Chapter Seven Common sporting illnesses and injuries
Demonstrate care and management of athletes suffering from sporting-related injuries and illnesses.
1. Define and apply the RICER and NO HARM principles.
2. Recognise and manage athletes with hard and soft tissue injuries.
3. Recognise and manage head and spinal injuries.
4. Recognise and manage trunk injuries.
5. Recognise and manage upper limb injuries.
6. Recognise and manage lower limb injuries.
7. Recognise and manage heat and cold injuries and illness.
8. Recognise and manage signs and symptoms of shock.
9. Recognise and manage serious bleeding.
Shock
Management of shock
 If any signs or symptoms of shock are present, seek medical help urgently.
If any signs or symptoms of shock are present, seek medical help urgently.
 If the athlete is apparently unresponsive, commence the DRSABCD principles.
If the athlete is apparently unresponsive, commence the DRSABCD principles.
 Lay the athlete on their back in a horizontal position to maintain circulation to the trunk. Do not elevate the head.
Lay the athlete on their back in a horizontal position to maintain circulation to the trunk. Do not elevate the head.
 If a head or spinal injury is not suspected, raise the athlete’s legs but keep the head level with the heart.
If a head or spinal injury is not suspected, raise the athlete’s legs but keep the head level with the heart.
 Loosen any tight clothing or protective equipment.
Loosen any tight clothing or protective equipment.
 Protect the athlete from extremes of temperature.
Protect the athlete from extremes of temperature.
 Moisten the athlete’s lips, but do not give drinks or food.
Moisten the athlete’s lips, but do not give drinks or food.
 Continue to monitor the athlete closely as they may deteriorate rapidly.
Continue to monitor the athlete closely as they may deteriorate rapidly.
Serious bleeding
The standard procedure for treating an athlete with serious life-threatening bleeding is:
 Apply and maintain direct pressure to control bleeding. Pressure is applied using gloved fingers or the heel of the hand in conjunction with sterile or clean compress pads, bandages or towels.
Apply and maintain direct pressure to control bleeding. Pressure is applied using gloved fingers or the heel of the hand in conjunction with sterile or clean compress pads, bandages or towels.
 If bleeding is heavy or a dressing is not available, grasp the sides of the wound and press them firmly together.
If bleeding is heavy or a dressing is not available, grasp the sides of the wound and press them firmly together.
 If bleeding persists, do not remove the dressing. Apply further pads and bandaging.
If bleeding persists, do not remove the dressing. Apply further pads and bandaging.
 In the case of bleeding from a limb, elevate the injured part while supporting any suspected fracture.
In the case of bleeding from a limb, elevate the injured part while supporting any suspected fracture.
 Do not try to clean major bleeding as stopping the bleeding using direct pressure is critical.
Do not try to clean major bleeding as stopping the bleeding using direct pressure is critical.
 Apply oxygen therapy when it is available and qualified personnel are present.
Apply oxygen therapy when it is available and qualified personnel are present.
Hard tissue injuries
Fractures
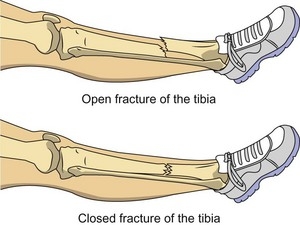
A fracture is an injury where bone tissue loses its normal structure, usually as a result of direct or indirect trauma. There are many different types of fractures; they can be classified according to the type of damage to the bone (e.g.complete/incomplete, displaced/undisplaced) as well as whether the fractured bone penetrates the skin and causes an open wound (open fracture/closed fracture – see Figure 7.1). Fractures can also be classified according to the cause, such as stress fractures, which commonly occur in sport because of overuse or biomechanical problems the athlete might have.
Fractures usually present with:
 the occurrence of a forceful episode
the occurrence of a forceful episode
 being hit by an object or opponent
being hit by an object or opponent
 possible deformity or swelling
possible deformity or swelling
Management of fractures
 Follow DRSABCD principles as appropriate.
Follow DRSABCD principles as appropriate.
 If the athlete is conscious, reassure them and advise them not to move.
If the athlete is conscious, reassure them and advise them not to move.
 Call for an ambulance or medical assistance.
Call for an ambulance or medical assistance.
 Control bleeding if there is an open wound and cover it with a sterile dressing to reduce infection.
Control bleeding if there is an open wound and cover it with a sterile dressing to reduce infection.
 Check that circulation is present distal to the fracture. If not, call for urgent medical aid.
Check that circulation is present distal to the fracture. If not, call for urgent medical aid.
 If the athlete needs to be moved, immobilise the area of the suspected fracture first.
If the athlete needs to be moved, immobilise the area of the suspected fracture first.
 Immobilise the injured limb in the position you found it.
Immobilise the injured limb in the position you found it.
 Be sure to immobilise the area above and below the fracture.
Be sure to immobilise the area above and below the fracture.
 If the fracture needs to be splinted, the splint must be long enough to extend past the joints above and below the fracture site as well as wide enough to support the fracture site.
If the fracture needs to be splinted, the splint must be long enough to extend past the joints above and below the fracture site as well as wide enough to support the fracture site.
 Check the athlete for other injuries and treat appropriately.
Check the athlete for other injuries and treat appropriately.
 Apply ice packs or cold compresses, if possible, for up to 20 minutes if pain permits. Reapply ice every 2 hours if necessary. Do not apply ice to open fractures.
Apply ice packs or cold compresses, if possible, for up to 20 minutes if pain permits. Reapply ice every 2 hours if necessary. Do not apply ice to open fractures.
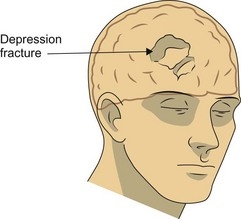
Management of skull fractures
Skull fractures may be characterised by:
Management of skull fractures includes the following steps:
 Rest and prevent the athlete from sustaining possible further harm.
Rest and prevent the athlete from sustaining possible further harm.
 Place the athlete in a position of comfort if possible.
Place the athlete in a position of comfort if possible.
Management of upper and lower arm fractures
 Control bleeding if there is an open wound and cover it with a sterile dressing to reduce infection. Apply padding around any protruding bones.
Control bleeding if there is an open wound and cover it with a sterile dressing to reduce infection. Apply padding around any protruding bones.
 For lower arm fractures, apply a splint from the elbow to the hand to immobilise the fracture. Support the fracture using a broad arm sling.
For lower arm fractures, apply a splint from the elbow to the hand to immobilise the fracture. Support the fracture using a broad arm sling.
 If the suspected fracture involves the elbow or is very close to it, do not move the elbow. Support and immobilise the arm in the position you found it.
If the suspected fracture involves the elbow or is very close to it, do not move the elbow. Support and immobilise the arm in the position you found it.
 For upper arm fractures, place a pad between the arm and the chest and apply an elevated arm sling to immobilise the arm.
For upper arm fractures, place a pad between the arm and the chest and apply an elevated arm sling to immobilise the arm.
 Check that circulation is present beyond the fracture. If not, call for urgent medical aid.
Check that circulation is present beyond the fracture. If not, call for urgent medical aid.
 Check the athlete for other injuries and treat appropriately.
Check the athlete for other injuries and treat appropriately.
Management of upper and lower leg fractures
 Control bleeding if there is an open wound and cover it with a sterile dressing to reduce infection. Apply padding around protruding bones.
Control bleeding if there is an open wound and cover it with a sterile dressing to reduce infection. Apply padding around protruding bones.
 The uninjured leg may be used as a splint for upper and lower leg fractures. Place a pad or splinting material between the legs, bring the uninjured leg to the injured leg and tie the legs together with bandages above and below the suspected fracture. Tie off on the uninjured side.
The uninjured leg may be used as a splint for upper and lower leg fractures. Place a pad or splinting material between the legs, bring the uninjured leg to the injured leg and tie the legs together with bandages above and below the suspected fracture. Tie off on the uninjured side.
 If the ground is supporting the limb adequately there may be no need to splint it to the other limb.
If the ground is supporting the limb adequately there may be no need to splint it to the other limb.
 Check that circulation is present beyond the fracture. If not, call for urgent medical aid.
Check that circulation is present beyond the fracture. If not, call for urgent medical aid.
 Check the athlete for other injuries and treat appropriately.
Check the athlete for other injuries and treat appropriately.
Management of hip fractures
 Control bleeding if there is an open wound and cover it with a sterile dressing to prevent infection. Apply padding around protruding bones.
Control bleeding if there is an open wound and cover it with a sterile dressing to prevent infection. Apply padding around protruding bones.
 The uninjured leg may be used as a splint for hip fractures. Place a pad between the legs, bring the uninjured leg to the injured leg and tie the legs together with triangular bandages above and below the fracture, at the knees and at the ankles/feet. Tie off on the uninjured side.
The uninjured leg may be used as a splint for hip fractures. Place a pad between the legs, bring the uninjured leg to the injured leg and tie the legs together with triangular bandages above and below the fracture, at the knees and at the ankles/feet. Tie off on the uninjured side.
 Do not move the athlete unless they are in life-threatening danger. If they must be moved, immobilise them on a spinal board or similar hard surface.
Do not move the athlete unless they are in life-threatening danger. If they must be moved, immobilise them on a spinal board or similar hard surface.
 Check for signs of circulation distal to the fracture site.
Check for signs of circulation distal to the fracture site.
Management of pelvic fractures
 Control bleeding if there is an open wound and cover it with a sterile dressing to prevent infection. Apply padding around protruding bones.
Control bleeding if there is an open wound and cover it with a sterile dressing to prevent infection. Apply padding around protruding bones.
 Place the legs and feet in a position of comfort.
Place the legs and feet in a position of comfort.
 Discourage the athlete from urinating.
Discourage the athlete from urinating.
 Monitor vital signs and treat for shock.
Monitor vital signs and treat for shock.
 Do not move the athlete unless they are in life-threatening danger. If they must be moved, immobilise them on a spinal board or similar hard surface.
Do not move the athlete unless they are in life-threatening danger. If they must be moved, immobilise them on a spinal board or similar hard surface.
Management of rib fractures
 Ensure the athlete is in a comfortable position. If possible, allow them to find their own position of comfort. A half-sitting position resting the affected side on a pillow or cushion is ideal.
Ensure the athlete is in a comfortable position. If possible, allow them to find their own position of comfort. A half-sitting position resting the affected side on a pillow or cushion is ideal.
 Encourage shallow breathing to reduce pain.
Encourage shallow breathing to reduce pain.
 Apply padding over the affected ribs.
Apply padding over the affected ribs.
 Place the arm that is on the same side as the injury over the pad.
Place the arm that is on the same side as the injury over the pad.
 Secure the pad with broad bandages over the arm and around the body, tying them off on the non-injured side.
Secure the pad with broad bandages over the arm and around the body, tying them off on the non-injured side.
 Immobilise the arm using an appropriate sling.
Immobilise the arm using an appropriate sling.
 Be aware that breathing difficulties may be associated with rib fractures.
Be aware that breathing difficulties may be associated with rib fractures.
Dislocations
Management of a dislocation
 Do not attempt to reposition the dislocated joint.
Do not attempt to reposition the dislocated joint.
 Prevent movement occurring at the site of the dislocation to reduce the risk of further tissue damage.
Prevent movement occurring at the site of the dislocation to reduce the risk of further tissue damage.
 Immobilise the injured limb in the position you found it.
Immobilise the injured limb in the position you found it.
 Gently apply a splint and sling. Be sure to immobilise the area above and below the injured joint.
Gently apply a splint and sling. Be sure to immobilise the area above and below the injured joint.
 Check for signs of circulation below the dislocation.
Check for signs of circulation below the dislocation.
 If possible, apply ice packs or cold compresses for up to 20 minutes at a time to relieve pain. Reapply if necessary.
If possible, apply ice packs or cold compresses for up to 20 minutes at a time to relieve pain. Reapply if necessary.
Rules for managing dislocations
Soft tissue injuries
 Muscle – muscles consist of cells with a specific function, namely to contract to produce movement of the body. They are usually attached to bones by tendons. Muscles have an extensive blood supply and consequently may bleed heavily when injured. The common injuries that occur to muscle tissue are strains and contusions/bruises.
Muscle – muscles consist of cells with a specific function, namely to contract to produce movement of the body. They are usually attached to bones by tendons. Muscles have an extensive blood supply and consequently may bleed heavily when injured. The common injuries that occur to muscle tissue are strains and contusions/bruises.
 Tendons – tendons are tough bands of slightly elastic connective tissue that connect muscle to bone. Tendons relay the force the muscle produces to the bones to cause movement. Common injuries to tendons include strains or complete tears (rupture) and inflammation or degeneration of the tendon (tendinopathy).
Tendons – tendons are tough bands of slightly elastic connective tissue that connect muscle to bone. Tendons relay the force the muscle produces to the bones to cause movement. Common injuries to tendons include strains or complete tears (rupture) and inflammation or degeneration of the tendon (tendinopathy).
 Ligaments – ligaments are strong bands of fibrous tissue that attach to adjacent bones in joints. They enhance the stability of the joint. An injured ligament is called a sprain.
Ligaments – ligaments are strong bands of fibrous tissue that attach to adjacent bones in joints. They enhance the stability of the joint. An injured ligament is called a sprain.
 The joint capsule – this is the thin ligamentous tissue that surrounds joints and produces the lubricating synovial fluid found in joints. These tissues can also be injured with a joint strain, dislocation or subluxation.
The joint capsule – this is the thin ligamentous tissue that surrounds joints and produces the lubricating synovial fluid found in joints. These tissues can also be injured with a joint strain, dislocation or subluxation.
 Skin and fatty tissue – an injury to any of these tissues is classified as a soft tissue injury.
Skin and fatty tissue – an injury to any of these tissues is classified as a soft tissue injury.
Process of injury and repair in soft tissue injuries
There are eight stages in the process of injury and repair:
Secondary tissue damage
Additional or secondary tissue damage may be caused by:
 movement, which may lead to the tearing of more tissue or cause more bleeding damage
movement, which may lead to the tearing of more tissue or cause more bleeding damage
 damaged capillaries that continue to bleed, hence causing some cells in the damaged tissue to not receive their required blood supply, thereby leading to further damage
damaged capillaries that continue to bleed, hence causing some cells in the damaged tissue to not receive their required blood supply, thereby leading to further damage
 tissue swelling, which can compress the small blood vessels in the area and reduce circulation to the damaged area.
tissue swelling, which can compress the small blood vessels in the area and reduce circulation to the damaged area.