Chapter 13 Complex Cases in Cartilage Repair
Tricks and Tips
Case 1. Medial subvastus approach to the knee
Introduction
Recently there has been an emphasis on minimally invasive and muscle-sparing approaches in orthopedic surgery. The subvastus approach to the knee joint has been described as an alternative to traditional approaches, which involve a large arthrotomy with partial division of the quadriceps mechanism. I have found the technique very useful for joint-preserving surgeries as well as prosthesis implantations when the soft tissue mobility of the extensor mechanism is supple. Careful surgical technique is pursued, as described and illustrated here.1
Surgical Technique
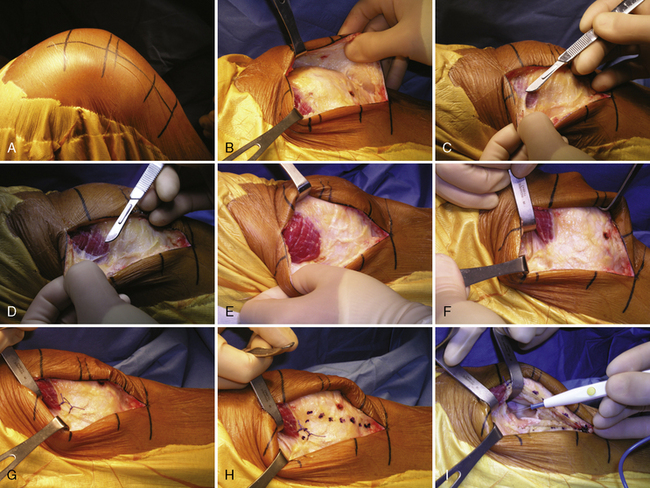
The patient is positioned supine in the standard fashion. We generally use employ a lateral post at the level of the thigh tourniquet as well as a post to support the foot, such that the knee can be flexed and maintained at 90 degrees of flexion. The skin incision can be made directly midline or slightly medial to midline, depending on the nature of the pathology. The length of the incision is based on the underlying pathology. Generally, it extends from the superior pole of the patella to the inferior aspect of the tibial tubercle (Figure 13–1A). The incision is carried sharply through the subcutaneous tissue down to the retinacular tissue. Full-thickness medial and lateral flaps are then created sharply with careful hemostasis (Figure 13–1B). The creation of large, full-thickness flaps is important because it allows the extensor mechanism to be mobilized deep to the subcutaneous tissues.
The distal insertion of the vastus medialis obliquus (VMO) on the patella is exposed (Figure 13–1C). The fascia overlying the VMO is released sharply, taking care not to injure any underlying muscle fibers (Figure 13–1D). The fascia is released posteriorly toward the attachment of the VMO on the medial intermuscular septum. This exposes the entire distal extent of the VMO (Figure 13–1E). Using blunt dissection, a finger can be placed underneath the VMO at its inferior border. The VMO is retracted proximally and laterally while maintaining its attachment to the patella. A Z-retractor is inserted anterior to the distal femur and deep to the muscle to maintain retraction (Figure 13–1F).
Two no. 1 Vicryl marking sutures are placed at the level of the VMO attachment to the patella (Figure 13–1G). An oblique capsular incision is made just distal to the VMO, beginning posteriorly at the level of the intermuscular septum and extending laterally, parallel to the inferior border of the muscle, toward the medial border of the patella. The incision is made between the marking sutures, which then serve as a guide for later repair. At the medial border of the patella, the arthrotomy is extended distally, taking care to leave a cuff of tissue attached to the patella for closure (Figure 13–1H). The arthrotomy incision is carried distally across the joint line and parallel to the medial border of the patellar tendon. Care is taken to avoid damaging the anterior horn of the medial meniscus if a biologic procedure is being performed. If necessary, the retropatellar bursa and fat pad can be incised to gain additional exposure.
Next, attention is turned to the suprapatellar pouch, where the synovial capsular attachments to the undersurface of the quadriceps tendon are released completely from medial to lateral (Figure 13–1I). This is the key maneuver that allows full mobilization of the extensor mechanism because it detaches the quadriceps muscle from the anterior femoral synovial supracondylar attachments. The patella can then be subluxed into the lateral gutter. Creating a large, full-thickness, lateral subcutaneous flap during the initial exposure is necessary in order to create a pocket into which the patella can be subluxed. A 90-degree bent Hohman or Z-retractor is placed in the lateral gutter at the level of the quadriceps tendon insertion above the patella to maintain retraction of the patella. Flexing the knee to approximately 90 degrees provides excellent exposure of the entire joint, and the appropriate procedure can be performed (Figure 13–1J). A standard closure is performed at the end of the case (Figure 13–1K). The closure is quite simple because no muscle needs to be repaired.
Discussion
The medial subvastus approach was originally described in the German literature by Erkes in 1929.2 A modified version was reintroduced by Hofman in 1991.3 A so-called “mini” subvastus approach has since been described.2,4,5 Multiple reports in the literature describe the results with respect to total knee arthroplasty. Although concerns have been raised regarding appropriate component positioning, many studies demonstrate more rapid recovery, better pain scores, less blood loss, and better short-term knee range of motion when comparing the subvastus approach to more traditional appproaches.6–12 Schroer et al13 reported their results of 600 primary total knee arthroplasties performed through a subvastus approach. Follow-up was short term, averaging 28 months. A historical group of 150 total knee arthroplasties performed through a standard medial parapatellar arthrotomy was used as a control. Overall, 11 (1.8%) major complications required reoperation in the subvastus group and 6 (4.0%) in the traditional group. The rates of both major and minor complications were found to be independent of surgical technique. The rate of major complications in the subvastus group was associated with surgical experience, as the rate was reduced by 16% for each additional 50 procedures performed. Mean knee flexion at 1 year averaged 125 degrees in the subvastus group and 114 degrees in the traditional group. Average operative time was initially higher in the subvastus group but decreased with experience so that it was less than the traditional group in the last 400 subvastus procedures performed. Of note, the authors stated that 99% of total knee arthroplasties performed during the study period were done through a subvastus approach, with 91% of patients classified as overweight and 11% as morbidly obese.
Case 2. Intraarticular osteotomy after tibial plateau fracture
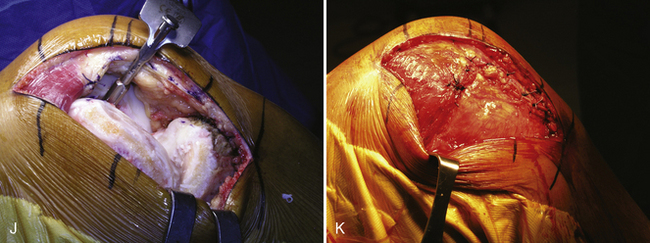
Radiographic assessment (Figure 13–2A and B) reveals she has mechanical alignment passing through the center of the lateral tibiofemoral compartment. The medial and patellofemoral compartments are intact. Joint-preserving considerations for treatment include corrective realignment osteotomy combined with intraarticular osteotomy through the fracture site versus a lateral tibial plateau allograft.
Radiographic sizing of the opposite intact uninjured knee (Figure 13–2C) allows sizing for both allograft tissue as well as the normal medial to lateral tibial plateau dimensions for restoring the opposite knee if possible through intraarticular osteotomy surgery.
Computed tomographic (CT) scan with sagittal (Figure 13–2D) and coronal (Figure 13–2E) imaging allows assessment of the size of the comminuted fracture fragments to assist in decision making of osteotomy versus allograft. Because several large articular fragments are present, it was believed that osteotomy through the old fracture site would be possible, with elevation of the articular surfaces, autologous and allogeneic bone grafting from the iliac crest, and varus-producing femoral osteotomy to unload the damaged lateral compartment.
Angular correction for the osteotomy is determined by long alignment x-ray films corresponding to an 8-degree angular correction placing the mechanical axis to the medial tibial spine. A longitudinal anterior incision is made along the lateral patellar border distally and proximally. A lateral parapatellar arthrotomy is performed to expose the lateral tibial plateau as well as the distal lateral femur (Figure 13–2F). The anterior to posterior intraarticular osteotomy is made by using small K-wires and sharp wide osteotomes along the K-wires through the prior fracture sites. The comminuted metaphyseal bone is elevated. The articular fragments are reconstructed and temporarily held with K-wires and pointed reduction forceps as the width of the tibia is measured compared to the opposite knee native tibial surface. Intraoperative fluoroscopy (Figure 13–2G) confirms an adequate reduction. Autologous bone grafting from the iliac crest to the elevated tibial plateau articular fragments is performed along with compression buttress plating. Opening wedge femoral osteotomy is performed to correct the alignment and unload the reconstructed lateral tibial plateau. Seven years postoperatively, the patient continues to have minimal or no pain, functions at a high level, and is satisfied with her reconstruction (Figure 13–2H).
Case 3. Extraarticular supracondylar femoral reverse dome osetotomy following posttraumatic deformity
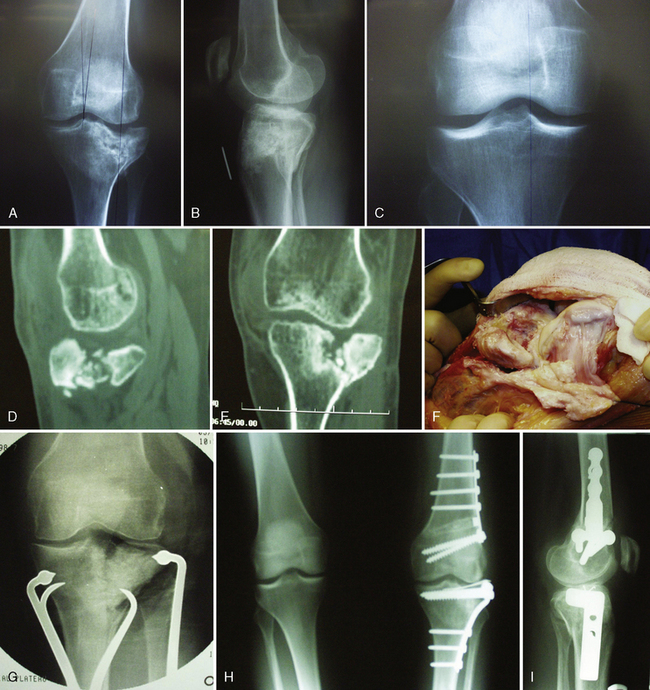
Long alignment x-ray films (Figure 13–3A) demonstrate that the mechanical axis to her right knee falls outside the medial joint space, requiring a 15-degree angular correction to bring it back to normal mechanical axis. Lateral x-ray films (Figure 13–3B and C) demonstrate that her distal femoral flexion deformity is approximately 20 degrees.