Closed Reduction and Percutaneous Pinning of Supracondylar Fractures of the Distal Humerus in the Child
Amy L. Mclntosh
INTRODUCTION
Supracondylar fracture of the distal humerus is the most common and problematic elbow fracture that occurs in children. It accounts for 3% of all pediatric fractures and occurs at an annual rate of 177.3 per 100,000 children (1,2). It occurs from a fall usually from a height greater than 2 feet. In a review of 391 supracondylar fractures admitted to Children’s Hospital in San Diego over an 8-year period, 29% of the injuries occurred in falls from school playground equipment (3).
INDICATIONS/CONTRAINDICATIONS
Classification
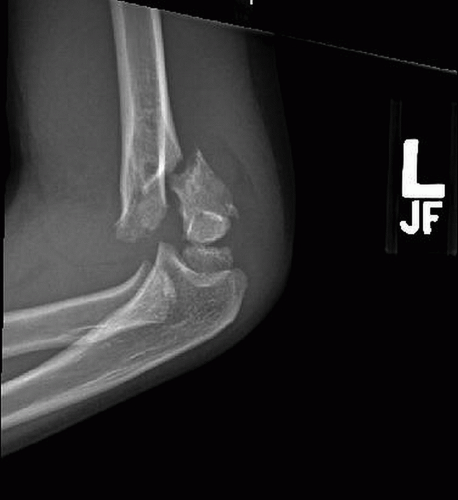
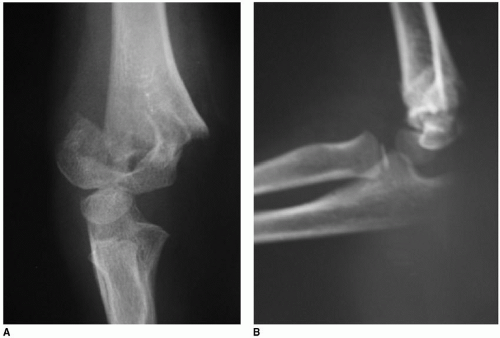
Appropriate treatment is determined by the type of fracture. Extension-type supracondylar fractures, which constitute 98% of the supracondylar fractures, occur from a fall onto an outstreched arm. This places the elbow into a hyperextended position where the olceranon acts as a fulcrum and the forces propagate across the medial and lateral columns of the distal humerus until they fracture. In this type of fracture, the distal fracture fragment is posterior (Fig. 2-1). Flexion-type supracondylar humerus fractures only constitute 2% of fractures. They result from a fall onto a flexed elbow. The distal fracture fragment is anterior (Fig. 2-2), and they are associated with a higher rate of ulnar nerve injury, increased need of open fracture reduction, and open ulnar nerve decompression (4).
Supracondylar fractures of the humerus were originally classified by Gartland in three types (5). Type I fractures are nondisplaced, type II fractures have an intact posterior hinge, and type III fractures are completely displaced with disruption of both the anterior and posterior cortices. Mubarak and Davids subclassified the Gartland I fracture into A and B subtypes (6).
Type IA: Nondisplaced Often the fracture line is difficult to see. The diagnosis of nondisplaced fracture is made by the clinical examination, which reveals tenderness, both medially and laterally, over the distal humeral condyles. Though radiographs may show no cortical disruption, a posterior fat pad sign is often present (7). With this fracture, the diagnosis is often not confirmed until 3 weeks after injury, when radiographs will show callus formation. The preferred treatment of a nondisplaced supracondylar fracture of the humerus is a long-arm cast, elbow flexed to 90 degrees or less for 3 weeks.
Type IB: Minimally Displaced/Medial Compression This minimally displaced fracture must be evaluated carefully to avoid underestimating the degree of deformity, which can lead to subsequent cubitus varus (8). If the radiographs reveal compression (torus) or collapse of the medial column, closed reduction may be required. The carrying angle of the contralateral, uninvolved elbow should be carefully checked. Children with little physiologic valgus (10 degrees or less) are at particular risk for developing an unsightly cubitus varus deformity.
These fractures should be taken to the operating room, where the alignment of the extremity can be more fully examined. It is often necessary for a closed reduction and percutaneous pinning using two 0.062 smooth K-wires via a lateral approach to be performed.
Wilkins modified the Gartland type II fractures by dividing them into A and B subgroups (9).
Type IIA: Hyperextension/Posterior Cortex Intact On the lateral radiograph, these fractures demonstrate extension of the humeral/capitellar relationship without rotation.
Type IIB: Displaced/Angulated with Osseous Contact The displaced/angulated with osseous contact fracture demonstrates both rotational and hyperextension deformity radiographically, but some cortical contact remains, usually on the posterior side.
Both types IIA and IIB of supracondylar fractures require general anesthesia, closed reduction, and percutaneous pin fixation with two lateral pins in the operating room. Type IIB is more difficult to reduce than is IIA and requires correction of the angulation and rotation.
Type III: Completely Displaced All type III fractures require general anesthesia, closed reduction, and percutaneous pin fixation with three lateral entry pins or two lateral entry and one medial entry pins.
Type IV: Multidirectional Unstable These fractures are unstable in both flexion and extension because of complete loss of a periosteal hinge. They occur either as a result of trauma or by excessive flexion force during a closed reduction maneuver (10).
Indications for a closed reduction and percutaneous pin fixation of a supracondylar humerus fracture include any IB, II, or III type fracture. Basically, any fracture that requires a closed reduction should undergo percutaneous pin fixation for the following reasons:
It provides immediate stability of the fracture fragments.
It allows the patient to be cast in a long-arm cast with 90 degrees of flexion or less, and decreases the risk of future compartment syndrome and Volkmann contracture.
Contraindications for closed reduction and percutaneous fixation include the following:
Open fracture. Usually, the proximal fragment will perforate the skin anteriorly through the brachialis muscle, creating a grade I open fracture. These are best treated by an extension of the laceration, debridement of the fracture fragments, and reduction and internal fixation of the fracture fragments. Care must be taken not to injure the anterior neurovascular structures during the fracture reduction and stabilization.
Irreducible fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree