Fig. 20.1
(a–f) Complex elbow instability (terrible triad). Conservative treatment was attempted (due to the patient’s general status). Instability recurred after hyperflexed and well-fitted cast
Surgery can consist in open reduction and internal fixation of the fractures, external fixation, exploration, and repair of the medial collateral ligament and/or lateral ulnar collateral ligament. Procedures may be performed alone or combined with each other [12, 37, 51]. Dynamic external fixation is an option that can be considered when the elbow remains unstable even after surgical treatment, allowing an early mobilization while maintaining a concentric reduction (Fig. 20.2).
Fig. 20.2
Dynamic external fixation allowing motion while maintaining a concentric reduction
We will review the specific surgical procedure, according to the injury pattern, and the reported results.
20.7 Patterns of Injury and Specific Treatment
20.7.1 Transolecranon Fracture-Dislocations
In this pattern of injury, we have type III (Mayo classification) olecranon fractures, associated with elbow instability (Fig. 20.3). These uncommon lesions often result from high-energy injuries, which forces an anterior translation of the forearm in relation to the humerus; they are often misidentified with Monteggia fracture-dislocation [32, 33, 45].
Fig. 20.3
Transolecranon fracture-dislocation
Ligaments are typically not involved, so that reduction of the ulnohumeral joint is sufficient to restore stability. The important pearls in treatment are as follows:
Stable anatomic fixation with restoration of the trochlear notch width, preferably with contoured anatomical olecranon plates
Fixation of concomitant coronoid process fracture
Preservation of the olecranon tip, even if significantly comminuted, due to the attachment of triceps
Early postoperative mobilization
20.7.2 Elbow Dislocation with Coronoid Fracture
Fractures of the coronoid process are relatively uncommon injuries occurring in approximately 2–15 % of patients with elbow dislocation [25, 52]. The coronoid process plays a key role in elbow stability. Coronoid fractures are often associated with other lesions, but their management is usually the fundamental step, defining the postoperative stability and subsequent range of motion.
The first classification system was proposed by Regan and Morrey: coronoid fractures were classified based on the amount of coronoid involved. They observed a directly proportional correlation between poorer prognosis and larger fractures [40]. However, this system does not take into account the whole injury pattern and therefore has limited value in planning operative treatment [54]. More recently, O’Driscoll described a new classification system (Fig. 20.4) that emphasizes the importance of the anteromedial facet [36, 50]. The relevance of this anatomical reference is the relationship with sublime tubercle to which the anterior band of MCL is attached [50].
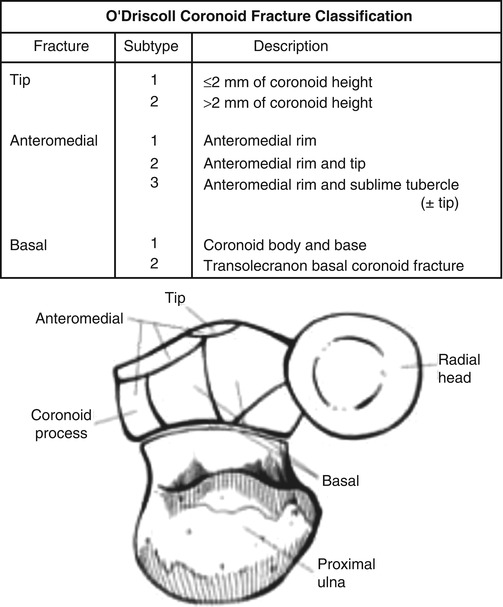
Fig. 20.4
O’Driscoll coronoid fracture classification (Printed with permission)
Coronoid tip fractures are often associated with terrible triad injuries and rarely occur in isolation [43]. However, in isolated tip fractures, some authors have suggested suture fixation [8], while others argue with biomechanical evidence suggesting that small (<10 % of coronoid height) fractures contribute very little to stability and any valgus instability should be addressed by repair of the MCL instead [5].
Doornberg and Ring reported the results of 18 patients with fracture of the anteromedial facet of the coronoid process and they observed concerns with elbow stability in the group with limited treatment of the fragment. On the other hand, the group with secure fixation had significantly better function, according to the system of Broberg and Morrey, and no signs of elbow instability were present [9].
The important pearls in treatment are as follows:
Fixation of the anteromedial facet of the coronoid (Fig. 20.5) should always be performed, even when the fracture is very small, through a medial approach.
Fig. 20.5
Anteromedial facet fracture of the coronoid
Small tip fractures (<10 %) usually does not need fixation, but when valgus instability is present, the repair of the MCL should be done.
Dynamic external fixation is an option that can be added when the elbow remains unstable.
The fixation methods should be stable enough to allow an early postoperative mobilization.
20.7.3 Elbow Dislocation with Radial Head Fracture
Isolated radial head fractures following a dislocation are relatively rare injuries [55]. Josefsson et al. [16] underlined the importance of preserving the radial head to avoid recurrent instability and posttraumatic osteoarthritis. Currently, a more aggressive approach in the treatment of the radial head fractures has been adopted, trying to stabilize them with internal fixation whenever possible. When the resection is unavoidable, because reconstruction is not possible, replacement is better achieved with the use of metallic head prosthesis [18, 23, 54]. Ring et al. suggest that open reduction and internal fixation has to be reserved for minimally comminuted fractures with three or fewer articular fragments [47].
Prostheses have certain drawbacks, such as the possibility of incorrect sizing which may result in “overstuffing” of the joint, inadvertent damage to the capitellum, and loosening. However, when the radial head is not amenable to fixation due to severe comminution, prosthetic replacement in the acute setting is recommended in order to address the underlying resultant instability [44, 54].
Some authors advocate surgical repair of the MCL when radial head is excised because the increased stability allows for early mobilization avoiding valgus instability [3, 16]. However, the ligamentous complexes, particularly the MCL, can heal in the presence of sufficient stability. If the radial head is not reconstructable and prosthesis is not readily available, then the MCL should be acutely repaired in order to restore the coronal plane stability of the elbow and to allow early mobilization [54].
The important pearls in treatment are as follows:
Internal fixation whenever possible.
Arthroscopy can help in obtaining an anatomic reduction using minimal invasive procedures.
Radial head resection without replacement is not recommended due to the associated instability risk.
If replacement is required, preference is given to metallic head implants.
In radial head replacement, correct sizing is the key point to avoid overstuffing that can subsequently wear the capitellum and to obtain a successful outcomes.
If instability is present after radial head fracture treatment, exploration and repair of the medial collateral ligament and/or lateral ulnar collateral ligament should be the next step.
20.7.4 Terrible Triad Injuries
When a dislocation of the elbow is accompanied by fractures of both the radial head and the coronoid, also associated with disruption of the MCL complex, this is known as a “terrible triad of the elbow” [46] (Fig. 20.6). The reason for this eponym are the poor outcomes usually associated with this injury, resulting from an underappreciation of the importance of preserving the radial head or from a neglected coronoid fragment [7, 39].
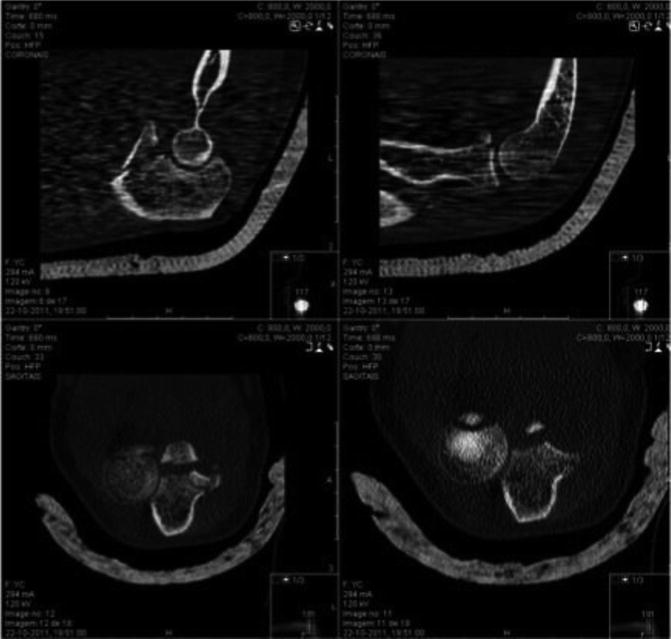
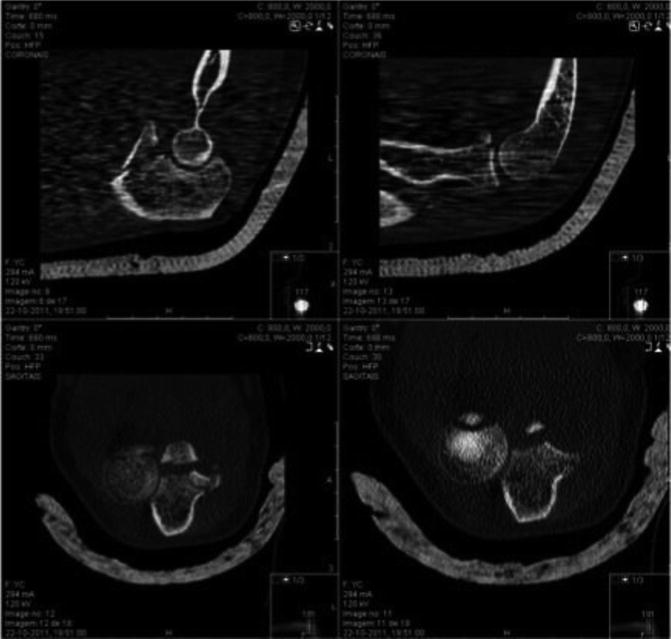
Fig. 20.6
“Elbow terrible triad”
The coronoid fracture’s height in this pattern of injury is on average 35 % of the total height and rarely above 50 % [8]. The coronoid plays a vital role as an anterior buttress and is the key point in the treatment of these lesions. Repairing even smaller coronoid fragments has shown benefit in the final result [8, 14, 39, 46].
LCL complex disruption is prevalent in terrible triad injury and its important role as a primary posterolateral stabilizer of the elbow justifies its repair [21, 39]. On the other hand, although injuries to the MCL are also very commonly associated, being present in 50–60 % of cases, they are not universally repaired [14, 15]. Some authors assert that MCL injuries tend to heal by scarring in simple elbow dislocations and the repair of articular and LCL complex injuries will effectively transform complex elbow dislocations into a simple dislocation, thereby making MCL repair unnecessary [11]. However, other authors stated that the repair of the MCL, as shown in biomechanical studies, is fundamental and that the medial approach may be beneficial to repair fractures involving the medial facet of the coronoid [13, 14, 48] (Fig. 20.7).


Fig. 20.7
Terrible triad with anteromedial facet fracture of the coronoid that was treated with a buttress plate by a medial approach
In our opinion, the MCL repair must be performed only when posteromedial or valgus instability is still present intraoperatively after fractures fixation and LUCL repair [54].
The radial head fracture is treated following the same principles stated before. The important pearls in treatment are as follows:
Repair or reconstruct the coronoid process, even when the fragment is small.
Use an additional medial approach to the repair medial facet coronoid fractures.
When disrupted, the LUCL should be repaired with transosseous sutures or with anchors.
Repair the MCL when posteromedial or valgus instability persists after fracture fixation and LUCL repair or when a medial approach is used to fix a coronoid anteromedial facet fracture.
Dynamic external fixation is an option that can be added when the elbow remains unstable.
20.8 Rehabilitation
The results of treatment after a complex elbow dislocation are not universally successful. Early mobilization is the key point, but it relies on the quality of stability achieved with the initial treatment.
Hinged elbow braces in the postoperative period can be used to give confidence to patients and to usually start an immediate and safe range of motion as defined by the surgeon; this can be increased every week while soft tissues progressively heal. However, if stability is not a concern, an early and supervised motion program, without any immobilization can give the greatest likelihood to obtain an excellent functional outcome.
Rehabilitation should be closely supervised, with an easy contact between the surgical and rehabilitation teams, and often requires a long period with multiple therapy sessions per week.
20.9 Complications
Posttraumatic stiffness is much more common than instability after a complex elbow dislocation. The likelihood of instability decreases significantly when the correct surgical treatment has been established.
Bracing and therapy are not generally useful after 1 year. So, when the functional elbow range of motion defined by Morrey [30] is compromised and does not improve with a well-designed and supervised rehabilitation program, an open or arthroscopic arthrolysis should be considered.
Heterotopic bone formation (Fig. 20.8) occurs most frequently in the neighborhood of the lateral and medial collateral ligaments but also in the anterior capsule above the coronoid process, where it can be very disabling due to the flexion compromise. Excision is performed when there is a functional compromise but is usually delayed until reactive bone has matured, generally at 1 year.










