Common Problems in Ambulatory Internal Medicine (Case 2: A Problem Set of Five Common Cases)
Madelaine R. Saldivar MD, MPH and M. Susan Burke MD
CASE 1
A 35-Year-Old Woman with Headache
The patient is a 35-year-old healthy woman who comes to the office with daily headache and dizziness for 6 weeks. Her only medication is an oral contraceptive. Her exam is unremarkable except for a blood pressure of 130/90 mm Hg and body mass index of 30.
Differential Diagnosis
Primary Headache | Secondary Headache |
Migraine | Medication side effect |
Tension | Inflammatory: systemic lupus erythematosus (SLE), temporal arteritis |
| Infectious: meningitis, sinusitis |
| Intracranial mass or hemorrhage |
When we see this patient in the office, our first task is to determine whether she is well enough to continue her evaluation in the office. Signs and symptoms that warrant consideration for immediate transfer to the emergency department (ED) for emergent evaluation include sudden-onset severe headache, focal neurologic complaints, projectile vomiting, and severe hypertension. Headaches are common, and 90% of the time there will be a benign cause. A gradual onset of symptoms and a precipitating event, such as increased stress or a recent viral illness, make us consider benign causes.
PATIENT CARE
Clinical Thinking
• A careful history is the best tool to narrow the differential diagnosis.
• Radiologic studies are reserved for persistent or changed symptoms.
• Counseling on modifying environmental and lifestyle triggers is important.
History
Making sure there are no concerning symptoms is important. These are:
• Accompanying systemic symptoms
• Headache brought on by exertion
• Visual changes or focal neurologic deficits
• Sudden onset of the worst headache of one’s life
• Change in the pattern of chronic headache
Physical Examination
Tests for Consideration
$334 | |
$534 | |
$11 | |
$12 | |
$21 | |
$272 | |
$4 | |
$16 | |
$4 |
| Clinical Entities | Medical Knowledge |
Migraine Headache | |
Pφ | The pathophysiology of headaches is not well understood. However, experts agree that there are multiple factors that contribute to development of a headache: 1. Increased neuroexcitation with cortical spreading depression 2. Vascular dilation |
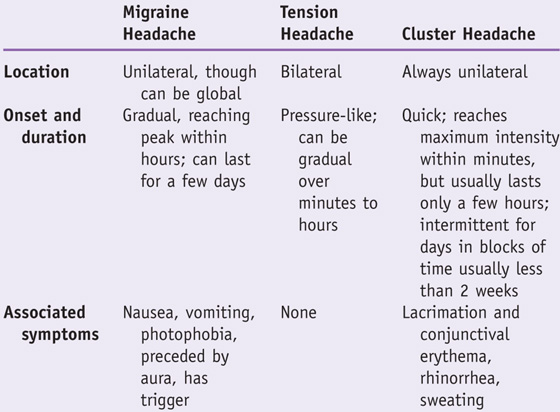
TP | Migraine can be distinguished from other types of primary headaches by its characteristics. |
Dx | Making the diagnosis is based on history and physical. Secondary causes and warning signs of more serious causes should not be present. |
Tx | All of the headaches described above respond to acute management with analgesics. Acetaminophen and ibuprofen have been shown to be effective as first-line medications for tension and migraine headaches. Remove headache triggers—alcohol, chocolate, sweeteners, caffeine, nitrites, hormonal medications, stress, and schedule changes or sleep deprivation. If migraine headaches persist, consideration should be given to headache prophylaxis with daily suppressive therapy (e.g., amitriptyline, β-blocker, or topiramate). See Cecil Essentials 119. |
Secondary headaches are discussed in Chapter 64, Headache.

Practice-Based Learning and Improvement: Evidence-Based Medicine
Title
Practice parameter: evidence-based guidelines for migraine headache; report of the Quality Standards Subcommittee of the American Academy of Neurology
Problem
What are evidence-based approaches to treating migraine headache?
Intervention
Analgesic medications and prophylactic medications
Quality of evidence
Systematic review of class I studies for treatment, class I, II, and III studies for diagnosis and neuroimaging utility
Outcome/effect
Migraine is a chronic condition with episodic attacks that affects 18% of women and 6% of men. Treat acute attacks rapidly. Consider prophylactic medications to reduce disability, frequency, and severity associated with attacks.
Historical significance
Migraine headaches are common and are disabling at a significant cost to society due to lost work productivity.
CASE 2
A 43-Year-Old Man with Back Pain
The patient is a 43-year-old truck driver who presents with right lower back pain (LBP) that started about a week ago when he lifted a heavy load at work. He stopped working and has been resting ever since. He tried acetaminophen, which did not help; however, his brother’s oxycodone with acetaminophen does provide him with relief.
Differential Diagnosis
Mechanical/nonspecific | Disk herniation | Compression fracture |
Degenerative spine disorders | Spinal stenosis |
|
Speaking Intelligently
Back pain is the second most common symptom-related reason for which patients present to the doctor. The vast majority of low back pain is due to mechanical or nonspecific causes and does not require imaging. The goal of evaluation is to identify those patients needing urgent attention by looking for signs and symptoms (red flags) suggesting an underlying condition that may be more serious and by determining who may need urgent surgical evaluation. We also evaluate for psychosocial factors (yellow flags), because they are stronger predictors of LBP outcomes than either physical examination findings or severity and duration of pain.
PATIENT CARE
Clinical Thinking
History
• Look for secondary gain, such as work disability and litigation.
• Evaluate for red flag symptoms that suggest more ominous causes requiring immediate evaluation.
• Recent significant trauma, mild trauma with age over 50 years
• Unexplained fever or recent urinary tract infection
• Prolonged use of glucocorticoids
• Progressive motor or sensory deficit
• Duration longer than 6 weeks
• Saddle anesthesia, bilateral sciatica/weakness, urinary or fecal difficulties
Physical Examination
• Observe patient walking and changing position.
• Check reflexes and sensation.
• Test for manual strength in both legs. Can the person walk on his or her heels (L5) and toes (S1)?
| Clinical Entities | Medical Knowledge |
Mechanical Low Back Pain/Nonspecific | |
Pφ | Complex and multifactorial; can involve any lumbar spine elements including bones, ligaments, tendons, disks, muscle, and nerve. Onset may be from an acute event or cumulative trauma. Most common presentation of back pain. May be divided into acute (<4 weeks), subacute (4–12 weeks), or chronic (>12 weeks). |
TP | Pain can be hard for patient to localize because of the small cortical region dedicated to the back. |
Dx | Clinical diagnosis; imaging is indicated only if red flags are present or symptoms persist. More than 90% of symptomatic lumbar disk herniations occur at the L4/L5 and L5/S1 levels. |
Tx | Most mechanical LBP resolves within 6 weeks. If it persists or worsens (or both), consider imaging. For acute pain use heat, nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and/or spinal manipulation. For chronic pain, use exercise, heat, NSAIDs, tricyclic antidepressants, and/or spinal manipulation. May also consider acupuncture or cognitive behavioral therapy. See Cecil Essentials 119. |
Disk Herniation | |
Pφ | Herniation is thought to result from a defect in the annulus fibrosus, most likely due to excessive stress applied to the disk, with extrusion of material from the nucleus pulposus. Herniation most often occurs on the posterior or posterolateral aspect of the disk. |
TP | Dermatomal distribution of sensory deficit, motor weakness, or hyporeflexia. |
Dx | Clinical exam including SLR test. MRI is indicated only if weakness or incontinence is present. |
Tx | Initial treatment is with analgesics and/or steroids. Surgery is reserved for patients with refractory pain or with evidence of motor deficits. Outcomes are similar at 5 years for patients treated either way. |