Complex Open Fracture-dislocations of the Wrist
26.1 Introduction
Distal radius fractures are said to be complex in various situations: extensive articular comminution, coexistent fracture or dislocation of the ipsilateral upper extremity (e.g., associated elbow or carpal dislocation), associated regional soft tissue (including skin) or general lesions (e.g., polytrauma), or inadequate primary treatment necessitating difficult late surgery. Here we focus specifically on the management of open distal radius fractures.
26.2 Incidence and Epidemiology
Fractures of the distal radius account for up to one-sixth of all fractures seen in the emergency room. Most fractures are closed, with the exception of the Galeazzi fracture-dislocation, with the ulnar head sometimes protruding through the skin after relatively minor trauma. Open fractures, which constitute less than 4% of all distal radius fractures, may result from high-energy trauma and are then associated with a range of other various general injuries, sometimes life-threatening. In polytrauma patients, complex fracture-dislocations of the wrist are frequent but in most cases closed, while associated fractures of the humerus and forearm are commonly open. The majority of open distal radius fractures result from a penetrating injury to the wrist (e.g., from a circular saw) and are then usually associated with severe soft tissue injuries (▶ Fig. 26.1). There are few epidemiological studies on open wrist injuries, but, compared with Western countries, it is probable that the incidence of open wrist fractures is higher in low- and middle-income countries, where there are more motorbike injuries and less security in industry and agriculture.
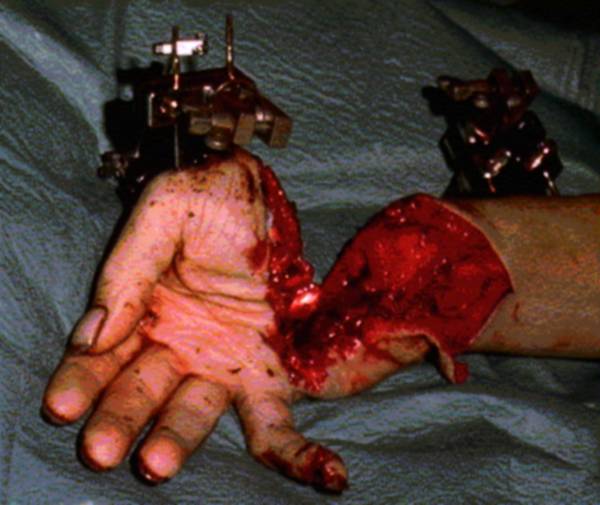
Fig. 26.1 Open wrist fracture related to circular saw injury. Note the external fixation pins and clamps already inserted.
26.3 Clinical Assessment
Polytrauma patients presenting with associated life-threatening injuries should be initially evaluated and resuscitated according to Advanced Trauma Life Support protocols. Despite a frequently dramatic clinical situation, the associated distal radius fracture should not be neglected, for the only late sequelae of the injury might well be painful functional limitations at the wrist, particularly in a manual worker.
As always, a brief medical history should be obtained, if possible from the patient, if necessary from his or her relatives or field personnel, regarding age, sex, education, work status, leisure activities, hand dominance, and existing comorbidities. It is essential to try to understand the mechanism of injury (direct blow, crush, avulsion, missile, etc.) and the type of contamination (animal bite, soil, water, etc.). Tetanus immunization status should be noted, and a booster toxoid given in case of uncertainty (frequently forgotten in polytrauma patients). The surgeon should also assess the immunological status of the patient: higher infection rates have been reported in open fractures in class B (2.9 times higher) and in class C (5.7 times higher) compromised immune system patients; similarly, there is an increased risk of deep infection in HIV-positive patients.1 It is also important to know whether the patient is a smoker, especially if microsurgical reconstructions have to be performed. Beside the risk of microvascular thrombosis, smoking has been demonstrated to impair bone healing2 and to increase the risk of chronic osteomyelitis.
The examination of the open wound should be done only in the presence of the senior hand surgeon. It is dangerous to open the dressing several times: in open fractures, this practice raises the ultimate infection rate by 3 to 4 times.3 The hand surgeon assesses the location and size of the wound, the viability of the traumatic skin flaps, and possible areas of burn. The lesions should be documented with a digital picture. Gross hemorrhage is controlled by digital pressure, avoiding blindly inserting a clamp into the wound. Areas of hypoesthesia or anesthesia are noted. The presence of foreign bodies is recorded. The hand surgeon observes the obvious deformities related to the skeletal and tendon lesions. Due to skeletal instability and pain, the function and viability of the muscle—tendon units are difficult to assess at this stage. Of particular importance, the surgeon should recognize an upper limb compartment syndrome, knowing that the presence of an open fracture does not decompress the limb compartments. In conscious patients, the diagnosis of compartment syndrome is basically clinical: intense pain, unresponsive to painkillers, and increased with passive stretching of muscles. Paresthesias, paralysis, and disappearance of distal arterial pulses are late symptoms. Diagnosis of a compartment syndrome in an unconscious or sedated patient, or in the case of sensory impairment, is challenging. Tenderness, bruising, and clinical signs of blunt, high-energy trauma to the upper extremity are key elements. A measurement of the intracompartmental pressures should be performed in every doubtful case. A differential pressure between the compartment and diastolic blood pressure less than 30 mm Hg is diagnostic. Of course, when a compartmental syndrome is diagnosed or even strongly suspected, fasciotomies must be performed immediately.
After this careful examination, the mangled extremity is covered with a sterile dressing and is not reinspected until surgery. After realignment, a temporary splint supporting the wrist is applied and radiographs are obtained. The patient is then informed of the operative plans. If amputation is considered, the patient is informed of this possibility.
26.4 Radiographic Examination
In complex injuries of the hand and fingers, a thorough preoperative radiographic examination is indispensable. At least two good-quality orthogonal radiographs should be obtained. Information concerning the complexity of the fracture, the pattern of displacement, as well as possible associated injuries to the carpus and presence of radiopaque foreign material is needed to inform decisions on management and ultimate prognosis. In complex wrist injuries, computed tomography (CT) scanning is an important tool to assess the severity of the distal radius comminution and to detect associated carpal injuries. Other investigations (sonography, magnetic resonance imaging) have limited indications in the emergency setting.
26.5 Classifications
Several types of classification are used in open distal radius fractures, based on injury severity, condition of the soft tissues, and degree of bacterial contamination, and on the characteristics of the fracture. Each classification helps in determining the optimal treatment regimen and establishing the prognosis of clinical outcome. The classifications are also helpful in clinical research, to assess the results in series of comparable patients after a given injury or a specific treatment. To improve the accuracy of each classification, the extent and severity of the injury should be reassessed during surgery, after wound exploration and debridement.
Scoring of the Injury Severity Different scoring systems have been proposed to aid the surgeon when faced with the difficult decision of amputation versus salvage (see later).
Classification Systems for Open Fractures These classification systems guide the treatment of the fracture as a function of the associated skin injury (see later).
Classifications Based on the Type of Distal Radius Fracture These classifications help the surgeon in choosing the optimal type of osteosynthesis, based on the fracture lines and severity of bone comminution. The most widely known and used are the AO, the Frykman, and the Melone classifications.
AO Classification The AO classification allows detailed anatomical categorization, especially useful in trauma registries. Although widely used in the literature, it lacks links between the description of the fracture and the clinical decision-making of fracture treatment. Furthermore, inclusion of CT scans in the diagnostic protocol has demonstrated the poor validity and interobserver reliability of this classification regarding intra-articular fractures of the distal radius.4
Frykman Classification This classification draws attention to the distal radioulnar joint (DRUJ). It also distinguishes intra-articular from extra-articular fractures; however, the classification does not differentiate between displaced and nondisplaced fractures.
Melone Classification This classification is dedicated to comminuted intra-articular fractures of the distal radius. It has gained more reliability and precision with the inclusion of CT scanning in the diagnostic armamentarium, but it does not help in classifying severely comminuted fractures with destruction of the dorsal or palmar metaphyseal buttresses of the distal radius.
Authors’ Preferred Classification System With comminuted intra-articular fractures, conventional radiography is not sufficient and CT is warranted in most cases, if the general condition of the patient permits. Until a valid CT scan-based classification system for intra-articular comminuted fractures is available, we recommend the use of the Melone classification.
26.6 Management
26.6.1 Polytraumatized Patients
A great danger in a severe polytrauma patient is being sidetracked by a visually striking, bloody, mangled extremity and not evaluating other life-threatening injuries. On the other hand, if the wrist is incorrectly treated in the emergency period, its sequelae are likely to affect the final quality of life of the patient—upper limb salvage is of course especially important in paraplegic patients. The aim of the treatment is therefore not only to save the life but also to limit residual handicaps, which are usually related to undertreated orthopedic lesions. The modern concept of treatment of a severe polytrauma is, after resuscitation, quick diagnosis of all traumatic lesions (cerebral, thoracic, abdominal, orthopedic) by CT and damage control strategy,5 reducing the second hit on the patient related to the surgery aiming at stabilizing the orthopedic lesions (the first hit being the trauma itself). This second hit is deleterious in increasing systemic inflammation and posing the risk of multiorgan failure. The damage control strategy consists of three stages: (1) the first stage consists of immediate stabilization of all unstable fractures and control of hemorrhage, in a short operative time and without additional blood loss (▶ Fig. 26.2); (2) the second stage involves resuscitation of the patient in the intensive care unit and optimization of their condition; (3) in the third stage, delayed definitive bone fixation is performed. For the management of an open wrist fracture in a severe polytrauma patient, the first stage is therefore, if the extremity is salvageable, debridement, reduction of traumatic dislocations, realignment of the wrist, and quick bone fixation, usually by radiometacarpal external fixation (▶ Fig. 26.2). The definitive bone and soft tissue reconstruction is delayed by 5 to 10 days, until the systemic inflammatory reaction has decreased. In these 5 to 10 days, however, some new surgery or debridement may be necessary, if the first debridement is insufficient. The definitive treatment can, for example, be replacement of the fixator by a volar locked plate; however, in many cases, provided that the reduction is acceptable, we retain the fixator until bone healing occurs (▶ Fig. 26.2). In each case a multidisciplinary team composed of orthopedic surgeons, trauma surgeons, and hand surgeons develops a patient-oriented plan of interventions and reconstruction, following the concept of a damage control strategy. To decrease the operative time in the first stage, it is recommended that, if possible, several teams operate on the patient at the same time (e.g., inserting a ventricular cerebral drain and simultaneously fixing the wrist). This is not always possible, and the order for orthopedic intervention is then usually first fixing the lower extremity fractures, then the pelvis, then the spine, and ending with the upper extremities.

Fig. 26.2 Road traffic polytrauma in a young adult. (a and b) Gustilo II open fracture of the distal radius and ulna and second metacarpal bone. The other major traumatic lesions affected the chest, the abdomen, the humerus, and both femurs. (c and d) A damage control strategy was instituted, with emergency stabilization of all fractures (lower limbs, humerus, and wrist/hand) using external fixation (radiometacarpal transarticular fixation for the radius, one-bone external fixation for the ulna, external minifixation for the second metacarpal). The femur external fixators were replaced by internal fixation implants 5 days later. The humerus and wrist/hand fixators were kept as definitive treatment.
26.6.2 Decision and Planning
Decision making is not easy in the emergency department. Because of pain, the initial clinical examination of the mangled extremity is difficult, even in a conscious and collaborative patient. Frequently only inappropriate radiographs are available. Thus it is often only in the operating theatre, during exploration and debridement, that the exact pattern of traumatic lesions can be precisely assessed.
Amputation Amputation of a mangled extremity is a difficult decision, but prolonged unsuccessful attempts at salvage are associated with high morbidity and are sometimes lethal. Early amputees probably have better functional scores and more satisfaction with their quality of life than do patients with delayed amputations or sometimes salvaged limbs.6 Regarding the costs, in the United States, the mean one-time and estimated 30-year prosthetic costs are respectively US $2,196 and US $21,960 for transradial amputation. Although the hospital costs for primary amputation are far less than that for limb salvage, the lifetime cost of prosthetic devices and their maintenance offset the differential.6 On the other hand, even with modern prosthetics, an amputated upper extremity has an important impact on the overall function of the patient, much greater than amputation of the lower extremity.
Because the goals and results of salvage in the upper and lower limbs are not the same, the criteria for salvage are also different. Could scoring systems guide the decision to salvage or amputate a mangled upper extremity? Indeed, several scoring systems of injury severity are available to guide the surgeon. The first scoring system, called the Mangled Extremity Syndrome Index (MESI), was proposed by Gregory et al in 1985.7 The MESI is quite complex and requires the physician to have complete knowledge of all the patient’s injuries. In addition, some of the elements of the MESI are subjective, causing a lack of inter-observer reliability. In 1990, Johansen et al proposed the Mangled Extremity Severity Score (MESS), based on four clinical criteria: skeletal and soft tissue injury, ischemia, shock, and age.8 In nearly all cases, the necessary information is available at initial evaluation. For lower extremity amputation, a value of 7 was 100% specific, and a value of 7 or more was 100% predictive.9 Slauterbeck et al used MESS in severely injured upper extremity patients; they concluded that it is an accurate objective predictor of amputation and advocated its use when deciding between amputation and salvage.10 In 1991, Russell et al proposed the Limb Salvage Index (LSI), but this very detailed score cannot be reliably used in the acute decision-making process.11 Finally, in 1994, McNamara et al modified the MESS system, separating the skeletal and soft-tissue components and adding a score for nerve injury. These changes have increased the complexity of calculating the score.9
Authors’ Preferred Severity Scoring System We believe no predictive score can be used with confidence to determine whether to amputate or to attempt to salvage a mangled upper extremity. Until more prospective validation is available, we recommend to use the MESS only as a guide to supplement the surgeon’s clinical judgment. When the affected upper limb is nonviable, when an irreparable vascular injury is present, or in the case of an extensive crush, immediate amputation is necessary. If obvious criteria for primary amputation are not met, we recommend an initial salvage attempt, observation, and subsequent early secondary amputation if unavoidable, with the risk of increased morbidity with prolonged, unsuccessful salvage attempts. Although it is important that the patient participates in the decision of secondary amputation, the surgeon should not allow the patient’s desire for limb salvage to override his or her own clinical judgment, knowing the risks associated to crush of renal insufficiency and/or infection in the early posttraumatic course, or the end result of a functionless limb.
Limb Salvage In complex open wrist fractures, the type of associated skin injury should be established. Gustilo et al made a major contribution to the management of open long bone fractures with their well-known classification, prognostic for sepsis and late amputation.12 However, their classification has poor interobserver agreement13 and is not well adapted to gunshot injuries, to open fractures with “minor” wounds but massive contamination (e.g., bites), or to hand, ankle, and foot fractures. In particular, the classification is not adapted to open metaphyseal fractures of the upper extremity, like the distal radius. The wrist is indeed not comparable to the tibia; the dimensions are different, and the wrist is better covered by soft tissue and has excellent blood supply, making it less susceptible to infection. Glueck et al found a direct correlation of deep infection with wound contamination, and no correlation with wound size or extent of soft tissue injury.14 He applied the very simple classification system proposed by Swanson et al for hand injuries and concluded that the greatest contributing factor to infection was contamination and specifically the type of contamination (▶ Table 26.1).15 Many times the skin lesion is a contusion, a crush, or a degloving; at the lower extremity, the classification of Tscherne and Oestern is more adapted to such lesions; in our knowledge, this classification has not been used in the upper extremity (▶ Table 26.2).3
Type I | Type II |
Clean | Contaminated |
Treatment < 24 h | Treatment > 24 h |
No systemic illness | Systemic illness |
Source: Reprinted from Swanson TV, Szabo RM, Anderson DD. Open hand fractures: prognosis and classification. J Hand Surg (Am). 1991;16:101–7 with permission from Elsevier. | |
Grade 0 | Closed fracture with little or no soft tissue injury (e.g., closed spiral fracture resulting from torsion) |
Grade 1 | Superficial abrasion of the skin due to fragment pressure from within (e.g., fracture-dislocation of the ankle) |
Grade 2 | Direct trauma with local contusion to skin or muscle |
Grade 3 | Severe fracture comminution with extensive skin/soft tissue contusion/crushing; possible closed degloving; possible compartment syndrome |
Source: Oestern HJ, Tscherne H. The management of open fractures. In: Tscherne H, Gotzen L, eds. Fractures with Soft Tissue Injuries. Berlin: Springer-Verlag, 1984: 10–32 with kind permission from Springer Science and Business Media. | |
Authors’ Preferred Classification System of Open Fractures Until the development of a classification system well adapted to open fractures of the distal radius, we recommend using the classification of Swanson, originally developed for open hand fractures, with an emphasis upon the type of contamination. Highly contaminated open fractures, sometimes with obvious debris (e.g., gravel) should be treated with multiple debridements as part of the initial plan, and not on the basis of subsequent development of infection.
Antibiotics in Open Fractures By definition, all open fractures are contaminated; one should therefore avoid speaking of antibioprophylaxis—the antibiotic administration is better viewed as early therapeutic. The microorganisms cultivated from the wound sometimes originate from the trauma site; more frequently, they are skin contaminants, particularly Staphylococcus aureus and S. epidermidis. Gram-negative bacteria are usually hospital-acquired (too frequent preoperative examinations of the wound, in poor hygienic conditions). When the open wrist fracture has been contaminated by soil, there is a risk of gas gangrene (Clostridium perfringens); in the case of contamination by water from rivers, the likely microorganisms are either Pseudomonas aeruginosa or Aeromonas hydrophilia. An open extremity fracture can be the origin of a life-threatening necrotizing fasciitis.
Antibiotic administration is the first step in the treatment of an open fracture of the distal radius, although this attitude is poorly documented and carries the significant risk of selecting resistant microorganisms. The current evidence-based recommendations are: (1) early antibiotherapy against gram-positive microorganisms with additional coverage of gram-negatives in Gustilo-Anderson type III open fractures (A-level recommendation); (2) in type III fractures, minimum 72 hours antibiotherapy and no longer than 24 hours after wound closure (B-level recommendation); (3) there may be a benefit from additional local antibiotic treatment (cement beads or spacers: C-level recommendation).16 Practically, the usual recommendation is to give intravenously a first-generation cephalosporin (e.g., cefazolin), which is active against gram-positive microorganisms, and an aminoglycoside (e.g., gentamicin or tobramycin), against gram-negatives. The plasma level should be monitored, particularly in the case of renal insufficiency (acute renal failure is not infrequent in polytrauma patients). Substitutes for aminoglycosides can also be used in certain cases: they include quinolones, aztreonam, and third-generation cephalosporins. Note that quinolones have been associated with inhibition of osteoblastic cell activity. Ampicillin or penicillin are chosen in conditions favoring the development of anaerobic infections (farm injuries, ischemic conditions). In case of bone loss, it is helpful to supplement the general antibiotherapy with local antibiotherapy from cement carriers (gentabeads or custom-made spacers; minigentabeads are commercially available for small bone defects such as occur at the hand and wrist).17 The antibiotics should be started as soon as possible. The duration of antibiotic administration is controversial. Dellinger et al demonstrated that a prolonged 5-day course of antibiotic administration was not superior to a one-day course.18 We empirically recommend a duration of 3 days, to be repeated at each subsequent significant surgical procedure.
26.6.3 Wound Debridement and Exploration
The adequacy of initial surgical wound debridement is the most important single factor under the surgeon’s control. The goal is to decrease the bacterial load, to eliminate the devitalized tissue, and to prevent further contamination, thereby facilitating the action of the host’s defense systems.
Timing of Wound Debridement
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








