Clinical development and progression of coronary heart disease
Pamela Reynolds
Introduction
Globally, cardiovascular diseases (CVDs) were the number one cause of death (30%) in 2008. CVDs include: coronary heart disease, cerebrovascular disease, peripheral artery disease, congenital and rheumatic heart disease, deep vein thromboses and pulmonary embolisms. In low- and middle-income countries, CVDs are disproportionately high, at about 80% of all deaths; and they affect men and women equally. By 2030, it is projected that deaths from CVD will remain high and continue to be the single leading cause of death. About 45% of CVD deaths are due to coronary heart disease (WHO, 2013). The purpose of this chapter is to detail the causes and clinical implication of coronary heart disease (CHD), which are diseases that affect the blood vessels of the heart. The other CVDs are addressed separately in other parts of this text.
CHD can begin early in the young adult and become progressive until it becomes clinically evident in middle to late adulthood (Watchie, 2010). Recognition of early subclinical onset of CHD was discovered by Enos and colleagues in 1953. They autopsied 300 apparently healthy soldiers killed in the Korean War and found 77.3% of them had visible blockages in their coronary arteries. As a result of this work, the medical community now differentiates coronary artery disease (CAD) from coronary heart disease (CHD). In CAD, there are obstructions that limit blood flow in the coronary arteries, however, not enough to significantly impair the function of the cardiac muscle. The term CHD indicates not only that there is obstruction in the coronary arteries, but also permanent damage to the cardiac muscle, limiting its function (Hillegass et al., 2011).
Myocardial ischemia results from a deficient blood supply to the heart muscle because of either obstruction or constriction of the coronary vessels. Underlying this deficiency is an imbalance between the oxygen supply and demand of the myocardial muscle cells. The majority of diseased coronary arteries have fixed obstructions in the form of atherosclerotic lesions that lead to chronic stable angina symptoms. When blood flow becomes more restricted, angina symptoms increase in frequency and intensity leading to acute coronary syndrome (ACS). Clinical presentations of ACS include sudden death, unstable angina leading to an acute myocardial infarction, which are classified by the presence or absence of specific ECG changes in at least two leads. These changes are classified as either ST elevation myocardial infarction (STEMI) or a non-ST elevation myocardial infarction (non-STEMI or NSTEMI) (Watchie, 2010; Hillegass et al., 2011).
However, ischemia can also be caused by spasms of the coronary artery walls, also known as Prinzmetal’s angina. Both atherosclerosis and vasospasms are equally capable of reducing the supply of blood and therefore of oxygen to the myocardial muscle cells. Hypertension can also damage the coronary arteries.
Ischemia produces major changes in two of the important functions of a myocardial cell: electrical activity and contractility. Alteration in electrical activity generates many of the electrocardiogram (ECG) arrhythmias. Impairment of myocardial contractility affects the function of the left ventricle and results in a reduced ejection fraction (the amount of blood pumped out with each heartbeat) and decreased cardiac output, which further compromises the blood supply to the coronary arteries.
Causes of coronary artery disease
The Framingham Heart Study has led to the identification of risk factors and acceptance of their role in the development and progression of CVD (Wilson et al., 1987). Risk factors for developing coronary heart disease are discussed in Chapter 39. The most significant and modifiable risk factors in the causation and acceleration of atherosclerotic disease are cigarette/tobacco smoking, hypertension, hypercholesterolemia and physical inactivity. Nicotine increases the sensitivity of low-density lipoprotein (LDL) receptors and increases the levels of fibrinogen circulating in the blood. Persons who quit smoking can reduce their risk of developing CAD by half in 1 year. In 15 years, risk for CAD is equalized with nonsmokers (Goodman, 2009). Hypertension appears to be an independent risk factor in the development of CAD. Efforts to lower blood pressure have been more effective in reducing stroke morbidity and mortality than in decreasing heart attacks (Hillegass et al., 2011). When total blood serum cholesterol level reaches more than 200 mg/dl a person is at greater risk for heart disease. The risk doubles when cholesterol exceeds 240 mg/dl and the ratio of total cholesterol to high-density lipids (HDL) exceeds 4.5 (Goodman, 2009). The Centers for Disease Control and Prevention report that physical inactivity is the most prevalent risk factor for developing CHD (Hillegass et al., 2011).
Heredity, gender and age are non-modifiable risk factors. Some other factors that may influence development of CHD include body habitus (obesity), diet, hyperglycemia, diabetes mellitus, stress and personality type. Also, more recent studies indicate that male gender is no longer considered to be a differentiating risk factor. Male risk is higher until females reach menopause, then the risk is equal (Hillegass et al., 2011). Atherosclerosis and vasospasm causes of CHD are detailed further in this chapter.
Atherosclerosis
Coronary arteries have three layers. The outer layer or adventitia provides the support for the artery and is composed primarily of collagen fibers. The middle layer or media has multiple layers of smooth muscle. As demand for blood flow in the coronary arteries changes, this muscular layer is able to make adjustments in the diameter of the vessels. The intima or inner layer is comprised of endothelium and variable amounts of collagen, elastic fibers and some isolated smooth muscle cells (Hillegass et al., 2011).
Development and progression of atherosclerosis is a complex process in which lipid deposits are irregularly distributed in the intima and endothelium layers of the larger and medium coronary arteries. The arterial endothelium is especially permeable to macromolecules the size of low-density lipoprotein (LDL). Fatty streaks in the intima layer of the artery are the first clinical evidence of atherosclerosis. These lesions contain lipid-laden macrophages and smooth muscle cells. Eventually the accumulation of lipid-laden macrophages grows so large that the endothelium stretches and begins to separate, leading to cell injury; and bearing the intima and underlying connective tissue to the circulation. Platelets then accumulate around this injured area and a thrombus is formed, which is the sclerotic element of the atherosclerotic lesion. The arterial walls continue to thicken through the buildup of lipids, macrophages, T lymphocytes, smooth muscle cells, extracellular matrix, calcium and necrotic debris. The growth of the atherosclerotic plaques and thickening of the arterial walls are responsible for the narrowing of the blood vessel, which ultimately leads to end organ ischemia (Goodman, 2009; Cassady & Cahalin, 2011; Hillegass et al., 2011).
The clinical outcomes of atherosclerosis can be improved by removing or reversing a single or group of risk factors. In particular, alteration of diet, reduction of blood cholesterol levels, treatment of hypertension and cessation of smoking are the major targets to prevent the progression of atherosclerotic disease. Physical activity has been shown to reduce the negative effects of some of these factors. Exercise allows an individual to attain or maintain a higher metabolic rate, which allows better caloric intake tolerance – one can enjoy a few more calories without gaining weight. Reduction of blood cholesterol and blood pressure along with successive reductions or elimination of reliance on blood pressure-lowering medications are other benefits of exercise (ACSM, 2010). The general rehabilitation exercise considerations presented in Chapter 39 are all applicable to individuals with atherosclerosis.
Vasospasm
Prinzmetal’s angina is an atypical or variant angina that causes myocardial ischemia and chest pain. It is a variant angina in which there is a transient increase in vasomotor tone or vasospasm. It occurs primarily at rest and often without any precipitants. Unlike the other types of angina, the exercise capacity in those with variant angina is preserved. There is also a tendency for the pain to occur at about the same time each day. Arrhythmia or conduction disturbances may accompany episodes of this variant angina. Considering that up to one-third of variant angina sufferers have no atherosclerotic disease of the coronary vessels, the current theory of pathogenesis is this variant angina is caused by the vasospasm of one or more of the coronary arteries. Vasospasms are not isolated to variant angina; they are also seen in individuals with typical angina and acute myocardial infarction (AMI). Unlike other forms of angina, an episode of variant angina actually causes ST-segment elevation on an ECG. Similar to typical angina, Prinzmetal’s again can be quickly relieved by nitroglycerin or other vasodilators (Cassady & Cahalin, 2011; Hillegass et al., 2011).
Clinical course of coronary heart disease
Sudden death
Sudden cardiac death is death that occurs within an hour of onset of symptoms of the initial presentation of acute coronary syndrome. Frequently, a patient with CHD is diagnosed during an autopsy for a sudden unexplained death. Sudden cardiac death occurs in about 40% of patients with CHD (Watchie, 2010; Hillegass et al., 2011).
Chronic stable angina
The term ‘angina pectoris’ describes paroxysmal or spasmodic chest pain, which is usually caused by myocardial ischemia. It is typically precipitated by exertion or excitement. Stable angina is characterized by episodic chest pain that usually lasts for 5–15 minutes, is provoked by exertion or stress; and is relieved by rest or sublingual nitroglycerin. The pain almost always has a retrosternal component and commonly radiates into the neck, jaw and shoulders and down the left or the left and right arms. Radiation to the back is also possible. Additional symptoms, such as lightheadedness, palpitations, diaphoresis, dyspnea, fatigue, nausea or vomiting, may accompany the pain. Females and elderly individuals are more likely to present with atypical symptoms. The specific ECG changes seen with ischemia are usually indicated by ST-segment depression of more than 1 mm, which also occurs in about 50% of cases during an acute attack (Goodman, 2009; Hillegass et al., 2011).
Acute coronary syndrome (ACS)
The term acute coronary syndrome is used to describe a patient who presents to the emergency room with symptoms of either unstable angina or an evolving AMI. This diagnostic terminology was adopted to expedite patient management; and decrease myocardial damage and associated morbidity and mortality. Patients with ACS are classified in one of three categories: unstable angina, ST elevation myocardial infarction (STEMI) or a non-ST elevation myocardial infarction (non-STEMI or NSTEMI).
Unstable angina
Unstable angina represents a clinical state between stable angina and AMI. It is also referred to as crescendo or preinfarction angina. The clinical definition of unstable angina includes any of the following subgroups: (i) exertional angina of recent onset, usually within the past 4–8 weeks (which means that all newly diagnosed angina is essentially unstable); (ii) angina of worsening character, either with increasing severity of pain, increasing duration of pain, increasing frequency of pain or increasing requirement for nitroglycerin; and (iii) angina at rest. Also included within this group of unstable angina is postinfarction angina, which, as its name suggests, occurs after an AMI. It is important to remember that it can occur within days or weeks of an acute infarction or even months to years later (occurring after an angina-free period dating from the AMI). Those who experience angina after successful coronary artery bypass surgery comprise another group of individuals who are considered unstable. Unstable angina is thought to be caused by a progression in the severity and extent of coronary atherosclerosis, coronary artery spasm or bleeding into non-occlusive plaques in the coronary artery. It eventually results in complete occlusion of the artery (Grimes, 2007; Hillegass et al., 2011).
Acute myocardial infarction (AMI): stemi and non-stemi
Insufficient blood flow to an area of the myocardium for longer than 20 minutes will evoke symptoms of an acute myocardial ischemia or infarction. The vast majority of people with AMI have CHD, but there is no universal agreement about exactly what precipitates the acute event. Current concepts concerning the immediate cause of AMI include the interaction of multiple trigger factors: progression of the atherosclerotic process to the point of complete occlusion; hemorrhage at the site of an existing, narrowing coronary artery embolism; coronary artery spasm; and thrombosis at the site of an atherosclerotic plaque (American Heart Association, 2005).
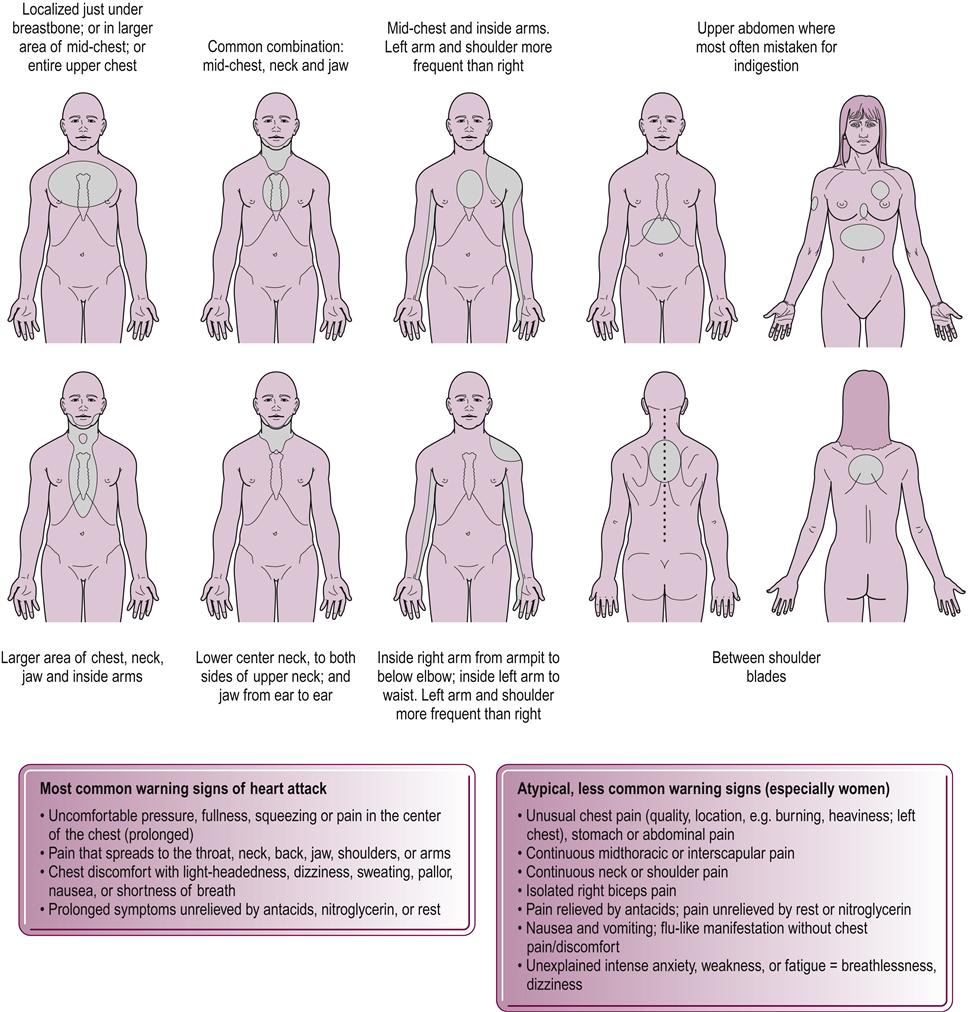
The classic symptom of AMI is retrosternal chest pain, which is usually the same as angina pain but lasts for more than 15–30 minutes. Individual variation in the site and radiation of the pain, and also in the nature and severity of the pain, is very common (Fig. 40.1). Associated features such as dyspnea, diaphoresis, palpitations, nausea and vomiting are common accompaniments but not all are present all of the time. The degree of heart muscle damage and extent of infarction is usually independent of the presence of associated features or the severity of the pain. A long duration of pain often indicates more damage. AMIs in elderly patients, as opposed to those in younger individuals, are likely to present with no pain or with a noncardiac type of pain or altered mental status. Longitudinal studies indicate that up to 25% of myocardial infarctions are not recognized clinically but are diagnosed later in routine ECGs performed for unrelated conditions. In addition, individuals with diabetes are more susceptible to silent (painless) myocardial infarction (Goodman, 2009; Watchie, 2010).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







