Chapter Eight Common medical conditions affecting athletes
Common medical conditions
Medical management plans should take into consideration:
For the protection of the athlete and to assist the sports trainer, every athlete should:
 undertake a pre-competition medical assessment (PCMA) with their doctor. The pre-exercise screening system developed by SMA in conjunction with Exercise Sports Science Australia and Fitness Australia could also be used
undertake a pre-competition medical assessment (PCMA) with their doctor. The pre-exercise screening system developed by SMA in conjunction with Exercise Sports Science Australia and Fitness Australia could also be used
 for athletes with medical conditions, obtain clearance from a medical practitioner before beginning a new season
for athletes with medical conditions, obtain clearance from a medical practitioner before beginning a new season
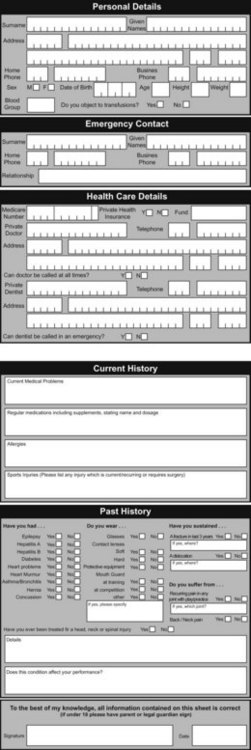
 complete an athlete medical profile form that outlines their medical history
complete an athlete medical profile form that outlines their medical history
 notify the sports trainer of any changes to their condition or medications, including recent illnesses not of a chronic nature such as a virus or other infection.
notify the sports trainer of any changes to their condition or medications, including recent illnesses not of a chronic nature such as a virus or other infection.
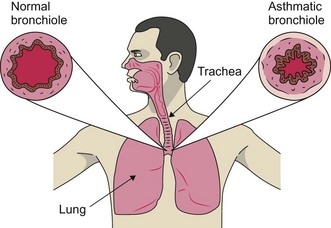
Asthma
Some general triggers for asthma include:
 allergies, commonly including dust, pollens, grasses, lawn cuttings, animal hair
allergies, commonly including dust, pollens, grasses, lawn cuttings, animal hair
 certain medications, such as aspirin
certain medications, such as aspirin
 viral illnesses, including colds and flu
viral illnesses, including colds and flu
Signs of an asthma attack
 noisy breathing, such as coughing or wheezing
noisy breathing, such as coughing or wheezing
 in children, skin being sucked in around the base of the neck and between the ribs.
in children, skin being sucked in around the base of the neck and between the ribs.
Management of a severe asthma attack
 Sit the athlete comfortably upright. Be calm and reassuring.
Sit the athlete comfortably upright. Be calm and reassuring.
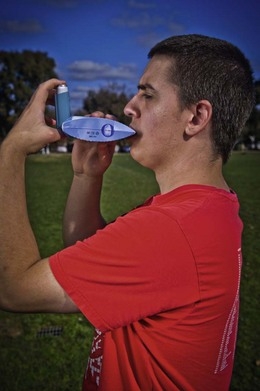
 Help administer four puffs of a reliever or combination inhaler (Ventolin, Airomir, Epaq, Symbicort or Asmol).
Help administer four puffs of a reliever or combination inhaler (Ventolin, Airomir, Epaq, Symbicort or Asmol).
 Relievers are best given through a spacer, if available. Use one puff at a time and ask the person to take four breaths from the spacer after each puff. Use the person’s own inhaler if possible. If not, use the inhaler from the first aid kit or borrow one from someone else.
Relievers are best given through a spacer, if available. Use one puff at a time and ask the person to take four breaths from the spacer after each puff. Use the person’s own inhaler if possible. If not, use the inhaler from the first aid kit or borrow one from someone else.
 Wait 4 minutes. If there is no improvement, give another four puffs, ensuring the person takes four breaths in and out through the spacer after each puff of medication.
Wait 4 minutes. If there is no improvement, give another four puffs, ensuring the person takes four breaths in and out through the spacer after each puff of medication.
 If there is little or no improvement, call an ambulance immediately and state that the athlete is having an asthma attack. Keep giving four puffs every 4 minutes until the ambulance arrives.
If there is little or no improvement, call an ambulance immediately and state that the athlete is having an asthma attack. Keep giving four puffs every 4 minutes until the ambulance arrives.
Reliever medication with a spacer
 Shake the inhaler and insert the mouthpiece into the spacer.
Shake the inhaler and insert the mouthpiece into the spacer.
 Place the spacer mouthpiece in the person’s mouth and fire one puff.
Place the spacer mouthpiece in the person’s mouth and fire one puff.
 Ask the person to breathe in and out normally for about four breaths.
Ask the person to breathe in and out normally for about four breaths.
 Repeat in quick succession until four puffs have been given.
Repeat in quick succession until four puffs have been given.
First asthma attack
 If someone collapses and appears to have difficulty breathing, call an ambulance immediately, whether or not the person is known to have asthma.
If someone collapses and appears to have difficulty breathing, call an ambulance immediately, whether or not the person is known to have asthma.
 Give four puffs of a reliever and repeat if there is no improvement.
Give four puffs of a reliever and repeat if there is no improvement.
 Keep giving four puffs every 4 minutes until the ambulance arrives.
Keep giving four puffs every 4 minutes until the ambulance arrives.
 No harm is likely to result from giving a reliever to someone who does not have asthma.
No harm is likely to result from giving a reliever to someone who does not have asthma.
 If a reliever is used for an athlete who is not known to have asthma, the athlete must be referred to a doctor for further assessment; this may confirm a diagnosis of asthma and thus require ongoing medical management.
If a reliever is used for an athlete who is not known to have asthma, the athlete must be referred to a doctor for further assessment; this may confirm a diagnosis of asthma and thus require ongoing medical management.
Asthma medications
There are three types of medications prescribed for asthma:
Asthma and the athlete
 know the severity of their asthma
know the severity of their asthma
 exercise safely and regularly to improve fitness and lung function
exercise safely and regularly to improve fitness and lung function
 avoid trigger factors where possible
avoid trigger factors where possible
 perform at their best by using the right medication in the correct manner
perform at their best by using the right medication in the correct manner
 have their asthma checked regularly by their doctor – every 6 months
have their asthma checked regularly by their doctor – every 6 months
 have a ready supply of medication for use before, during and after exercise.
have a ready supply of medication for use before, during and after exercise.
Pre-exercise advice
During pre-exercise, the athlete should avoid:
 allergy triggers, where possible (e.g. dust, pollens, grasses etc)
allergy triggers, where possible (e.g. dust, pollens, grasses etc)
 exercising in cold air (e.g. early morning or late evening)
exercising in cold air (e.g. early morning or late evening)
 vigorous exercise when the athlete has a viral infection
vigorous exercise when the athlete has a viral infection
 any exercise if the athlete is wheezing or has a chest infection.
any exercise if the athlete is wheezing or has a chest infection.
 warm up adequately to allow the body to adapt to changes in the weather; an indication of an adequate warm-up is a light sweat
warm up adequately to allow the body to adapt to changes in the weather; an indication of an adequate warm-up is a light sweat
 if advised by the doctor, take medication 5–10 minutes before exercise
if advised by the doctor, take medication 5–10 minutes before exercise
Two different types of warm-up have been shown to be effective in reducing EIA:
During exercise advice
 If asthma develops during exercise, stop the athlete and have them take their reliever medication.
If asthma develops during exercise, stop the athlete and have them take their reliever medication.
 Do not allow the athlete to resume activity until all the signs and symptoms have subsided.
Do not allow the athlete to resume activity until all the signs and symptoms have subsided.
Diabetes
Types of diabetes
There are two main types of diabetes:
1. Type 1 diabetes – it is believed that this is an autoimmune condition where the insulin cells in the pancreas fail. This condition typically presents before the age of 30 years and usually early in childhood. Type 1 diabetics require insulin replacement via injection, pen or pump to survive.
2. Type 2 diabetes – this is the most rapidly increasing medical condition in the world. It more often affects people over the age of 40 years and accounts for around 85% of all cases of diabetes. Lifestyle factors (lack of exercise and obesity) are the biggest contributing factors in developing type 2 diabetes. This condition may be controlled with diet, exercise and oral medication, but may require insulin-replacement therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree