Muscle
Activation/perpetuation
Symptoms
Examination
Gastrocnemius
Muscle overload/prolonged plantar flexion
Nocturnal calf cramps
Restriction of knee extension with ankle in dorsiflexion
Soleus
Muscle overload, forefoot slipping/prolonged plantar flexion
Heel pain and tenderness
Restriction of ankle dorsiflexion with knee in flexion, Achilles reflex may be reduced
Plantaris
Muscle overload, forefoot slipping/prolonged plantar flexion
Posterior knee and upper calf pain
Restriction of ankle dorsiflexion with knee in flexion, Achilles reflex may be reduced
Popliteus
Running, twisting, or sliding with knee bent
Posterior knee pain with knee bent
Passive lateral rotation restricted by pain with thigh fixed and knee flexed at 90°
Tibialis posterior
Chronic muscle overload, jogging on uneven surfaces/prolonged hyperpronation
Pain in sole, arch, or Achilles tendon while walking or running
Functional weakness, restricted ROM, aching pain when muscle is actively retracted in fully shortened position
Long toe flexors (FHL, FDL)
Running on uneven ground/walking, running on soft sand, Morton foot structure, prolonged hyperpronation
Painful feet, especially with weight bearing
Weakness in toe flexion, restricted ROM in extension
Gastrocnemius trigger points become activated in the belly of the muscle in the center of the calf as a result of the muscle becoming strained, either as a primary event, or when a limp develops as a result of a painful disorder occurring in the heel or foot, and also when, because of a circulatory disorder, the muscle becomes ischemic. Pain from the trigger points in this muscle is felt in the calf and the sole of the foot. It is often worse when walking uphill, and may be associated with the development of nocturnal cramps, often misdiagnosed as restless leg syndrome [19]. Figure 13.1 shows the locations of the gastrocnemius trigger points.
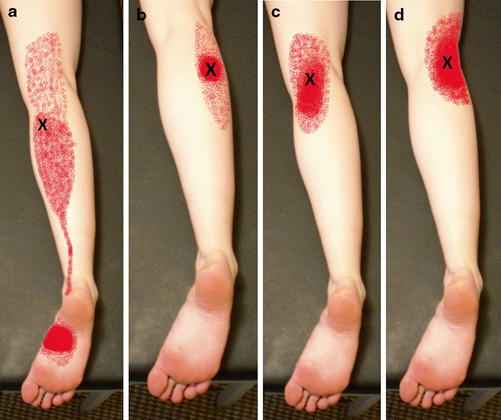
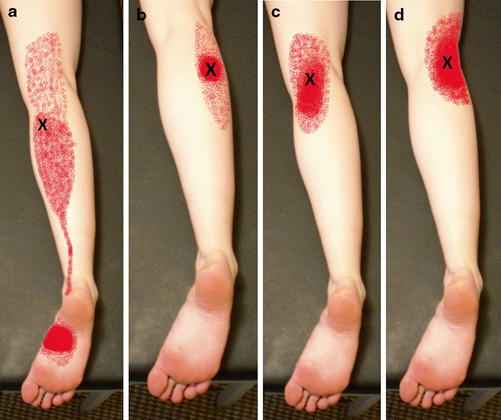
Fig. 13.1
Gastrocnemius trigger points (X) and pain referral patterns (red color). Solid color is primary site of pain, with stippling indicating the spillover pattern. a Trigger point 1, b trigger point 2, c trigger point 3, d trigger point 4
The soleus is liable to develop trigger points in its distal third for the same reasons as they develop in the gastrocnemius. Pain from these trigger points is referred distally along the Achilles tendon to the heel. The pain may also be referred upwards to the ipsilateral sacroiliac joint. The posterior part of the gluteus minimus can also refer pain to the calf, and this can activate satellite trigger points to the soleus [16]. The ankle jerk reflex may be decreased or absent in patients with trigger points in the soleus. The deactivation of the trigger points restores this reflex to normal [19]. A small study showed a significant improvement in ankle range of motion after a single intervention on latent soleus trigger points [28]. It is particularly important to distinguish between pain developing in the base of the heel as a result of an inflammatory lesion in the tendon, and pain referred to that site from trigger points in the soleus muscle. In Achilles tendonitis, the tendon is liable to be slightly swollen and there may be crepitus over it when the foot is moved. On examination, exquisitely tender trigger points are found in the tissues around the tendon. Inserting dry needles in the tissues overlying these trigger points may relieve the pain. This usually has to be repeated three or more times at weekly intervals in order to obtain any lasting benefit, but is certainly preferable to steroid injection at this site. The steroid injection is associated with much postinjection pain, and if inadvertently injected into the tendon sheath, may cause rupture of the tendon, requiring surgical repair [19]. Figure 13.2 shows the locations of the soleus trigger points.
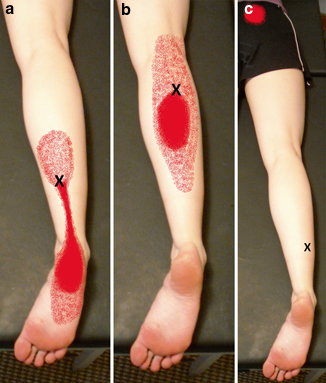
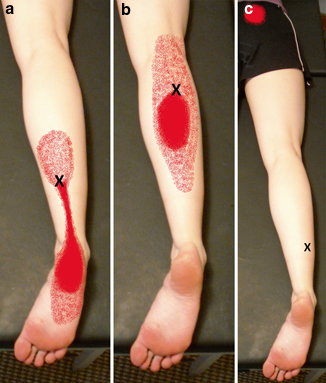
Fig. 13.2
Soleus trigger points (X) and pain referral patterns (red color). Solid color is primary site of pain, with stippling indicating the spillover pattern. a Trigger point 1, b trigger point 2, c trigger point 3
Plantaris trigger points are commonly associated with soleus tender points [27]. They primarily refer pain to the back of the knee as well, with pain extending about midway down the back of the calf [27]. Figure 13.3 shows the location of the plantaris trigger point.


Fig. 13.3
Plantaris trigger point (X) and pain referral pattern (red color). Solid color is primary site of pain, with stippling indicating the spillover pattern
Popliteus trigger points primarily refer pain to the back of the knee joint. Pain may be worse with crouching, going downhill or downstairs. There is rarely pain at night [27]. These trigger points may be associated with gastrocnemius and plantaris trigger points [27]. Figure 13.4 shows the location of the popliteus trigger point.


Fig. 13.4
cating the spillover patternPopliteus trigger point (X) and pain referral pattern (red color). Solid color is primary site of pain, with stippling indi
Tibialis posterior trigger points concentrate proximally over the Achilles tendon above the heel, but may extend from the trigger point down over the calf, the entire heel, and the plantar surface of the foot and toes [27]. The trigger points in the tibialis posterior may be indirectly palpated through other muscles. Interpreting tenderness at this site depends on the preceding examination establishing involvement of this muscle and determining that the surrounding muscles are free of tenderness [27]. Figure 13.5 shows the location of the tibialis posterior trigger point.


Fig. 13.5
Tibialis posterior trigger point (X) and pain referral pattern (red color). Solid color is primary site of pain, with stippling indicating the spillover pattern
The long toe flexors, flexor hallucis longus (FHL) and flexor digitorum longus (FDL) help to control motions of the foot. Trigger points may become activated in situations where the foot is unstable [27]. Pain referred from the FDL is felt in the middle of the plantar forefoot proximal to the lateral digits. Pain referred from the FHL is felt in the plantar surface of the great toe and head of the first metatarsal [27]. Figure 13.6 shows the locations of the long toe flexor trigger points.
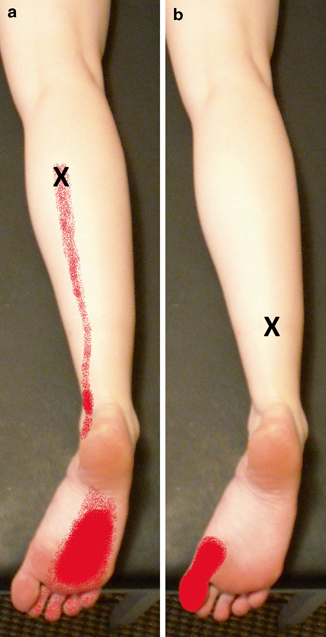
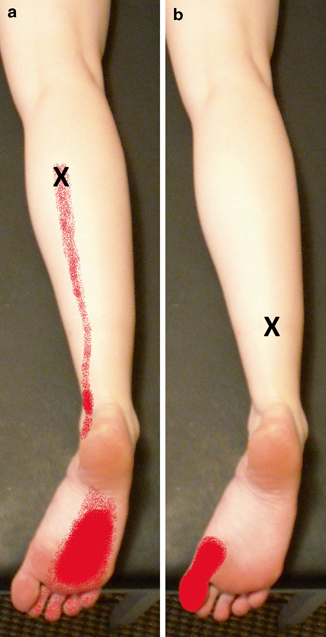
Fig. 13.6
Long toe flexor trigger points (X) and pain referral patterns (red color). Solid color is primary site of pain, with stippling indicating the spillover pattern. The flexor digitorum longus point (a) is pictured on the left, the flexor hallucis longus point (b) is pictured on the right
Trigger Point Treatment
Treatment is typically done with injection of a local anesthetic or dry needling, either with a small-gauge hypodermic needle or an acupuncture needle . Injections using preservative-free products are generally recommended to minimize the damage produced by the anesthetic [16]. This is consistent with the goal of minimizing neurological irritation.
The patient positions for gastrocnemius trigger injections are lateral recumbent on the ipsilateral side for trigger point 1, on the contralateral side for trigger point 2, and prone for trigger points 3 and 4. Using a pincer grasp on the trigger points, insert a 27-gauge 1.5-in. needle directly into trigger point 1 and trigger point 2 without worry of neurovascular structures. Injection of trigger point 3 and trigger point 4 must proceed with caution, and the needle should be directed away from the midline. The trigger points can be infiltrated with 0.5 mL of Marcaine 0.25 %, and this can be done with a multi-quadrant approach for trigger point 1 and trigger point 2 [16].
The patient positions for soleus trigger point injections are lateral recumbent on the ipsilateral side for trigger points 1 and 2, and on the contralateral side for trigger point 3. Using a pincer grasp on trigger point 1 and trigger point 3, insert a 27-gauge 1.5-in. needle into trigger point 1 through a medial approach and into trigger point 3 through a lateral approach. For injection of trigger point 2, the needle is directed toward the fibula, because the trigger point is close to the bone. The trigger points can be infiltrated with 0.5 mL of Marcaine 0.25 %. This can be done in a multi-quadrant approach for trigger point 1 and trigger point 2 [16].
Trigger point injection may result in soreness for 5–6 days afterward. The stretching exercises help to relieve this, but as a precaution you may only want to treat one side in a visit. The patient may also use acetaminophen for residual pain after the injection [16, 27]. Muscle retraining exercise and maintenance exercises are recommended after treatment [16].
Acupuncture/Dry Needling
The precise origin of acupuncture is a source of debate. Evidence exists for a variety of potential antecedent practices [29]. Even today, there is no standardized approach to acupuncture due to past acupuncture scholars freely editing prior texts [29]. Classic acupuncture refers to thin, solid metallic needles inserted into the skin at specific points along meridians that correspond to internal organs. This is done to restore the balance in the body. In traditional Chinese acupuncture, needle effectiveness is frequently measured by the elicitation of de qi. The patient may feel a throbbing ache, while the practitioner feels a grasp of the needle by the tissue [29]. One proposed theory is that acupuncture points are associated with anatomic locations of loose connective tissue. Studies have shown a relationship between fascial structures and acupuncture points and meridians, as well as a relationship between connective tissue and the effects of acupuncture [30–33]. One study has also shown a decrease in alpha-motoneuron activity after acupuncture [34]. When combined with the theories behind myofascial pain, acupuncture may have a role in treating pain associated with posterior lower extremity injuries.
Trigger points may be treated with acupuncture techniques including dry needling and intramuscular stimulation. A number 3 (0.2 mm by 40 mm) acupuncture needle is used. The patient position for treatments is prone. The trigger point(s) are identified. The acupuncture needle is placed perpendicular to the skin into the trigger point. The practitioner depresses the skin firmly with the insertion tube to cause a local anesthetic effect, then taps the needle through the skin barrier. The tube is removed and the needle directed toward the trigger point in a pecking/probing manner. The practitioner should proceed with caution for blood vessels and nerves that lie in the midline. Ideally, there will be muscle twitching in response to this procedure, as well as a grab of the needle by the muscle. This grab is usually released instantaneously [16]. The needle may be rotated until the patient feels a dull throbbing at the point. The procedure is terminated when the discomfort level is 7/10 per patient, or if there is no muscle grab and the muscle seems to have relaxed [16]. In some cases, there is a strong spasm of the muscle during treatment. In this case, the needle can be left in place for 10–20 min, without manipulating the needle, before removal. The spasm is not usually accompanied by pain unless the needle is manipulated during the spasm [16].
Muscle Energy
Muscle energy is a technique that may be used following trigger point treatments [16]. It was developed by Fred L. Mitchell, Sr., DO, although similar techniques were previously described [35]. There are nine different physiologic principles that may be used in muscle energy [35], although post-isometric relaxation may be the most common one used. The physiologic basis behind this principle is that immediately after isometric contraction, the neuromuscular apparatus is in a refractory state allowing for passive stretching to be performed without encountering strong myotactic reflex opposition [35]. Generally, the practitioner positions the patient’s body so that the muscle is at its pathological barrier. The patient pushes about 5 pounds of force against that barrier for 5 s while contracting the muscle (isometric contraction). Upon relaxing, the physician follows the relaxation to engage a new barrier reflecting the lengthened muscle. This is repeated 3–5 times or until the range of motion stops improving. If there is no release toward a new barrier, then the dysfunction is likely not of muscular origin, and the diagnosis should be reconsidered [16]. The post-contraction relaxation period prevents stretch receptors from activating [3], allowing for increased stretch in the muscle and increased range of motion at restricted joints.
The muscles of the posterior lower extremity can be treated with the patient prone and knee extended with their feet hanging off the end of the table. Dorsiflexion at the patient’s foot is controlled and encouraged through the physician’s leg or knee contact on the forefoot, to the point of the initial barrier. The patient is instructed to apply a plantar flexion force against the physician’s resistance for 5 s. Upon relaxation after the 5-s force the foot is dorsiflexed further into the new barrier. This is repeated 3–5 times or until no further barrier is appreciated. Ice or vapocoolant spray may be applied in a proximal to distal direction along the calf. This should be done after the initial plantar flexion to the barrier [16]. Treatment can also be done with the patient prone and knee flexed. Dorsiflexion at the patient’s foot is controlled and encouraged through the physician’s hand contact on the forefoot, to the point of the initial barrier. The patient is instructed to apply a plantar flexion force against the physician’s resistance for 5 s. Upon relaxation after the 5-s force the foot is dorsiflexed further into the new barrier. This is repeated 3–5 times or until no further barrier is appreciated. Cool and stretch may be used in this position also.
After cool and stretch, the muscle may be rewarmed with a heating pack for 5–10 min. After rewarming, the patient is instructed to move through their greatest range of motion [16]. Ideally, the patient should not return to previous activities immediately afterward, as the muscle needs a period of rest. Patients can attain the most benefit if they soak the muscle in a hot bath as soon as possible and practice the prescribed stretches. As the muscle fibers are allowed to relax, they release toxins, which may result in discomfort that the patient identifies as similar to the pretreatment pain. Stretching wrings the toxins out of the muscle and may result in immediate alleviation of posttreatment discomfort [16].
Strain–Counterstrain
This technique was developed by Lawrence H. Jones, DO, as a treatment for tender points in the muscle belly. These tender points can occur due to chemical or mechanical sensitization causing an increase in afferent flow [36–38]. Edema and increased muscular pressure may also induce these points locally in the muscle belly, but these points may be perpetuated by long-term changes in the synaptic processes in dorsal horn neurons [36]. These tender points share some characteristics with trigger points, but can be differentiated clinically (Table 13.2) and are still separated in the literature [38].
Table 13.2
Comparison of tender points and trigger points
Tender point | Trigger point |
|---|---|
No characteristic pain pattern | Characteristic pain pattern |
Located in muscle, tendons, ligaments, and fascia | Located in muscle tissue |
Locally tender | Locally tender |
Elicits jump sign when pressed | Elicits jump sign when pressed |
No radiating pattern when pressed | Elicits a radiating pain pattern when pressed |
Taut band not present | Present within a taut band of tissue |
Twitch response not present | Elicits twitch response with snapping palpation |
Dermographia not present | Dermographia of skin over point
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





