11. Clinical placement
Nick Southorn
• What you need to know before you get there122
• Uniform etiquette122
• What you need to know when you get there126
• The learning agreement128
• Marking criteria128
• The role of the clinical educator130
• The role of the academic tutor131
• Conclusion131
 |
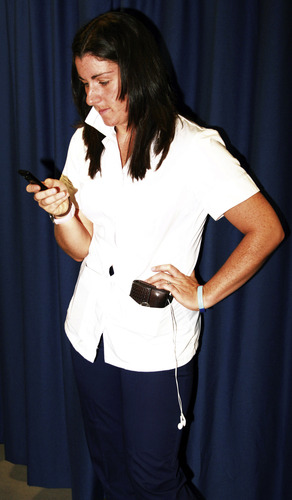
| Fig. 11.1. |
| Don’t panic! They don’t expect you to just start treating patients – you are a student, remember. |
Clinical placements are the most taxing part of your physiotherapy degree for a number of reasons: you are expected to put into practice what, in theory, you know from book reading, you will just be settling into your placement and you then have to rotate or it comes to an end, you are constantly “the student” and can feel as though you get under people’s feet, and you are generally shattered all the time! However, placements are the most valuable part too. You will be shocked at exactly how much you will learn from educators of all professions and patients from all backgrounds. Placements will open your eyes to the practicalities of being a physiotherapist and give you pure insight that you can’t read about in books. It is often said that only in clinical placements can you decide what area of this diverse profession you would like to work in. If you take one thing from this chapter, it should be that you should enjoy your placements and learn from them.
How to prepare
The best way you can prepare is to be well informed as to the nature of the placement. Don’t try to guess as you may find that you have missed the mark entirely. To do this, you should find out who is your clinical educator and give them a ring. Your university placement organizer will happily give you the information you need to contact them. Actually, most expect you to do this: it shows that you are a confident and conscientious student and is an easy way to make a good first impression. It helps if you have everything you need to say written down clearly in front of you; there is nothing worse than being asked your phone number and forgetting it! Make sure they know what placement number you are on, eliminating any possibility of error on their part. For example, if this is your first placement and they are expecting a third placement student, they are going to expect much more from you. This does happen and it is not a good start to placement number one! See below under “What you need to know before you get there” for starter questions. Although you have a list of questions written down, you should remember that you are having a conversation, i.e. don’t be too rigid in your structure, allow the conversation to flow and let them ask questions along the way too.
Usually your first placement, regardless of the area you are in, will be a test of your assessment technique. My most valuable bit of advice to you is to learn how to assess a patient thoroughly. This may sound easy but believe me, it isn’t as simple as that. A comprehensive assessment includes the impact of the pathology not only on the physical aspect but also on the functional (Activities of Daily Living) and the psychologic. Also, you need to understand the consequences of the answers you get quite quickly, e.g. if the patient has kidney failure, what implications are there for the musculoskeletal system or the blood pressure? If a patient presents with back pain and on assessment it appears has saddle anesthesia and urinary incontinence, what do you do? These are all very important and, luckily, usually specific to a particular clinical area.
When you do find out what type of patient you are likely to see, it is imperative that you learn how to assess them as this will save you a lot of time and earn you lots of brownie points! You need to discover the medications the patient is taking and for what (e.g. a beta-blocker could be for migraines as well as for hypertension) and diurnal patterns, etc. Each bit of information is important in making a diagnosis. As for the objective assessment, look at everything that has been done – blood tests, X-rays and so on – to give yourself a full picture. You won’t be expected to develop a completely clinically reasoned explanation for the findings immediately but if you have a basic understanding for each individual test, that is a good start. It is usually a good idea to get a group of friends together and use each other as patients; it’s a much better way of learning than auscultation on a pillow! If you are playing the part of the patient then you also get to describe how your colleagues are doing. Always remember that in the “role play” setting as well as the clinical setting, you should always gain informed consent from your friend/the patient.
You should also prepare your social life too. Unlike other university students, you are about to have no time at all! Clinical placements are all-encompassing and are severely detrimental to your social life. You get up early, have about 30 minutes for lunch (during which you are reading) and by the time you get home you are completely knackered but still have more reading to do! It is therefore important to always make time to see friends and family at weekends, evenings, etc. You have to switch off and give your poor brain a rest otherwise you will not last the duration. Make sure that someone on your course prepares a “pre-placement party” to blow off steam before you all disappear.
What you need to know before you get there
OK, so you are about to ring your clinical educator: what are you going to ask? Here are a few generic questions that may help you.
• What time do you want me to arrive? Take this time and make it 15 mins earlier. Being late is a big no-no.
• Do you have any specific uniform guidelines, i.e. shirt, tie and trousers or tracksuit?
• Are there any changing facilities available in the unit/hospital? Also ask about lockers/secure storage of kit.
• What type of patients do you see?
– Conditions?
– Length of stay?
– Typical rehab/treatment (physio/medical/others)?
– Other professional members involvement (assistants/OTs/podiatrists/doctors, etc.)
• Do I need any specialist equipment?
– Goniometer
– Stethoscope
– Swimming trunks/costume, etc.
• Should I do any preparatory reading on the area? You should always do some but they may have some specific ideas as to what they expect you to read.
• Are there any information leaflets that I can have about the area? Each area usually has written information available for students.
You are obliged to ensure that all entries into medical records are countersigned by a qualified member of staff. Remember that no matter how good you are, you are a student and therefore should never be in a position where you feel unsupported by qualified staff. If you don’t know the answer to something, the worst thing to do is keep it quiet. Now is your opportunity to ask questions and be sure of the answers. Always be safe and just think ahead of time about what you are about to do and you’ll be just fine. You will naturally learn where the fine line is between being independent and autonomous, and dangerous practice – you will also always strive never to cross that line.
Uniform etiquette
You may not have used it since your interview but now the iron has to re-emerge. Not all physio students follow this principle but having an ironed uniform makes the world of difference. Your uniform should be clean and tidy as once you walk into the hospital or clinic, you become a representative of your school, your profession and yourself; you should strive to make a good impression at all times. It is always a good idea to travel to your placement in your civilian clothes and change once you are there, even if you are expected to wear a shirt and tie. Hospital infection is a major issue and one that should be taken very seriously by everyone, from visiting relatives to the chief executive. Ensure that a name badge is seen at all times as per the local policy. Hair should be tied up if necessary – this is something that all physios should adhere to; it only needs to happen once for you to know why. I’m told that having a patient swing from a pony tail when they are heading floorwards is not a nice experience! You will have found out what the uniform policy is before you get there if you are organized and that is what they will expect from you. If you try to “bend” the rules by wearing something that resembles the uniform but isn’t, then you can expect a stern talking to.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree