Sciatic neuropathy is the second most common neuropathy of the lower extremity and a common cause of foot drop. This article reviews the anatomy, clinical features, pathophysiology, and electrodiagnostic assessment of sciatic neuropathies. There are multiple potential sites of pathology, determined in part by the mechanism of insult, including trauma, compression, masses, inflammation, and vascular lesions. Diagnosis is augmented by careful electrodiagnostic studies and imaging to help distinguish sciatic neuropathy from other sources of pathology. Electrodiagnostic studies may also help in assessing for early recovery and in determining prognosis.
Key points
- •
Sciatic neuropathy is the second most common neuropathy of the lower extremity.
- •
Sciatic neuropathy often presents with foot drop, mimicking common fibular neuropathy.
- •
The hip is the most common site of sciatic nerve injury.
- •
Trauma and masses account for most of the pathology leading to sciatic neuropathy.
- •
Electrophysiologic studies can help localize the lesion.
- •
Neuroimaging can sometimes identify an abnormality in more severe cases.
Introduction
Sciatic neuropathy is the one of the most common neuropathies of the lower extremities, second only to common fibular (peroneal) neuropathy. One of the most common presentations of sciatic neuropathy is foot drop. Because ankle dorsiflexion weakness, with or without lower extremity sensory impairment, may also be associated with several other clinical syndromes, a careful evaluation is necessary before confirming a diagnosis of sciatic neuropathy. Electrodiagnostic testing is of great value in confirming the diagnosis of suspected sciatic neuropathy and assessing the potential for recovery of nerve function.
Introduction
Sciatic neuropathy is the one of the most common neuropathies of the lower extremities, second only to common fibular (peroneal) neuropathy. One of the most common presentations of sciatic neuropathy is foot drop. Because ankle dorsiflexion weakness, with or without lower extremity sensory impairment, may also be associated with several other clinical syndromes, a careful evaluation is necessary before confirming a diagnosis of sciatic neuropathy. Electrodiagnostic testing is of great value in confirming the diagnosis of suspected sciatic neuropathy and assessing the potential for recovery of nerve function.
Anatomy
The sciatic nerve is the longest and widest single nerve in the body, originating just distal to the lumbosacral plexus and extending distal branches into the feet. It is responsible for most of the function of the lower extremity. It is derived from several lumbosacral nerve roots and the lumbosacral plexus. A minor branch of L4 combines with the ventral ramus of L5 to form the lumbosacral cord or trunk. The lumbosacral trunk descends over the sacral ala and combines with the ventral rami of S1, S2, and S3 and a branch of S4 to form the sacral plexus. The sciatic nerve forms the sacral plexus apex, located anteriorly to the sacroiliac joint and the piriformis muscle ( Fig. 1 ).
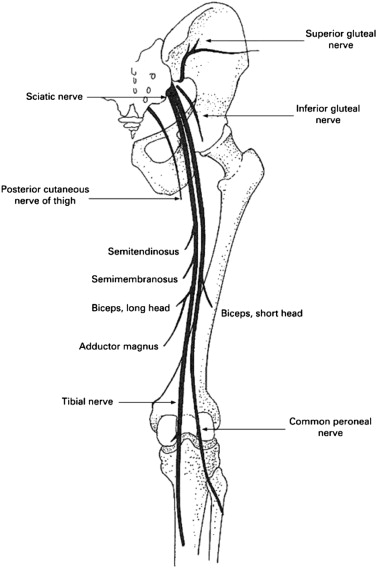
The sciatic nerve comprises the lateral division, which eventually forms the common fibular nerve, and the medial division, which forms the tibial nerve, each separately encased from the outset. After arising at the exit of the superior and inferior gluteal nerves, the sciatic nerve leaves the pelvis via the sciatic notch, typically through the greater sciatic foramen, and is accompanied by the posterior femoral cutaneous nerve, inferior gluteal artery, pudendal vessels and nerves ( Fig. 2 ). There is a close relationship to the piriformis muscle, which also exits the pelvis via the greater sciatic notch. The sciatic nerve usually travels under the piriformis muscle, except in 10%–30% of cases, notably when the fibular division passes through or above the piriformis muscle.
Distal to the piriformis muscle, the nerve is covered by the gluteus maximus muscle and soft tissue. The nerve then travels halfway between the bony landmarks, greater trochanter laterally, and ischial tuberosity medially, and then descends into the subgluteal area. From there, it runs posteriorly in the midthigh, remaining dorsal to the adductor magnus and ventral to the long head of the biceps femoris. The tibial division of the sciatic nerve innervates the hamstring muscles (semimembranosus, semitendinosis, and long head of the biceps femoris) and the adductor magnus in the thigh. In the thigh, the common fibular division innervates the short head of the biceps femoris.
The nerve divides into the common fibular and tibial branches approximately 6 cm above the popliteal fossa crease. The tibial nerve then continues posteriorly in the midline to the calf, innervating the muscles of the posterior compartment of the lower leg and supplying sensation to the posterior calf and lateral foot by the sural nerve (which also has a limited contribution from the common fibular nerve), the sole of the foot by the medial and lateral plantar nerves, and the heel by the medial calcaneal nerve. After passing through the upper popliteal fossa, the common fibular nerve travels laterally and around the fibular head, dividing into the deep fibular and superficial fibular branches, which supply the muscles of the anterior and lateral compartments of the lower leg, respectively. The superficial fibular nerve also forms a sensory branch that supplies sensation to the anterolateral lower leg and dorsum of the foot while the deep fibular nerve supplies sensation to the webspace between the first and second toes.
Presentation
Sciatic neuropathy often presents with foot drop. Patients often experience abrupt pain radiating down the posterolateral limb, with weakness and numbness evolving more gradually. In sciatic neuropathy, the clinical findings are often more consistent with injury to the common fibular division rather than tibial division, sometimes mimicking a common fibular neuropathy at the knee. This finding is particularly true of more distal lesions, as they may not affect the flexors of the knee, or of less severe sciatic nerve injury. Because the common fibular division has fewer and larger fascicles and less supportive tissue compared with the tibial division, it is thought to be more vulnerable to compression. Also, the common fibular division is more taut, and secured at the sciatic notch and fibular neck, resulting in greater potential for stretch injury.
In milder cases at the hip or thigh, the following features are typically noted:
- •
Foot drop that may mimic a common fibular neuropathy at the knee
- •
Weakness in knee flexion, ankle plantar flexion, ankle inversion
- •
Normal or decreased ankle jerk
- •
Pain and sensory loss in the foot and possibly the lateral shin
In severe lesions, these signs and symptoms are common:
- •
Weakness in ankle dorsiflexion and plantar flexion and toe extension and flexion
- •
Hamstring weakness
- •
Decreased ankle jerk
- •
Dysesthesic pain and numbness in the sole and dorsum of the foot and lateral lower leg
Electrodiagnostic studies
Electrodiagnostic testing (EDx) is helpful in localizing the site of injury and the severity of the lesion. EDx studies are also useful for assessing both recovery and prognosis. Standard nerve conduction studies for evaluation of the sciatic nerve include testing the following:
- •
Ipsilateral common fibular and tibial motor nerve conduction and minimum F wave latencies
- •
Superficial fibular and sural sensory nerve conduction
- •
Comparison with the unaffected leg
Findings on motor nerve conduction studies most commonly include reduced fibular compound muscle action potential (CMAP) amplitudes often with a normal tibial CMAP amplitude. Given the depth and size of the sciatic nerve proximally, it is not possible to obtain reliable studies with more proximal stimulation using standard techniques. Tibial H reflex studies may be normal in fibular-predominant lesions, and therefore may not confirm the diagnosis or help localize the site of injury. In sensory nerve conduction studies, reduced superficial fibular and sural sensory nerve action potential amplitudes are seen in most cases ( Table 1 ). Similar abnormalities are found in different age populations. In one study of patients with sciatic neuropathy, nerve action potential amplitudes were reduced in the fibular motor nerve of 80% of adults and 83% of children; tibial motor nerve of 52% of adults and 67% of children; sural sensory of 71% of adults and 79% of children; and superficial fibular sensory of 83% of adults and 60% of children. Minimum F wave latencies in adult patients with sciatic neuropathy were abnormally prolonged in 85% of fibular and in 57% of tibial nerve studies.
| Nerve | Latency | Amplitude | Velocity | F Wave |
|---|---|---|---|---|
| Common fibular motor | ||||
| Ankle | NL | Reduced | Abnl a | |
| Below fibular head | NL | Reduced | NL | |
| Above fibular head | NL | Reduced | NL | |
| Tibial motor | ||||
| Ankle | NL | NL to reduced | NL/Abnl a | |
| Knee | NL | NL to reduced | NL | |
| Sural sensory | NL | NL to reduced | NL | |
| Suprfl fibular sensory | NL | NL to reduced | NL | |
a F wave abnormalities include prolonged latency or decreased persistence.
To maximize the yield for identifying signs of active denervation, needle electromyography should generally be performed 3 to 4 weeks after onset of symptoms. Positive sharp waves and fibrillation potentials can be identified reliably only after this period, initially in muscles closer to the lesion and then in those more distal, with reinnervation occurring in a similar pattern. In sciatic neuropathy, any muscle in the foot and lower leg is likely to show denervation. Commonly tested muscles include the extensor digitorum brevis, tibialis anterior, tibialis posterior and gastrocnemius. In general, however, needle EMG abnormalities in sciatic neuropathy are more commonly seen in fibular-innervated muscles (94%–100% of patients) than tibial-innervated muscles (74%–84% of patients). Muscles innervated by the sciatic nerve in the thigh that often show denervation, depending on the site of the lesion, include both the short and long heads of the biceps femoris, semimembranosus, and semitendinosis.
In addition to studying muscles innervated by the sciatic nerve, the examiner should also study muscles that share the same root innervation but are supplied by a nerve other than the sciatic, such as the gluteus medius or tensor fascia latae (superior gluteal nerve) and the gluteus maximus (inferior gluteal nerve) to exclude L5 or S1 radiculopathy and lumbosacral plexopathy. To rule out a length-dependent process, such as a peripheral neuropathy, the electromyographer should also compare distal with proximal muscles of the leg, including those muscles in the proximal leg not supplied by the sciatic nerve. For example, the examiner could compare the extensor hallucis longus muscle (supplied by the sciatic nerve) with the vastus medialis muscle (supplied by the femoral nerve). Paraspinal muscle abnormalities of the lumbosacral spine on needle examination support a diagnosis of lumbosacral radiculopathy rather than sciatic neuropathy or a superimposed additional site of neuropathic injury.
Performed together, nerve conduction studies and needle electromyography can detect subclinical involvement of the tibial nerve and thereby exclude a common fibular mononeuropathy, for example, by showing involvement in the gastrocnemius or hamstring muscles. It is important to recognize that more distal tibial-innervated muscles, such as the gastrocnemius, tibialis posterior, and flexor digitorum longus, are more likely to show denervation than the hamstring muscles in chronic lesions, because the hamstring muscles may have had adequate time to reinnervate.
Imaging techniques
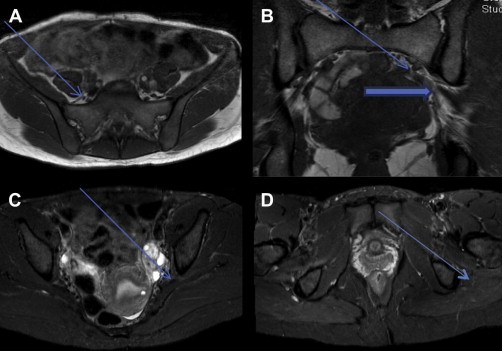
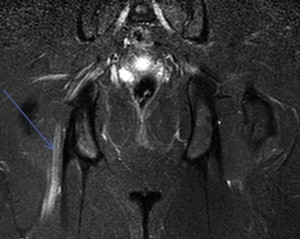
Magnetic Resonance Imaging
Of all imaging techniques, magnetic resonance imaging (MRI) seems to be the best technique to identify sciatic nerve pathology. Depending on the severity of the injury, T2-weighted magnetic resonance images may show high signal intensity in the nerve fibers or increased nerve dimension, deformation of the nerve, or total loss of nerve integrity. Short tau inversion recovery (STIR) sequences of the nerve help identify the extent of a lesion, with a more diffuse area of high signal indicating an inflammatory etiology ( Fig. 3 ). Chhabra and colleagues found higher nerve-to-vessel signal intensity ratios and higher incidences of T2 hyperintensity, nerve enlargement, and abnormal fascicular shape in affected nerves compared with normal nerves, with excellent interobserver and intraobserver reliability. Affected muscles showed more fatty infiltration, edema, and atrophy. However, findings on MRI may sometimes be difficult to interpret, because abnormal signal may occasionally be seen in normal individuals on both T2 and STIR imaging.
Other
Computerized axial tomography is helpful in finding lesions that impact the sciatic nerve involving bone (eg, sacrum fracture), vessel abnormalities (eg, aneurysm), or hematoma. Ultrasonographic studies have limited utility in the diagnosis of sciatic neuropathy and have been used more frequently for sciatic nerve blocks rather than to identify sciatic nerve pathology. However, a few recent studies have tried to use ultrasound scan to foster a greater understanding of the causes of sciatic nerve injury. For instance, Moayeri and Groen and Brull and colleagues, with the use of specific ultrasonographic settings, found more neural than nonneural tissue in the hip region than in the thigh, which might contribute to the greater proximal vulnerability of the sciatic nerve.
Etiologies
Different conditions can lead to sciatic neuropathy ( Table 2 ). In one retrospective study of individuals referred for electrodiagnostic evaluation of sciatic neuropathy, hip trauma and surgery were the most common etiologies. Sciatic neuropathy has been reported in as many as 1%–3% of patients after total hip replacement surgery. The neuropathy is usually discovered immediately postoperatively and is typically a consequence of stretch injury. The next most common causes include external compression and open injuries, such as gunshot wounds and knife injury, and ischemia, which may occur secondary to vasculitis or atherothrombosis or after bypass surgery. Endometriosis, iatrogenic nerve injection, and compartment syndrome are also less commonly reported causes. Not infrequently, a cause cannot be identified (ie, idiopathic sciatic neuropathy). An etiology for sciatic neuropathy was uncertain in 16% in the series reported by Yuen and colleagues of 73 patients. Vascular malformations may also uncommonly lead to sciatic neuropathy as a consequence of nerve compression.








