Chapter 6 Community Physiotherapy
Introduction
Treatment techniques/management approach
• For any treatment, as for assessment, there is the additional focus on improving function related to the patient’s needs and their environment.
• The intervention can take place in a variety of settings, from privately owned or rented property, Council or Housing Association accommodation, supported housing (sheltered or special sheltered), a caravan, hostel, Residential/Nursing Home or Day Centre.
Patient choice and rights
• Careful consideration must be given to:
Risk assessments
• Risk assessments should be carried out at the start of each treatment session as the environment may have changed since the previous visit. Risk assessment CSP (2002). Personal safety CSP (2009) (for the physiotherapist and the patient), Lone working CSP (2009).
• There will quite possibly not be any height-adjustable furniture or space for large pieces of equipment in the home environment. There could be environmental constraints when treatments take place in confined and cluttered areas, some of which may be unkempt or unclean.
• It may be difficult or impossible for a patient to manoeuvre, if they are becoming more dependent on a walking aid.
• Therefore, the environment may directly affect the choice of treatment. Moving and handling CSP (2009).
Consent
• Where consent is required for involvement with carers, either formal (through an agency) or informal (family and friends) this must be clarified in the treatment process (CSP, 2004; DH, 2001a,b,c; DH 2009).
• The involvement can be supporting the treatment regime through assistance with moving and handling, reinforcing exercise programmes, assisting with communication or helping to understand any cultural issues.
• Patients with a high level of anxiety can often be reassured by people who are familiar to them, especially when a physiotherapist is introducing alternative approaches to treatment or new activities.
Holistic assessment and treatment
• All patients should be assessed and treated holistically with functional treatments aimed at improving their independence, safety and quality of life.
• Assessment may have identified a need to involve other professionals in the treatment process and joint visits may be of benefit to the patients and physiotherapist.
• Treatment programmes or activities should always involve a good understanding of the rehabilitation ethos of enabling and handing over responsibility to the patient, wherever possible.
• If an assessment has highlighted a particular functional activity that the patient is unable to carry out independently or safely, the choice of treatment should be focussed on addressing this.
• As an example, toileting in the acute setting may require a patient to walk 10 or more metres on an uncarpeted floor to reach a toilet with adequate lighting and assistance if required.
• When this activity is attempted at home, a similar distance is likely to involve walking on different floor coverings, through doorways and in potentially poor lighting, so provision of a commode by the bed at night would improve patient safety.
• Practise getting out of bed, arranging their clothes, cleaning themselves and getting back into bed.
• To be able to go to the toilet safely and independently at night contributes greatly to an individual’s quality of life and dignity and involves the coordinated action of different muscle groups, strength, balance, adequate range of movement and confidence to perform the task.
• There may also need to be provision of equipment for bed mobility to facilitate these activities.
• Another example of a functional activity would involve accessing a drink. In the acute setting, this is usually provided by staff. In the home setting a patient will need to plan how this is going to take place.
• The task will involve mobility, balance whilst multi-tasking, manual dexterity and transportation of the drink.
• This would apply to people of all ages and advice and exercises to address these activities should be incorporated into treatment programmes.
• Problem solving of the transportation for someone using a walking aid may include provision of a kitchen trolley or advising the use of a pocketed apron or shoulder bag in which to hold a bottle of liquid.
Pain management
• Treatments may involve the need for pain control, increasing range of movement, muscle strength, training on safe positioning, provision of appropriate equipment, improving balance and safety instructions.
• Repetition of activities may address some of these issues and can be carried out under the supervision of a delegated rehabilitation assistant or alternative carer.
• Treatments involving electrical and other equipment may be limited by the mode of transport used to travel to a patient and the environment of the patient.
• However, treatments can be carried out where appropriate using any of the following in the community: transcutaneous electrical nerve stimulator (TENS), portable ultrasound machine, pulse oximeter, interferential therapy, acupuncture, gym balls, Thera-Band and cuff weights for ankles and wrists.
Documentation
• All treatment interventions, conversations (with patients, formal and informal carers, family, friends and other colleagues and health professionals), giving advice and information must be carefully and accurately documented.
• If a patient chooses not to take your advice for whatever reason, this must also be documented (CSP, 2000).
Treatments specific to the speciality area
• The community is a speciality area using core skills that are enhanced by other specialities and skills specific to the environment.
• It should be recognised that it is not always possible to carry out a ‘traditional’ style of physiotherapy treatment and this may depend on the needs of a particular patient at a particular time in their unique setting.
• Invariably the treatment will involve problem-solving skills, using initiative, common sense and flexibility in approach.
• The physiotherapist may find that they are using a whole set of skills, apart from physiotherapy, as the treatment will be holistic and not just medical.
• The physiotherapist may need to draw on knowledge relating to other issues affecting the patient, for example, difficulty in accessing housing or other benefits, the involvement of young carers, may be of great concern to someone and until resolved, they may not be able to engage fully with their treatment plans.
• Following an assessment, the treatment will always take into consideration the specific abilities and needs of the patient.
• SMART goals will be agreed jointly between the physiotherapist and the patient (DH, 2001a).
Activities of daily living (ADL)
Patient confidentiality
• There are confidentiality issues if relatives, friends or neighbours are present.
• Just because a person is receiving their physiotherapy treatment within their own home does not alter the fact that they may not want anybody else present.
• Even if the neighbour is also their main carer, this does not automatically mean they are entitled to be present or contribute to the treatment session in any way, nor are they entitled to any information about the patient or their progress after a treatment session, unless the express permission to allow this has been given by the patient.
• Partners are also not automatically entitled to any information just because of their marital status (DH, 2003).
Cultural considerations
• Respect has to be given to cultural and religious beliefs in someone’s own home, but expectations of the patient should not compromise the physiotherapist’s rights, for example, taking off your shoes in someone’s house.
• Is there a way to reach a compromise, maybe by covering your shoes with an acceptable material?
Treatments related to specific areas of the home
• It is important to look at the home as the treatment/rehabilitation base.
• Treatment should always be functional and when related to daily living and activities it will encourage more compliance and ongoing adherence to the treatment plan.
• The advantage of treating someone in their home environment is that it gives the patient an opportunity to talk about their condition/s and about any concerns that they may have and how to manage them, or any other related questions.
• It may be that the physiotherapist will not be able to ‘cure’ the problem, but will be able to talk through or demonstrate effective ways to manage it.
• Advice based on this information will provide lifelong benefits to the patient.
• The physiotherapist is a great source of information and knowledge to the patient and should ensure that relevant written resources are provided (these are often available from self-help groups and charities or from the internet).
• In each area of the home, it is necessary to consider:
• There are some issues that need to considered during treatments in all areas, such as appropriate footwear, the potential use of assistive technology (including the use of a pendant alarm) and personal safety issues (for the physiotherapist, rehabilitation assistant or support worker, the patient and the carers).
• Patients should be encouraged to utilise as much of their environment as is possible to do safely and should resist the temptation to remain static, with the expectation that everything will be done for them (DH, 2001a).
• The community physiotherapist’s work is fundamentally functional, therefore it is important to incorporate the patient’s daily routine into the treatment plan. Therefore, a good place to start would be.
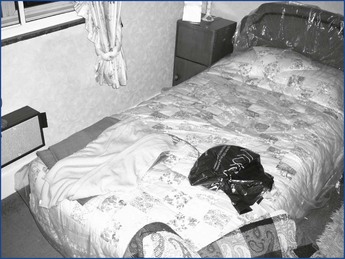
The Bedroom (upstairs or downstairs) (Figure 6.1)
Environmental considerations
• How much furniture or clutter is in the room? Are these forming obstacles? Can they be moved and re-positioned to improve the ability of the patient to mobilise and therefore reduce risk, if the patient agrees?
• Are there rugs or cables across the floor? Is it possible to tape down loose wiring and carpet edges and remove rugs, if the patient agrees? Can this be carried out by family members or the voluntary sector? Advise on risks, if the patient is unwilling or unable to adopt safer options.
• Is there adequate lighting/heating/ventilation (LHV)? Advise the patient to use a light if they need to get in and out of bed at night. When advising about the use of heating in the bedroom, it is an Act of Law that there should not be a working gas fire in a room where someone is sleeping unless it is a room-sealed appliance or it incorporates a safety control that will shut down the appliance to prevent a build up of combustible gas in the room concerned (GSR 1998 and HSE 1998).
• Bed is not always height adjustable or as firm as the conventional physiotherapy plinth. The bed that is in situ may be the only option available to you that can be used as the place to do exercises for limbs, trunk, balance, posture and to practice sitting to standing and standing to sitting.
• Consider joint visits with or referral to an occupational therapist (OT). However, this may involve different time scales depending on whether there is an occupational therapist in your team or access to a ‘Trusted Assessor’ (a physiotherapist, nurse or support worker who, when trained, will be able to assess for and prescribe a simple solution or a basic piece of equipment to meet the needs of an individual) available. It may be necessary to make a referral to an OT in Social Services.
• A patient may have started to use a commode or walking aid that prevents safe access to the side of the bed on which they usually sleep. In this case if the patient has accessed the bed in a specific way that is no longer possible, then an alternative method has to be developed and practiced to ensure the patient is able to get onto and off the bed safely.
• Advise on appropriate footwear and where it is safely accessible.
• Remind the patient to put on their pendant alarm, if they use one, before getting out of bed.
Functional treatments
Adaptive equipment/exercises
• To assist the physiotherapist to adapt to this different working environment, the following will provide suggestions of alternatives to the equipment more commonly encountered in a hospital/clinic setting.
• Physiotherapists will find that they have to be creative and adaptable within a community environment, often using available resources such as:
Involvement of other agencies and informal carers
• An equipment assessment with an occupational therapist could facilitate the treatments and personal activities of daily living with provision of bed equipment, bed raises or a commode.
• A community nurse can order a specialist bed, if required for nursing management, such as a height-adjustable/profiling bed with a pressure relieving mattress.
• The informal carers should be involved in the treatment process (with the patient’s consent) and shown specific techniques to avoid carer strain, such as using sliding sheets.
• Suppliers of assistive technology such as a pressure pad on the floor that switches the light on when the patient stands on it.
The bathroom and toilet (Figure 6.2)
• If it is a goal, the patient will expect to access the bathroom; however, not all patients need to access the bathroom to wash as they may just use a bowl in another room.
Environmental considerations
• What type of floor covering and what state of repair is it in?
• Ensure floor coverings are safe, i.e. not loose or slippery.
• Can they be moved and re-positioned to reduce risk, if the patient agrees?
• Ensure lighting is accessible and sufficient, especially if the patient needs to move around the home at night.
• Is there already equipment in situ and is it appropriate and safe for purpose.
• Advise on use or misuse of fittings already in situ, e.g. it may be possible to pull up from the toilet using a secure towel rail, but not using the toilet roll holder.
• Always advise against using a radiator to pull up on as this could lead to burns. Consider a joint visit with an OT or referral to an OT in a community or Social Services team.
• Is there sufficient access through the doorway for a walking aid?
• Is there room for a walking aid inside the bathroom/toilet?
• Is there floor space for equipment if needed, e.g. a perching stool?
• Is there space for a carer to be present?
• Does the patient become short of breath performing certain personal care activities? If appropriate, a perching stool or another suitable item of equipment can be supplied.
• If a pendant alarm is used, remind patient to always replace it around their neck after washing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree