Clavicle fractures are common, and they comprise close to 3% of all fractures seen in fracture clinics. Midshaft fractures account for approximately 80% of all clavicle fractures and are the focus of this article. In carefully selected cases primary plate fixation of displaced midshaft clavicle fractures improves outcome, results in earlier return to function, and reduces the nonunion and symptomatic malunion rate significantly compared with nonoperative treatment.
Clavicle fractures are common, and they comprise close to 3% of all fractures seen in fracture clinics. Midshaft fractures account for approximately 80% of all clavicle fractures and are the focus of this article. Distal clavicle fractures are next most common, consisting of 15% of clavicle fractures, and medial third fractures are the least common, making up 5% of injuries. Distal third and medial third fractures are distinct entities and have a separate set of features requiring different approaches to imaging, diagnosis, and treatment compared with middle third fractures.
Traditionally, even widely displaced midshaft clavicle fractures have been treated nonoperatively based on several large studies that demonstrated excellent functional outcome with various methods of closed reduction and nonoperative treatment. In the past, most of the controversy surrounded the optimal method (if any) of nonoperative treatment, with various investigators supporting simple sling treatment, figure-of-eight bandaging, or other types of external support. Operative methods were deemed to have a high complication rate and little role in the primary treatment of fractures. The nonunion rate after nonoperative treatment was described as being approximately 1%, even in widely displaced fractures, and malunion was described as being of radiographic interest only.
However, recent studies have reported significantly different outcomes with regard to completely displaced fractures of the clavicle. Studies that have used patient-based outcome measures (as opposed to the more traditional surgeon-based or radiographic outcomes) have described an unsatisfactory outcome rate of 25% to 31%. Multiple comprehensive, prospective studies have clearly shown the nonunion rate in this setting to be up to 21%, exponentially higher than previously reported. In addition, a significant number of patients with malunited fractures have ongoing symptomatology with orthopedic, neurologic, and functional cosmetic deficits in a characteristic pattern; it would appear that clavicular malunion is a distinct clinical entity.
There are multiple potential explanations for the increased rate of poor outcome including survival of critically injured trauma patients with more severe fracture patterns, increased patient expectations of having a normal shoulder after injury, comprehensive follow-up (including patient-oriented outcome measures), and excluding children (with their inherently good prognosis) from analysis.
These findings spurred further investigation into comparative studies examining the role of primary operative fixation (usually consisting of compression plating or intramedullary nailing) in the treatment of displaced midshaft fractures of the clavicle. These comparative investigations including those examining different methods of closed treatment, operative versus nonoperative treatment, and different methods of operative fixation are the focus of this evidence-based medicine article.
Treatment options
Although a variety of treatment options have been described for the treatment of midshaft fractures of the clavicle, they can be summarized in 3 main types: nonoperative, open reduction and internal fixation with a plate, and intramedullary pin fixation (through either an open or closed reduction technique). These options, and the articles supporting them, are described in the following sections.
Nonoperative
Nonoperative care is the treatment of choice for most fractures of the clavicle shaft, especially those that are minimally displaced or undisplaced or those that occur in elderly, ill, noncompliant, or sedentary individuals in whom the risk of surgical intervention is too high or the potential benefit is too low. There have been multiple different techniques and devices described to obtain and maintain a satisfactory nonoperative reduction of a displaced midshaft fracture of the clavicle. However, there is little or no convincing evidence that any significant improvement can be made to the original position of the fracture in most cases, and one must typically accept the displacement seen on injury films. Although some temporary improvement in alignment may well occur with various techniques, such as the figure-of-eight bandage (traditionally popular in North America), there is little evidence that this device can maintain a closed reduction of a displaced clavicle fracture.
Currently, immobilization with a simple sling until the patient is comfortable enough to begin a gradual return to preinjury activities is the commonest nonoperative treatment choice. A randomized trial by Andersen and colleagues examined the functional and radiographic results after the use of a figure-of-eight bandage versus a simple sling for the treatment of displaced midshaft fractures of the clavicle. They found no significant difference between the 2 groups at final follow-up in either radiographic or functional outcome. Also, patients preferred the sling (2/27 dissatisfied with sling versus 9/34 dissatisfied with figure-of-eight bandage, P = .09). For this reason, it is reasonable to consider nonoperative treatment groups in comparative studies as one homogenous group in terms of outcome, despite the fact that there may be some differences in the type of nonoperative therapy used.
The results of nonoperative treatment were previously thought to be satisfactory in most cases, but modern studies with patient-based outcome measures have revealed significant deficits. Hill and colleagues reported a high degree of residual patient dissatisfaction after nonoperative treatment of displaced midshaft clavicle fractures using a patient-based outcome tool. They found a nonunion rate of 15%, and overall 31% of patients were dissatisfied with their outcome. In a study examining 225 clavicle fractures, Nordqvist and colleagues described good results after long-term follow-up with 185 good, 39 fair, and only 1 poor result. It should be noted that in the subcategory of displaced, comminuted fractures 27% of patients rated their shoulder as fair and this corresponds to the dissatisfied group (31%) in Hill’s study. Nowak and colleagues reported that 46% of 208 patients treated nonoperatively had shoulder sequelae at 9- to 10-year follow-up. In a study from the fracture group in Edinburgh, Robinson and colleagues reported on a prospective, consecutive series of 868 patients with clavicle fractures, 581 of whom had a midshaft diaphyseal fracture, and described a nonunion rate of 21% in displaced comminuted midshaft fractures. Brinker and colleagues analyzed the data from that article and suggested a nonunion rate of 33% for displaced comminuted fractures in men.
What is clear from these articles is that a significant percentage of young active patients with displaced midshaft clavicle fractures treated nonoperatively will develop symptomatic nonunion or malunion. These patients complain of a short, droopy, ptotic, asymmetric shoulder with orthopedic (weakness, rapid fatiguability), neurologic (thoracic outlet), and functional cosmetic (difficulty wearing backpacks, straps, etc) symptomatology.
Open Reduction and Plate Fixation
Open reduction and plate fixation of displaced midshaft fractures of the clavicle using modern precontoured implants and techniques has been well described with a high degree of success and low complication rate. Older reports of operative fixation that described a high failure rate and an unacceptable level of complications were plagued by selection bias (only the worst, comminuted, open fractures received surgery), poor soft-tissue handling, and fixation methods (cerclage wires or short, weak plates) that could reasonably be described as suboptimal by modern standards. Modern studies have reported significantly improved results after plate fixation. Smith and colleagues reported union in all of the 30 cases treated in this manner in a prospective trial, Collinge and colleagues reported union in 39 of 42 cases treated with anterior/inferior plating, and Poigenfürst and colleagues reported excellent results in 122 consecutive cases treated with superior plating. The operative group in the randomized clinical trial performed by the Canadian Orthopaedic Trauma Society (COTS) reported only 2 nonunions out of 62 cases treated with plate fixation. Although there are disadvantages with this technique including plate prominence (and subsequent hardware removal) and potential wound complications from the dissection required, in most modern series the incidence is low. In addition, precontoured anatomic plates are now available that minimize local irritation and decrease the need for hardware removal. A careful 2-layer (deltotrapezial fascia/platysma muscle and skin/subcutaneous tissue) closure can decrease the incidence and morbidity of potential infection. Although it remains controversial, antero-inferior placement of the plate has been advocated as a means of decreasing local irritation (as well as avoiding neurovascular structures while drilling).
Intramedullary Pin Fixation
Various retrospective reviews describe various methods of intramedullary pinning of the clavicle. The main intrinsic difficulty is that of trying to perform intramedullary fixation of a curved bone with a straight intramedullary device. The theoretical advantages of this technique are many and include minimal soft tissue dissection at the fracture site, less soft tissue prominence of the hardware, and a reduced refracture rate when compared with plate fixation. If the pin does need to be removed, it can be done through a small incision with minimal dissection, often under local anesthetic. Chuang and colleagues reported success in 30 of 31 midshaft clavicle fractures treated with closed reduction and an intramedullary screw technique. Boehme and colleagues reported similar results in a series that included both fractures and nonunions. In addition, newer techniques describe insertion of smaller diameter elastic or flexible nails using a completely closed method. The fracture is reduced under image intensifier control and the pin is passed through a medial entry portal, across the fracture site, and impacted laterally. Disadvantages of this technique include difficulty in controlling shortening and rotation at the fracture site, especially if there is significant comminution. This may explain the inconsistent results seen with this technique when compared with nonoperative care (see later section).
Comparative studies
While there are many retrospective, single-arm studies that describe results after the treatment of various types of clavicle fractures, there are only relatively few prospective or randomized trials published. This section details high-quality comparative studies on a specific subgroup of injuries: completely displaced midshaft fractures of the clavicle in young (16–60 years of age) healthy patients.
Sling Versus Figure-of-Eight Bandage
There is evidence (2 randomized trials and multiple retrospective reviews) that a sling is as effective as a figure-of-eight bandage in immobilizing fractures of the clavicle and is favored by patients. There is no conclusively proven difference in radiographic or functional outcome regardless of the method of nonoperative treatment chosen. Lenza and colleagues, in a Cochrane Database Review of 234 nonoperatively treated patients from 3 randomized controlled trials, concluded that there was no evidence to support one nonoperative technique over another. For this reason the authors’ current treatment of choice for displaced midshaft fractures of the clavicle is a simple sling for comfort, followed by early range of motion exercise as pain diminishes.
Plate Fixation Versus Nonoperative Care
A multicenter, prospective, randomized clinical trial on this topic was performed by the COTS. One hundred thirty-two patients with completely displaced fractures of the midshaft clavicle were randomized to nonoperative (sling) or operative (open reduction and plate fixation) treatment. Although, as with most young male trauma populations, a significant number of patients were lost to follow-up, 111 patients were analyzed at a year after injury. Analysis of both surgeon- and patient-based outcome scores revealed significantly improved Constant and disabilities of the arm, shoulder and hand (DASH) scores in the operative group ( Figs. 1 and 2 ) with fewer nonunions (2/62 vs 7/49, P = .042) and symptomatic malunions (0/62 vs 9/49, P = .001). Complications in the operative group included hardware removal in 5 cases and local infections in 3 cases. These were treated with a single repeat operative procedure. In a similar study, which has been presented but not published, Smith and colleagues performed a prospective randomized trial comparing primary plate fixation with nonoperative care (sling) in 102 patients. This study was also complicated by a high rate of patients lost to follow-up, but the investigators found that open reduction and plate fixation resulted in union of all the 30 cases studied, whereas the nonoperative group had 12 nonunions in 35 cases ( P = .001). They concluded that plate fixation was safe, effective, and superior to nonoperative care with regard to preventing nonunion and improving patient function. They reported a 30% rate of hardware removal. It is important to note that both these studies were performed before the availability of anatomic precontoured plates.
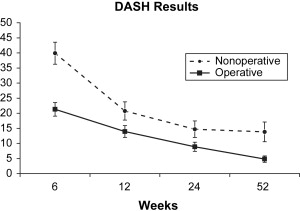
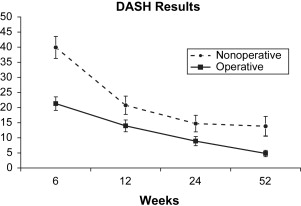
Based on these studies there is evidence that primary plate fixation of completely displaced midshaft fractures of the clavicle improves patient outcome and reduces the rate of nonunion and symptomatic malunion when compared with nonoperative care. This information is used when making a decision with the patient as to the optimal treatment method for their fracture.
Intramedullary Pin Fixation Versus Nonoperative Treatment
A randomized prospective trial performed in a US military population compared nonoperative care with intramedullary fixation (modified Hagie pin) of displaced clavicle fractures. There was no statistically or clinically significant difference in shoulder outcome scores at 1 year (operative 93 vs nonoperative 98). Also, complications were significantly higher in the operative group, including nonunion, refracture, infection, and pin prominence. However, the high rate of loss of reduction in the operative group (47%, leading to pin prominence as the fracture site shortened) indicates that fixation was suboptimal. An earlier retrospective study compared nonoperative (figure-of-eight bandage) with operative (intramedullary pin fixation) treatment in an Asian civilian population. The investigators reported no significant differences in shoulder scores (nonoperative 85 vs operative 83) at final review. The operative group had several complications including 8 infections, 3 refractures, 2 hardware failures, and 2 nonunions (14 of 40 patients, 35%). This technique using an open reduction with a large diameter pin does not appear to be as consistently successful as plate fixation. This may be due to several as-yet unclear factors including patient selection (size, compliance), fracture patterns (comminution), or surgery (technique, implant type).
In a randomized trial of 60 patients with completely displaced midshaft clavicle fractures, Smekal and colleagues compared a different type of intramedullary device, a smaller diameter elastic nail, with the nonoperative (sling) treatment. The investigators described a technique in which the fracture was reduced and the nail was inserted under radiographic control in a closed fashion in most cases. They reported superior outcomes in the operative group with better DASH and Constant scores at multiple time points up to and including 24 months after injury. There were 3 nonunions and 2 symptomatic malunions requiring correction in the nonoperatively treated group compared with no such complication in the group treated with a pin. However, there was pin protrusion in 7 patients and 2 required revision surgery. The authors concluded that their operative technique resulted in a decreased delayed and nonunion rate, resulted in a faster return to function, and provided better long-term functional outcome compared with nonoperative treatment.
Although intramedullary pin fixation remains promising, at the present time the results in comparative studies are too inconsistent to make any definite conclusions about one treatment over another.
Plate Fixation Versus Intramedullary Nailing
Because no comparative prospective or randomized study has been published comparing the outcome of plating with intramedullary nailing of displaced clavicular fractures, no specific recommendation can be made. Indirect inference can be made from the fact that 2 separate randomized trials show advantages of plate fixation over nonoperative care, whereas similar studies with intramedullary nailing as the operative technique are inconsistent. The theoretical advantages of intramedullary nailing (decreased soft tissue dissection, reduced hardware prominence, reduced refracture rate) may not outweigh the difficulties in maintaining length and rotation of the fracture (drawbacks of any unlocked intramedullary device). The only information currently available is an unpublished retrospective review with small numbers (17 patients per group), which suggested superiority of intramedullary pinning over plate fixation or nonoperative care for displaced midshaft clavicle fractures.
Meta-analyses on Clavicle Fracture Treatment
A meta-analysis of available data from articles on midshaft clavicle fractures published between 1975 and 2005 has been published. This meta-analysis contains information regarding all treated clavicle fractures, but for the purpose of this article data regarding displaced fractures are specifically assessed. A nonunion rate of 15.1% was observed after nonoperative care of such injuries, whereas the nonunion rate for similar fractures treated with plate fixation was 2.2%. The nonunion rate for fractures treated with intramedullary pinning was 2%. Therefore, plating a displaced fracture of the clavicle resulted in a decrease in the nonunion rate from 15.1% to 2.2% when compared with nonoperative treatment; this represents a relative risk reduction of 86%, (95% CI = 71%–93%). A meta-analysis performed by the Cochrane Database Review examined 3 trials that compared a sling with a figure-of-eight bandage or low-intensity pulsed ultrasound versus placebo in the treatment of displaced midshaft fractures. There were methodological problems with each study, and no significant differences in functional or other outcome could be shown. The investigators concluded that, at the present time, there is no evidence to support the superiority of one nonoperative technique over another ( Tables 1–3 ).








