Fig. 2.1
Flexion deformity of the distal interphalangeal (DIP) joint: the mallet finger
An eccentric axial load to the tip of the finger causing the distal interphalangeal (DIP) joint to forcefully hyperflex or hyperextend can disrupt the continuity of the insertion of the conjoined lateral bands onto the dorsal aspect of the distal phalanx . This avulsion may take the form of tendon avulsion off the dorsal lip of the proximal end of the distal phalanx or an intra-articular fracture of the dorsal lip may occur with the bony fragment still attached to the terminal extensor (Fig. 2.2 ). The dorsal fragment’s size and degree of articular involvement may vary from a fleck of bone to 70–80 % of the joint surface. Any joint involvement greater than 50 % is generally associated with volar subluxation of the DIP joint (Fig. 2.3 ) .
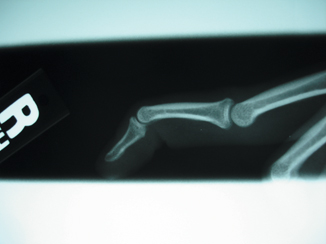

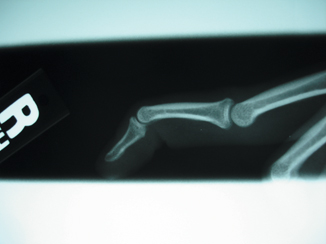
Fig. 2.2
Lateral X-ray of tendinous avulsion of the terminal extensor on the distal phalanx. Note the hyperextension of the proximal interphalangeal joint (PIP)

Fig. 2.3
Displaced mallet fracture involving 60 % of the articular surface. Note the volar subluxation of the distal phalanx
With the flexor digitorum profundus (FDP) tendon unopposed, the tip of the finger will assume a flexed posture. Initially thought of as a “jammed finger” of minor importance, it is frequently ignored. The characteristically flexed posture of the distal phalanx is usually detected immediately but sometimes may only manifest after several weeks once the swelling has subsided. Patients that seek medical attention within 2–3 weeks of injury can usually be treated nonoperatively. Others may wait up to 3 or 4 months after the full extent of the disability become manifest such as DIP joint pain, erythema, skin breakdown, DIP flexion contracture, swan-neck deformity, and difficulty in navigating tight spaces such as a back pocket. While it is possible to commence nonoperative treatment, these may fail to correct the deformity and thought must be given to surgical correction [4] .
Alternatively, there are patients who have undergone conservative treatment for 3–4 months only to find that the flexion deformity has persisted or recurred. In those patients, there have been weak or incomplete reattachment of the tendon end back to bone and the connection may be nothing more than a thin, transparent scar bridge with the tendon having retracted more than 3 mm ([5]; Fig. 2.4). This proximal retraction of the extensor hood causes increased tension on the central slip attachment on the middle phalanx causing proximal interphalangeal joint (PIP) hyperextension resulting in a secondary swan-neck deformity.


Fig. 2.4
Terminal extensor tendon. Note the loose scar bridge that connects the end of the tendon to the distal phalanx. Insufficient tension across the bridge will lead to a chronic mallet
Epidemiology
It has been reported that the incidence of mallet finger injuries is 9.89/100,000. The peak age for the injury is young to middle-age men and older women with males outnumbering females by 3/1 [6]. Wehbe and Schneider in 1984 reported that 74 % of these injuries occurred in dominant hands and 90 % of these injuries occurred in the ulnar three digits [7]. Simpson et al. (2001), showed that mallet deformities accounted for 2 % of all sporting injuries mainly rugby, football, and basketball [8].
Mechanism of Deformity
The terminal extensor tendon is a flat and thin structure measuring on the average 1.1 mm and inserts on the distal phalanx up to 1.2 mm distal to the joint margin and 1.4 mm proximal to the germinal nail matrix. The terminal extensor tendon is adherent to the underlying dorsal aspect of the DIP joint capsule. The terminal tendon is formed by the confluence of the radial and ulnar lateral bands. Just proximal to this confluence lies a thin membrane that runs transversely between the lateral bands called the triangular ligament. These prevent volar subluxation of the lateral bands. Injury to this ligament can result in the formation of a boutonniere deformity . The oblique retinacular ligaments (ORLs; Landsmeer) are thin fibers that run deep and volar to the lateral bands and they coordinate PIP and DIP flexion and extension. They originate from the lateral flexor sheath and form the outer margin of the terminal extensor tendon at the DIP joint.
The lateral bands are continuations of the interosseous and lumbrical tendons that run along the sides of the digit at the proximal phalanx. Dorsal subluxation of the lateral bands such as what is seen in swan-neck deformities is prevented by transverse retinacular ligaments that run from flexor tendon sheath dorsally to the volar rim of the lateral bands.
The central slip tendon is a continuation of the extensor digitorum communis to the finger and runs up the middle of the proximal phalanx. It connects to the lateral bands via the sagittal band fibers that run transversely and through oblique fibers that connect to the lateral bands distal to the PIP joint [5, 9] (Figs. 2.5a, b).
Fig. 2.5
a Lateral view of the extensor mechanism. Note the relationship between the central slip and the oblique retinacular ligament (ORL; With permission from Jessica Rose Waterman). b Coronal view of the extensor mechanism; note the relationship between the central slip, lateral bands, and terminal extensor (With permission from Jessica Rose Waterman)
Schweitzer and Rayan found that the excursion of the terminal extensor tendon at the DIP joint was 1–2 mm when the joint was moved passively from full extension to full flexion [10]. They also found that PIP joint angle of flexion had significant influence on the degree of possible DIP joint flexion. If the PIP was flexed 90°, the maximal DIP flexion was 82°, whereas if the PIP was extended, the maximal DIP flexion possible was 51°. If the terminal tendon is sectioned via “Z” lengthening, it was found that 1 mm of lengthening allowed 25° of flexion. Two millimeters of lengthening allowed 36°. Three millimeters of lengthening allowed 49° and four millimeters of lengthening allowed 63° of flexion. They also found variation between each of the palmar digits with the middle finger flexing the most for each millimeter of terminal tendon lengthening. They showed that if the cut tendon end retracted more than 1 mm proximally, it was extremely difficult to approximate the tendon end to its insertion. These data illustrate what occurs when the terminal extensor tears and retracts allowing the DIP to develop an extensor lag which persists even after the gap between tendon end and bony insertion is bridged by a scar and forms the basis of the conservative treatment of these injuries.
Classification and Diagnosis
If neglected, permanent fingertip disfigurement can result from mallet fingers , as well as dorsal DIP pain and inflammation, restricted DIP flexion, and swan-neck deformity. Prompt treatment of the injury can alleviate the risk of a scar bridge laxity of 1 mm between the terminal extensor tendon and the distal phalanx, which in turn leads to a 25° extensor lag.
To date, there have been no classification systems that refer to mallet deformities that involve tendon avulsions only. The existing ones either describe mallet “fractures” or mixed bony and tendinous injuries together ([7, 11]; see Tables 2.1 and 2.2).
Table 2.1
Webhe and Schneider’s classification system of mallet fractures based on injury severity [7]
Type 1 | No DIP joint subluxation |
Type 2 | DIP joint subluxation |
Type 3 | Epiphyseal and physeal injuries |
Subtype 1 | Less than 1/3 of the articular surface |
Subtype 2 | 1/3–2/3 of the joint surface |
Subtype 3 | > 2/3 of the joint surface |
Type 1 | Closed or blunt trauma with loss of tendon continuity with or without a small avulsion fracture |
Type 2 | Laceration at or proximal to the distal interphalangeal joint with loss of tendon continuity |
Type 3 | Deep abrasion with loss of skin, subcutaneous cover and tendon substance |
Type 4A | Transphyseal fracture on children |
Type 4B | Hyperflexion injury with fracture of the articular surface of 20–50 % |
Type 4C | Hyperextension injury with fracture of the articular surface greater than 50 % with early or late volar subluxation of the distal phalanx |
Clinical Evaluation
After obtaining a history of a crush, axial load, or even a trivial fingertip “stub” on a bed sheet or a carpet surface, one observes the resting posture of the DIP and PIP joints. The extensor lag and whether it is passively correctable should be noted as well as any hyperextension of the PIP joint. The dorsal skin integrity should be checked for lacerations, abrasions, erythema, and tenderness (Figs. 2.6a, b). Though the injury occurs at impact, the deformity may not manifest for several days [12]. This may be due to the fact that the initial injury to the tendon may have been incomplete but with repeated stress the remaining insertion may attenuate or avulse from the distal phalanx.
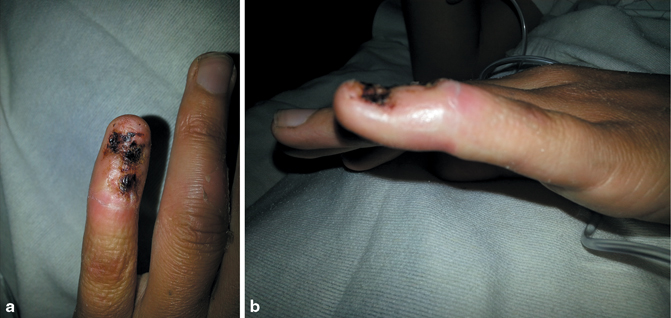
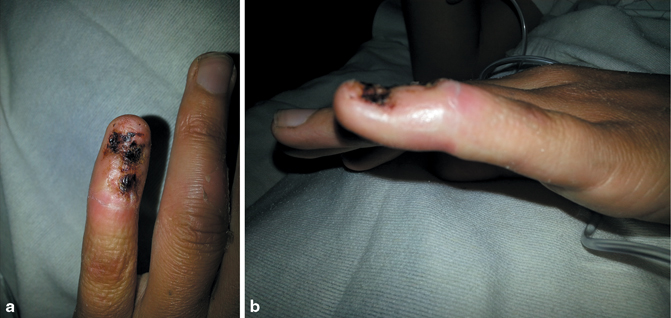
Fig. 2.6
a, b Crush avulsion injury to the tip of the fifth finger involving the terminal extensor. Note the loss of the dorsal skin and nail apparatus
X-ray assessment should include AP, lateral, and oblique views and the DIP should be evaluated for fracture, displacement of fragments, volar subluxation of the distal phalanx, and DIP joint congruity.
Nonoperative Treatment of Mallet Deformity
The goal of all closed treatment of mallet deformity whether purely tendinous or with a bony avulsion is the apposition and reattachment of the terminal extensor to the distal phalanx allowing full extension and correction of the flexion deformity. In pure tendon avulsions, this needs to be accomplished without the development of DIP flexion contracture, extensor lag from gapping between the tendon end and its insertion, and adhesions between the tendon end and the dorsal capsule of the DIP joint preventing active or passive DIP flexion. One must achieve a delicate balance between sufficient immobilization in extension and allowing careful active flexion to achieve gliding between the extensor tendon and joint capsule. If the immobilization period is too short, tendon rupture will occur [13].
There is some controversy whether only the DIP joint should be immobilized in extension or should DIP and PIP joints be splinted, the latter in flexion thus relaxing the terminal extensor hood and ORL [14]. Katzman in 1999 in a cadaveric study repeatedly flexed and extended the PIP and found no increased tension on a created gap at the DIP insertion. Thus, the only DIP extension needed was to preserve apposition of the extensor tendon to its insertion [15]. Others feel that it is necessary to keep the PIP flexed to allow the distal extensor mechanism to be “pulled” distally and thus relax the insertion site [16]. DIP extension alone is the more commonly used conservative approach. Typically, full-time splinting for 6 weeks followed by 2–6 weeks of part-time splinting usually at night or for strenuous activities has been accepted as the standard protocol for nonoperative treatment of mallet fingers [8].
Review of the Literature
Mason reported the first treatment of mallet finger in 1930. He advocated for quick surgical intervention of closed mallet fingers [17]. Similarly, Smillie designed a plaster splint to hold the DIP in hyperextension with the PIP joint in flexion [18]. Hallberg et al. in 1960 reported on 127 patients with mallet finger treated in a plaster cast and noted that half the patients had a poor result with a residual deformity of > 20° [19]. In 1962, the Stack splint (Fig. 2.7e) was devised, which made conservative treatment of mallet fingers more popular [20]. In 1975, Pulvertaft in an address to the British hand society said that: “60 % of mallet fingers had satisfactory results after splinting and that a further 20 % would improve sufficiently in the course of time” [21]. Seven years later, Auchincloss compared external splinting to surgical care for acute closed mallet fingers in 41 patients [22]. He found no difference in outcome and further opined that there was no need to splint at all after a period of 6 weeks.
Today, the overall opinion in the field is that that initial treatment of closed mallet fingers should be nonoperative, in a full-time splint that keeps the DIP joint in mild hyperextension (< 10°) for 6–8 weeks, followed by a 4-week period of part-time nocturnal splinting (Fig. 2.7). Evans et al. wrote that at the end of 6 weeks during the first week of immobilization, no more than 20–25° of flexion should be allowed [16]. A flexion-blocking splint would be helpful at this point. If no extensor lag develops, 35° of flexion can be permitted the following week. Patients can be allowed to flex the DIP 10–20 times, several times daily, until full flexion is allowed. If an extensor lag develops, splint again in full extension for 2 weeks then begin the process again.
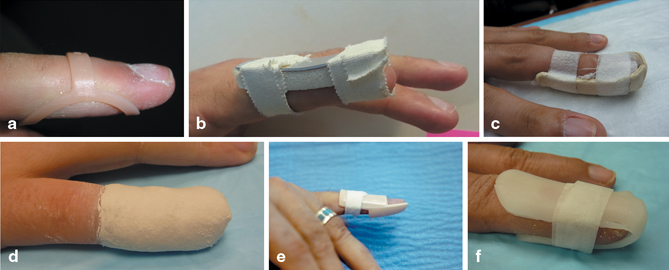
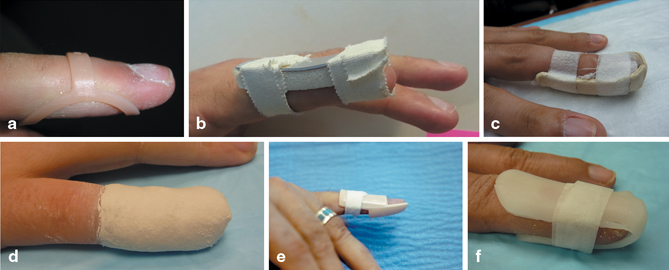
Fig. 2.7
Commonly used external splints used for the closed treatment of mallet fingers a, b Top: Oval-8 splint, dorsal AlumaFoam splint c, d Middle: Volar “cradle” splint, plaster cast e, f Bottom: Stack splint, custom coaptation splint
Patients need to be told that conservative treatment may leave them with a residual flexion deformity of 5–10°, a mild loss of DIP flexion and the presence of a dorsal “bump” (Fig. 2.8). A second 6-week round of splinting can be tried. In the past, some advocated splinting as late as 3 months post presentation [23].


Fig. 2.8
Dorsal “lump” of the distal interphalangeal (DIP) joint from a chronic untreated mallet finger. There is a secondary swan-neck deformity of the proximal interphalangeal joint (PIP)
However, there is controversy about the best way to splint. Most of the techniques reported used the following Crawford’s criteria to assess functional outcome of treatment [24]:
Excellent:
Full DIP extension, full flexion, no pain
Good:
0–10° of extension deficit, full flexion, no pain
Fair:
10–25° of extension deficit, any flexion loss, no pain
Poor:
> 25° of extension deficit or persistent pain
Abouna and Brown’s criteria [12]
Success:
Extensor lag < 5°, no stiffness, normal flexion, and extension
Improved:
Extension loss 6–15°, no stiffness, normal flexion
Failure:
Extension loss > 15°, DIP stiffness, impaired flexion
In 1997, Okafor et al. documented of 31 patients treated in a thermoplastic “Stack” splint for an average of 7.2 weeks [25]. They were followed for a mean of 5 years with a delay in treatment from 0 to 28 days. Of the 29 patients without fracture , or fractures less than 30 % of the joint surface, the delay in treatment had no significant effect on the outcome with regard to DIP motion or extension deficit. However, at follow-up at 6 months, 35 % of the patients had and extensor lag of > 10° and had a flexor range of 48°. Also, 35 % of those studied were mallet fractures and of those, half had degenerative changes at the DIP joint. In this series, swan-neck deformity developed far more commonly in mallet fractures than pure tendinous injuries. However, in this series, 90 % were satisfied with their results and 68 % noted no functional impairment in the finger . There was, however, a greater impairment of DIP joint flexion in patients with osteoarthritis (OA) though the presence of OA had no effect on extensor lag.
Garberman’s study showed that with similar splinting regimens, there was no difference between early (< 2 weeks) and late presentation (> 4 weeks) in terms of final outcome. Both groups had < 10° extensor lag at final follow-up at 2–6 months [26]. There was, however, a significant positive correlation between the length of splinting and final extension deficit. Patients with an intra-articular fracture had a higher incidence of degenerative changes on X-ray than those who were purely tendinous mallets. There were no complications reported in this series.
Kinninmouth and Holburn in a randomized prospective study of 54 patients compared a custom molded perforated splint to a stack splint (Fig. 2.7). Perforated splints were better tolerated and had better results according to Crawford’s criteria with less extension lag [27].
Tocco et al. in 2013 compared cast immobilization to a removable DIP orthrosis (Fig. 2.7) in 57 patients where patients were given detailed instructions in home self-care with close monitoring for compliance [28]. Follow-up was at 28 weeks. Those patients treated in a cast had an average extensor lag of 5°, whereas the orthotic group had a 9° lag. One of the factors observed was edema of the fingertip at final follow-up. Those that were edematous had a poorer outcome than those that were not. This could be due to diminished arterial, venous, and lymphatic flow to the edematous fingertip [29]. Casting allowed constant compression on the fingertip and not surprisingly had diminished edema than the other group. Colditz attributed “edema reduction” to be one of the salutatory effects of plaster casting of limbs [30]. There was no difference in active flexion between the two groups at follow-up. At 6 months, there was no difference between the two groups and both had a 5° extensor lag at follow-up. Other variables such as time from injury to treatment, mallet type, or injury mechanism had no effect on the final outcome in this study.
Warren and Norris followed 116 patients, randomized to wear either a “Stack” or “Abouna” wire splint [31]. At 10 weeks, both splints were shown to be equally effective with either near or complete resolution of the mallet. Patients preferred the “Stack” splint, reporting that it was more comfortable. In a randomized trial with 60 patients, Maitra and Dorani compared the “Stack” splint with padded aluminum (Fig. 2.7) and found that, while both splints were equally effective in correcting the extensor lag, the aluminum splint was more comfortable and had less dorsal skin maceration than the “Stack” [3]. Skin maceration can be prevented by pre-wrapping the DIP joint in gauze or by padding the splint in moleskin. In 2010, Pike and Mulpuri in a prospective randomized double-blinded study investigated the following three splint types with 87 patients [32]:
Volar-padded aluminum splint
Dorsal-padded aluminum splint
Custom thermoplastic splint applied to the volar side
All splint types had the DIP in “slight” hyperextension and the PIP joint free. The splints were applied full time for 6 weeks and, if there was a lag of > 20°, to apply for an additional 4 weeks. The single, major complication was full-thickness skin ulceration from dorsal skin pressure. Additionally, there were several, minor complications with maceration and erythema. An extension lag of 5–10° in all groups was reported at follow-ups of 7, 12, and 24 weeks, but there was no statistical significance between the groups at 12 weeks.
In another randomized, controlled trial, O’Brien and Bailey compared the dorsal aluminum splints, custom circumferential thermoplastic splints, and “Stack” splints, which were followed up at 12 and 20 weeks [33]. Finger braces were worn continuously for 8 weeks. Patients wearing stack splints and aluminum splints (5/21 each) experienced skin maceration, problems with fit, pain, and splint breakage. The group that wore thermoplastic splints (22 patients) had no complications. All patients experienced excellent results by Crawford’s criteria extensor lag of 6.4° and a flexion range between 59 and 64°, and there was no difference between the groups at final outcome at 20 weeks.
Additionally, Handoll and Voghella conducted a meta-analysis on splint treatment and concluded that there was “insufficient evidence to determine which splint type is best but that the splint must be stout enough to withstand everyday use [2].”
There has been some discussion in the literature about the vascularity to the dorsal skin over the DIP joint relevant to blanching of that skin when the DIP is hyperextended and to potential pressure from a dorsally applied splint. Flint in 1955 described the vascularity of the dorsal skin of the DIP joint. The blood supply to the dorsal skin arises from dorsal branches arising from the volar digital arteries [34]. These dorsal terminal vessels form an arcade where the branches join. Hyperextension of the DIP joint causes blanching by stretching the volar arteries and compression of the dorsal arcades (Fig. 2.9a) by the buckling of the overlying skin (Fig. 2.9b). Rayan and Mullins in 1987 showed that skin blanching occurred when the DIP joint was hyperextended to 50 % of maximum in healthy volunteers, the average normal hyperextension being 28.3° [35]. That blanching can be reproduced when a tight dorsal splint is applied.
Fig. 2.9
a Lateral view of the finger with the dorsal and volar arterial distribution. Nail bed is to the right. Note the proximal and distal crossing arterial branches from the proper digital artery on the volar aspect (With permission from Jessica Rose Waterman). b Finger hyperextended against a firm surface. Note the blanching of the dorsal skin
The state of vascularity of the extensor attachment and possible healing potential may explain the apparent direct relationship between age and extensor lag seen by Pike and coauthors where patients older than 60 years had a distinctly poorer outcome than younger patients [32].
In light of the above, it is clear that when a removable thermoplastic splint is applied, it needs to be removed frequently for skin checks and cleaning at home but great care must be exercised not to allow the finger to flex during this period. Noncompliance with this program will result in failure of splinting. It is advised that the fingertip rest on a flat surface or pinch tip to tip with the thumb to prevent DIP flexion. Compliance rates have been reported to range from 50 to 70 % in closely monitored studies. While no splint type has been shown to be more efficacious than another, compliance with splinting regimens appeared to be greater with custom thermoplastic splints than AlumaFoam or stack splints [36]. The most important factor in success of splint treatment is patient compliance with the regimen.
Surgical Indications
There is a whole subset of patients that cannot be treated by splinting alone. They include patients who cannot tolerate splinting either because of repeated skin breakdown, recurrent loosening, or claustrophobia despite the type of splint chosen. Other groups such as surgeons, dentists, musicians, or competitive swimmers cannot afford to take off from their activity for 8 weeks and may opt for a percutaneous pin placed across the DIP joint in full extension and buried under the skin at the distal end of the finger . It acts as an internal splint and allows much earlier return to work activity but is prone to breakage and pin tract infection if misused. Thus, patient selection for this treatment must be made with care [37].
Open Mallet Fingers
There is little controversy in the literature about the treatment of lacerations and open avulsions at the terminus of the extensor mechanism . Zone 1 lacerations involving the terminal extensor should be directly repaired either to a terminal tendon stump with locking mattress suture which can include the skin or directly to the distal phalanx using a volar pull-out button or suture anchors [38]. Deep abrasions and skin/tendon avulsions should be first debrided and should be considered for secondary tendon repair after the wound has been rendered clean and there is adequate skin coverage. In this scenario, tendon grafting may be necessary to reestablish continuity. Postoperative regimen is similar to closed mallet fingers [39].
Complications of Treatment of Mallet Fingers
Chronic Mallet Fingers
In 2011, Makhlouf and Al-Deek reviewed the treatment of chronic mallet fingers in 11 papers. Mallet fingers are generally considered “chronic” when significant deformity (> 20°) exits after 12–16 weeks of closed treatment [40].
There have been ten methods of treatment in the literature:
(1)
Excision of scar and tenorrhaphy
(2)
Reattachment of the tendon back to the bone
(3)
Imbrication of the healed tendon (Fig. 2.10)
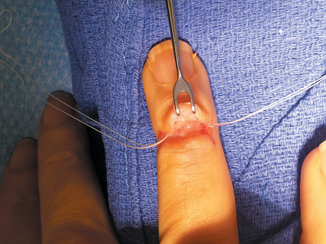
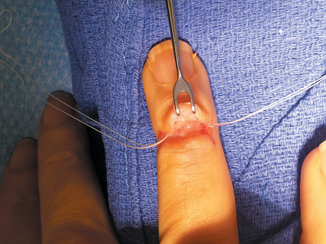
Fig. 2.10
Mitek anchors in distal phalanx securing the distal tendon and bridge drawing them both toward the distal phalanx
(4)
Tenodermodesis (Fig. 2.11)
Fig. 2.11
Tenodermodesis: The tendon avulsion is sutured into extension with the overlying skin. If there is any skin redundancy, it is excised as an ellipse
(5)
Fowler central slip tenotomy
(6)
(7)
Spiral oblique retinacular ligament reconstruction (SORL)
(8)
Arthrodesis
(9)
Tendon–bone graft
(10)
Bridge tendon graft inserted into a bone tunnel into the distal phalanx
Makhlouf tabulated the results of these treatments and showed the following: In the European literature, unless there is some hyperextension of the PIP joint, only the DIP joint is addressed [40]. The most frequently reported method is excising the tendon scar bridge and reattaching the tendon back to bone with an 80–100 % good to excellent result. In the US literature, Fowler releases are favored but not for extension deficits > 35° [39]. If there is a significant swan-neck deformity, a SORL reconstruction is favored. They also feel that poor results are directly related to:
1.
Delay in treatment > 4 weeks
2.
> 50° extensor lag
3.
Short thick fingers
4.
> 60-years-old
5.
Poor compliance
Fowler’s Central Slip Tenotomy (Fig. 2.12)
One of the simplest techniques for correction of chronic flexible tendinous mallet deformities is the central slip tenotomy. Described in 1949 by Fowler, the method is predicated on the concept that in the chronic phase of mallet deformity a scar bridge is developed between the tendon end and the distal phalanx [39]. A bridge that is a mere 3 mm too long has been shown by Schweitzer and Rayan and others can lead to a 45° extensor lag of the DIP [10]. The concept of the central slip tenotomy lies in the fact that the force exerted by the central extrinsic tendon in the finger is dissipated by its insertion at the base of the middle phalanx. There is not enough excursion in the lateral bands and ORL to extend the DIP. Sectioning the central slip allows the whole extensor apparatus to migrate 2–3 mm proximally, thus facilitating DIP extension.
It is also seen that sectioning the central slip may lessen the hyperextension moment in the PIP that can lead to secondary swan-neck deformity often observed in chronic mallet fingers.
Fowler’s central slip tenotomy is a reliable technique for reducing the degree of flexion deformity at the DIP joint but has generally not been advocated in deformities greater than 36° [39]. There have been concerns about aggressive tenotomy with subsequent injury to the triangular ligament creating a secondary extensor lag at the PIP joint and even frank boutonniere deformity. Classic papers on central tenotomy by Bowers, Hurst, and others have advocated a large mid-lateral approach, sectioning the transverse retinacular ligament lifting the extensor mechanism and releasing the central slip from below [41]. More recently, a limited approach utilizing a simple dorsal transverse incision 5 mm proximal to the PIP have been advocated [41].
Grundberg et al. reported a series of 20 patients who had their chronic mallet deformities treated with central slip tenotomies saw their extensor lag go from a pre-op average of 37–9° at final follow-up [4].
Chao and Sarwahi demonstrated in an experimental model that after sectioning the terminal extensor and creating a lengthening of about 3 mm, an extensor lag of 45° was created [42]. When a central slip tenotomy was performed in their specimens, they noted an immediate correction of 37–9°. Based on Schweitzer, that would be representing a proximal migration of 2 mm [10]. They concluded that correction greater than 36° was not possible utilizing this technique, although older clinical studies noted corrections of up to 60°. This could be due in part to remodeling of the terminal tendon. There may be no apparent correction immediately in the OR under anesthesia but correction of the DIP extensor lag can continue to improve at 1 year, something that the experimental model could not duplicate. It is clear, however, from these papers that full correction of the extensor lag was far less consistent with greater degrees of preoperative DIP flexion deformity.
Hiwatari et al. constructed an experimental cadaveric model of mallet finger in 16 fresh-frozen cadaveric fingers by sectioning and lengthening the terminal extensor so that a 45° mallet deformity was created [43]. A central slip tenotomy was created according to the technique of Bowers and Hurst [41]. The lateral bands were lifted after cutting the transverse retinacular ligaments from the center of the proximal phalanx to the center of the middle phalanx. The central slip was detached from its insertion on the dorsum of the middle phalanx and lateral band from the dorsum of the middle phalanx by one third, one half, and two thirds of the phalangeal length of the middle phalanx and the extensor lag of the PIP and DIP joints was measured. The mean pre-section DIP extensor lag was 44°. When one third was detached, the DIP lag was reduced to 19°. With one half detachment, the lag went down to 13° and when two third was cut, the lag went down to 6°. At the PIP joints, only four fingers demonstrated an extensor lag and that averaged 8° and no lag exceeded 15°. It is possible that no boutonniere deformity formed in this model because the transverse retinacular ligaments were also sectioned.
Rozmaryn described a technique where central slip tenotomy was augmented by a distal imbrication of the terminal extensor tendon and scar bridge to the distal phalanx by means of two microsuture anchors [44]. The tenotomy was performed through a minimally invasive transverse incision just proximal to the dorsal PIP crease. The fibers of the central slip were carefully separated from the lateral bands and 5 mm square of central tendon was excised. A separate transverse incision was made at the DIP joint and after two anchors were placed into the distal phalanx, the terminal extensor and scar bridge were brought up to the distal phalanx without sectioning the tendon or bridge. The DIP joint was secured in extension with a K-wire which was removed after 4 weeks and gentle active motion was begun. Thirty-nine patients underwent the procedure. The average pre-op extensor lag was 45° and post-op average was 6.7°. There was one failure with a residual 30° extensor lag. Pre-op PIP hyperextension averaged 18° and at post-op it was 4.8°.
Tenodermodesis
Excising the scar between the tendon and the bone as well as an ellipse of the dorsal skin and repairing both together using en bloc 2.0 nylon mattress suture with pin stabilization of the DIP for 6 weeks, can have a 50–90 % excellent result at 6 months. This procedure was first described by Brooks in 1961. The technique was further refined by Graner who introduced the DIP pinning to augment the postoperative splinting that Brooks recommended. Never published by the authors, it was not until Albertoni published the results in 1988 did this procedure become popularized as the Brooks–Graner procedure. He reported a 91.6 % satisfactory result using this method [45]. In the early 1990s, the procedure became popular not only treating chronic mallet fingers but even acute mallet fingers and even in children [46].
Kardestuncer, Bae, and Waters conducted a level IV study with 10 patients with > 45° ext lag. All were pinned for 6 weeks [47]. At 6.5 years follow-up, 2/10 full finger extension, 8/10 had a 20° extensor lag , and 7/10 had full DIP flexion. Iselin et al. reported on tenodermodesis in 26 patients and on final follow-up 22/26 had < 10° extensor lag [48].
Similarly, Kon et al. studied 27 patients and 26 had an arc of motion of 5–60° at final follow-up [49].
Sorene and Goodwin reported on 16 patients with a chronic mallet finger deformity after a mean of 26 weeks of failed conservative treatment with an average extensor lag of 50° [50]. At surgery, all had full passive range of motion (ROM) at the DIP joint. A third of the patients had 10° hyperextension of the PIP joint. At 36 months, the mean extensor lag was 9°. However, 6/16 had a lag of 20°. Average flexion was 30°.
Kaleli et al. added an external fixator for 5 weeks to the tenodermodesis technique to secure DIP extension while avoiding crossing the DIP [51]. At 36 months follow-up, the average extensor lag was 2° ( −7 to 13°) and the flexion average was 70° (20–90°).
Excision of Scar and Tenorrhaphy
Lind et al. reported on excision of scar and tenorrhaphy in 40 patients. At final follow-up, 16/40 achieved a full ROM [52]. Another eight had good results with < 8° extension lag but inability to flex more than 30°. The rest had extensor lags ranging between 30 and 60°.
Direct Reattachment of the Tendon to Bone
Ulkur in 2005 presented his results on 22 patients who had a direct reattachment of the tendon to bone via suture anchors [53]. All were diagnosed > 4 weeks out. In his technique, part of the scar bridge was maintained in order to reach the distal phalanx as the terminal extensor tendon had retracted proximally. The K-wire was removed at 2.5 weeks and active ROM exercise was begun. He had 15/22 excellent results with full ROM, 5/22 good with < 10° lag, and 2/22 had fair results with 10–20° extensor lag.
SORL Reconstruction (Littler)
This procedure has been recommended in the literature for swan-neck deformities that developed in the face of chronic mallet finger posture (Fig. 2.13). Originally described by Littler to regain the balance and synergy of PIP and DIP extension by reconstructing the function of the ORL correcting the DIP flexion deficit associated with PIP hyperextension [54].
Fig. 2.13
The Thompson modification of Littler’s spiral oblique retinacular ligament (SORL) reconstruction utilizing a free tendon graft anchored to the distal phalanx and passed volar to the axis of rotation of the PIP joint and anchored into the proximal phalanx. PIP proximal interphalangeal joint (With permission from JR Waterman)
Kleinman in 1984 reported that on 12 patients having undergone an SORL, 9 regained full DIP extension and three developed hyperextension deformity at the DIP [55]. One required tenolysis and one needed graft lengthening.
Thompson–Littler 1978 described a technique where the tendon graft was connected independently into the distal phalanx via a pull-out wire and volar button and proximally threaded under Cleland’s ligament between the neurovascular bundle flexor tendon sheath [54]. The graft was then passed transversely into a drill hole in the proximal phalanx mimicking the path of the lateral band described in Littler’s original description.
Kanaya et al. in 2013 reviewed Thompson procedure and reported on seven patients with chronic mallet deformity and the pre-op ext lag was 42° (35–50) [56]. At final follow-up, the DIP extensor lag was 4° (0–30). Post-op DIP flexion mean was 63° (45–85). At the PIP joint, post-op flexion was 91° (85–110°) and a mean of 5° hyperextension. They also reported that the result is independent of pre-op condition of the quality of the scar bridge as no attempt was made to address that.
There is some discussion in the literature as to the correct tensioning of the tendon graft vis-à-vis PIP and DIP extension. Thompson felt that the graft should be tightened so that by passively extending the PIP joint, the DIP would go into full extension as well. Kanaya et al. felt that doing so would over tighten the graft. They therefore recommended that the DIP be allowed into 5° flexion when the PIP is held in full extension so that full simultaneous flexion of the PIP and the DIP became possible [56].
Tendon Grafting
Gu and Zhu employed the technique of free tendon grafting in 27 patients with open lacerations and 40 patients who had failed 6 weeks of conservative treatment [57]. The tendon insertion was augmented by inserting a palmaris graft into a bone tunnel in the distal phalanx and proximally into the terminal extensor leaving the DIP in full extension against gravity. All but one had less than 10° of extensor loss and had virtually full DIP flexion.
Tendon–Bone Composite Grafting
Wang et al. in 2013 reported on 28 patients with failed closed mallet fingers with an average of 34° extensor lag [58]. They created a notch at the extensor insertion on the distal phalanx and inserted a tendon–bone composite graft from the medial half of the extensor carpi radialis brevis (ECRB) insertion. The bone was fastened to the distal phalanx with a preplaced polyprophylene suture and the tendon was attached to the terminal extensor with a 1.5 cm overlap. The DIP was pinned in extension for 4 weeks.
Bone healing was achieved at a mean of 5 weeks. At 15 months follow-up, no patient reported pain and the mean extensor lag was 4° and the average DIP flexion was 65°. Eighty-six percent of the patients had achieved excellent results by Crawford’s criteria.
Author’s Preference
For the reconstruction of a chronic mallet finger, my preference is to perform a central slip tenotomy first and see how much correction is evident under anesthesia. Assuming the correction is minimal, I imbricate the distal phalanx insertion and pin the DIP joint in full extension for 4 weeks. Following this, one can begin full active ROM but must be very careful not to remove too much of the central slip, or an extensor lag of the middle phalanx will result.
Mallet Thumb
Mallet thumb is an exceedingly rare injury (Figs. 2.14a, b). Robb reported on 149 mallet fingers and only one was a mallet thumb [59]. Wehbe and Schneider reported on 42 mallet fingers and only one and that too was a mallet thumb [7]. This could be the extensor pollicis longus (EPL) is thicker than any of the extensor digitorum communis (EDC) tendons in the digits and the thumb is shorter and stouter than the fingers which makes it more resistant to axial or hyperflexion forces.


Fig. 2.14
a Clinical appearance of a mallet thumb. Note the dorsal swelling over the DIP joint, b X-ray appearance of a mallet thumb. Note the avulsion fracture of the dorsal rim of the distal phalanx. DIP distal interphalangeal joint
Tabbai et al. reviewed the unique characteristics of mallet thumbs, which are anatomically based but will influence treatment [60]. Unlike the EDC in the palmar digits, the EPL lacks lateral bands, so if the insertion into the distal phalanx is interrupted, either by laceration or closed avulsion, the tendon would retract more than other digits (Figs. 2.15a, b). According to the author’s report, the tendon had retracted 1.4 cm and had infolded on itself. However, this has not been reported in mallet fingers involving palmar digits.
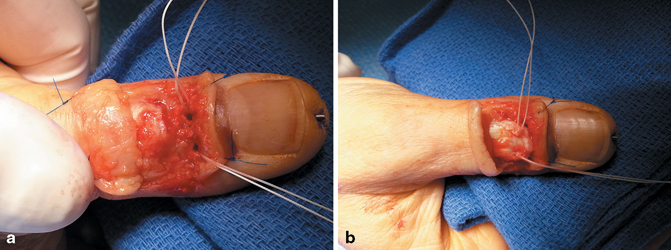
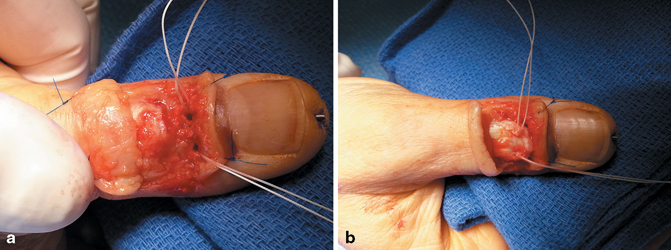
Fig. 2.15
a Open repair of a mallet thumb. With the thumb in full extension, the terminal end of the extensor tendon is retracted 8 mm. The bone anchor holes sit at the proximal verge of the distal phalanx. b The terminal extensor tendon has been mobilized and repaired back to the distal phalanx. There is a longitudinal 0.045 K-wire across the DIP joint. DIP distal interphalangeal joint
The mechanism of closed injury is the same as other digits with acute hyperflexion force against an extended thumb. Nevertheless, Miura et al. reported that 80 % of these injuries are open, and only 20 % are closed [61]. Patients are clinically unable to extend the interphalangeal (IP) joint from a flexed position, but these are distinguished from other, more proximal EPL ruptures by the presence of pain and swelling over the dorsum of the IP joint. They did feel along with several other authors the same year that the initial treatment of closed mallet thumbs should be nonoperative with immediate surgery reserved for open lacerations . They did advocate continuous splinting of the thumb IP in full extension for 6 weeks followed by 3–6 months of 12-h/day splinting .
Din and Meggit pushed for operative treatment of closed injuries, they noted a lack of reports of successful closed treatment [62]. Splint treatment cannot compensate for the significant proximal retraction of the EPL , and the terminal extensor of the thumb is stout, lending itself to suture placement. In 1975, Verdan was the first to advocate closed treatment for these injuries, stating that these injuries were no different from other digits [63].
The field is currently in agreement that primary repair and 6 weeks of splinting are appropriate in open injuries. However, closed injuries should be splinted for 6–8 weeks. There are no studies to date comparing open to closed treatment of closed injuries.
Tabbai recommends magnetic resonance imaging (MRI) evaluation of closed mallet thumbs, in order to assess the degree of retraction ([60]; Fig. 2.16). Traditionally, 1 mm of retraction has been used as benchmark for open repair, but there is no data to support this. Of course, if treatment fails, the option exists of attempting a closed treatment first and then operating .
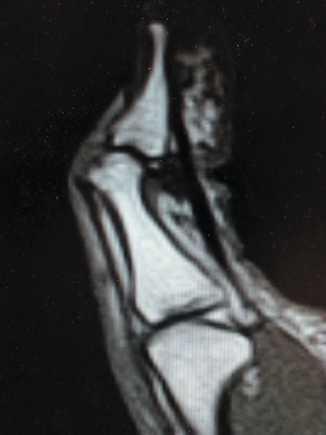
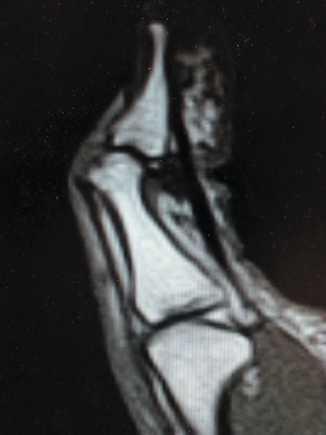
Fig. 2.16
MRI T-1 sagittal image of a mallet thumb. Note the degree of retraction of the extensor mechanism from the distal phalanx. There is also an oblique flexor pulley rupture in this patient. MRI magnetic resonance imaging
Nishimura et al. reported a case of a bony mallet thumb treated with an extension block pinning technique (see below) [64]. Pins were kept in for 4 weeks and splinting for 2 more weeks. At 7 months, patient’s ROM at the IP joint was 16–46°.
Mallet Fractures
Introduction
Most of the literature on mallet deformities written over the past 30 years combine the classification and treatment and outcome measures of tendinous mallet fingers and mallet fractures. While the clinical presentation may be similar, the mechanism of injury, treatment algorithm, and outcomes may vary. Both entities can be caused by a hyperflexion of the DIP but mallet fractures can be caused by hyperextension and axial loading which buckles the DIP joint into flexion as well. Zancolli reported that the degree of PIP flexion at the moment fingertip impact may play a role in whether the lesion at the tendon insertion is bony or tendinous [65]. He demonstrated that when the DIP joint is forcibly flexed beyond 90° when the PIP joint is in full extension, a bony avulsion occurs rather than a pure tendon avulsion .
Generally, mallet fractures whose bony components are less than 30 % of the joint surface behave like and can be treated as tendinous mallet deformities (Fig. 2.17). If the articular surface of the fractured dorsal fragment is greater than 50 % consideration must be given to the fact that while minimally displaced fractures will actually heal better than pure tendinous injuries with bone on bone contact (Fig. 2.18), displacement of the fragment on presentation with proximal migration of the dorsal fragment, if left untreated can be accompanied by volar subluxation of the DIP joint and if the joint surface is allowed to heal in an incongruous fashion, degenerative arthritis will in all likelihood occur (Fig. 2.19). In a cadaveric study, Husain et al. demonstrated that volar joint subluxation of the distal phalanx was not observed until the joint involvement in the fracture exceeded 43 % and was consistent beyond 52 % of the joint surface [66]. It is believed that the reason why volar subluxation occurs in these larger dorsal fragments is that the joint surface cannot support contact with the proximal phalanx head and that DIP collateral ligaments may play no role in stabilizing the DIP joint . Volar subluxation was defined in this study as displacement of the long axis of the distal phalanx on the axis of the middle phalanx > 7 % of the overall DIP joint surface of the distal phalanx (Fig. 2.20) .
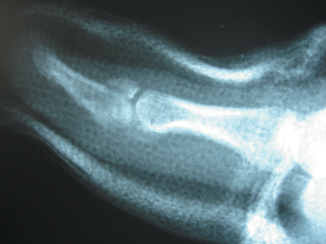
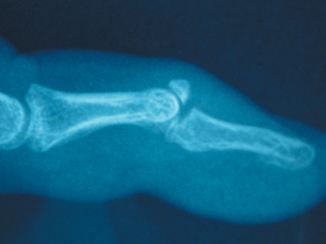

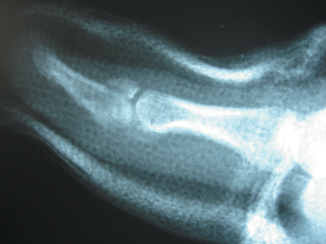
Fig. 2.17
Mallet fracture with 30 % of joint involvement and no displacement. This is treated like a tendon injury with immobilization for 6–8 weeks
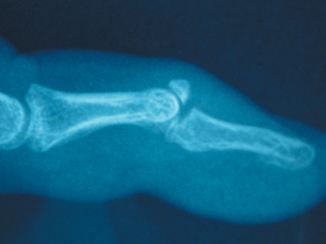
Fig. 2.18
Displaced mallet fracture involving 50 % of the joint surface. The distal phalanx is subluxated volarly

Fig. 2.19
Degenerative arthritis distal interphalangeal joint secondary to an untreated mallet fracture
Fig. 2.20
Joint subluxation of the DIP joint defined a volar drift of the distal phalanx equal to 7 % of the length of the total length of the articular surface of the distal phalanx. DIP distal interphalangeal joint (With permission from JR Waterman)
The Evidence: Review of the Literature
Nonoperative Treatment
Kalainov et al. studied the results of 21 patients who underwent nonsurgical treatment of closed displaced mallet fractures with greater than 30 % joint involvement using extension splinting for a mean of 5.5 weeks [67]. At 2 years follow-up, their patients had a high rate of satisfaction and finger function . He did note, however, that some patient developed dorsal DIP prominence, residual extension lag, DIP degenerative joint disease and swam neck deformity especially in cases of volar subluxation of the DIP joint. However, in this study, the fracture types were not broken down according to percentage of joint involvement past 30 % [67].
Nonoperative treatment of mallet fractures include “Alumafoam” splinting, plaster finger casts, Stack and Oval-8 splints, and custom-made Thermoplast custom fit orthrosis (Fig. 2.7). All of these interventions are designed to maintain full extension of the DIP joint so that the avulsed fragment can be reasonably be opposed to the main body of the distal phalanx. An anatomic reduction of the fracture is not necessarily expected, but rather just enough continuity of the extensor mechanism to allow full DIP extension. Patients frequently remain with a tender bony “bump” on the dorsum of the DIP joint.
Complications of closed treatment also include pressure sores, maceration, and skin necrosis on the dorsum of the DIP, which can be full thickness (Fig. 2.21). This results from the tenuous blood supply to the dorsal skin overlying the extensor tendon insertion. Dorsal skin ischemia can result from hyperextending the DIP joint even 5° or via direct pressure placed on the dorsal skin from a tight splint. Both can occlude the tiny dorsal crossing arteriolar branches emanating from the volar digital arteries [34].


Fig. 2.21
Full-thickness necrosis of the dorsal skin over the DIP joint from a wet thermoplastic splint that was never removed for several weeks. DIP distal interphalangeal joint
Additionally, recurrent flexion deformity and hyperextension contractures can occur. Any chronic malunions and resultant flexion deformities of more than 10° at the DIP will result in a secondary swan neck deformity and potentially degenerative changes in the DIP.
Treating mallet fractures is a highly controversial procedure. Wehbe and Schneider studied 160 patients with mallet injuries and have strongly advocated the nonoperative treatment of nearly all mallet fractures, with the exception of significant volar subluxation of the distal phalanx, on the head of the middle phalanx, and fracture involvement of > 30 % of the DIP articular surface [7]. The authors claim significant incidence of adverse outcomes when these injuries are treated surgically. They feel that even in the face of articular incongruity and volar subluxation, sufficient remodeling occurs to leave the patient with a pain-free functionally acceptable digit. Followed out to 3 years, however, 50 % of their patients were seen to have degenerative changes and stiffness in the DIP.
Geyman et al. conducted a meta-analysis of all studies of mallet fingers from 1966 to 1998 and found that in all tendinous mallet injuries and articular fractures < 30 % should be treated with splinting [68]. Surgery should be reserved for large displaced fractures that cause volar subluxation of the distal phalanx.
Weber and Segmüller published a series of ten patients with > 30 % of the articular surface, significant displacement of the dorsal fragment but without subluxation of the DIP joint [69]. They were all treated by splinting for 4–6 weeks. All showed excellent remodeling of the joint surface, normal DIP flexion and an extension lag of < 5°. Their conclusion was that secondary volar subluxation of the DIP joint only occurred if splinting was carried out incorrectly and that excellent results could be achieved by splinting alone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









