Neurological | Deep peroneal n. | + | 100 |
3 | 31 | F | R | – | 85 | 16 | A | Diagnostic arthroscopy | Nettoyage | Pulm. embolism | – | – | 100 |
4 | 37 | M | L | – | 90 | 16 | A | Nettoyage | Removal of osteophyte | Instrument breakage | – | LTFU | – |
5 | 31 | M | L | + | 20 | 12 | A | Osteophyte | Removal of osteophyte | Deep infection | – | – | 88 |
6 | 40 | M | L | + | 35 | 12 | A | Bony impingement | Removal of osteophyte | Superficial infection | – | – | 95 |
7 | 18 | M | L | + | 25 | 12 | A | Nettoyage | Removal of soft tissue + osteophyte | Sinus tract formation | – | LTFU | – |
8 | 46 | F
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





