7
Classification of Articular Cartilage Injury and Repair
BERT R. MANDELBAUM, RALPH A. GAMBARDELLA, AND JASON M. SCOPP
The most important issue in the management of articular cartilage disorders is accurate and uniform characterization of the local, regional, systemic, and familial factors. Subjective and objective tools can be used to assess both the lesion and the disease process. These tools can also be used for therapeutic and prognostic indications.
The assessment tools and classification schemes must be accurate, reproducible, valid, cross-cultural, and unbiased by age, language, and demographic differences. In the contemporary milieu of digital databases and multimedia information sharing, uniformly accepted multidimensional tools of assessment is essential. This chapter presents the methods of subjective and objective assessment of articular cartilage disorders, including the spectrum of normal chondropenia and osteoarthritis, and identifies essential future directions.
 Subjective Methods of Assessment
Subjective Methods of Assessment
History
An accurate and thorough patient history is an essential first step in the evaluation of articular cartilage defects (ACDs). Important details include the patient’s age, age at which the injury occurred, the defect etiology, mechanism of injury, and prior surgical interventions. Medical and family history of inflammatory arthritides such as lupus, rheumatoid arthritis, and human leukocyte antigen (HLA)-B27 associations are important factors to consider in treatment planning. Endocrine disorders including thyroid and diabetes, and collagen disorders such as Ehlers-Danlos and Marfan syndromes are known chondral modifiers and are important details in the patient’s history.
Subjective Knee Scores
A subjective clinical survey outcome tool can be used to create a reliable, reproducible score. This score can then be used to stratify each patient along the continuum of articular cartilage disorders and provide insight into the specific and appropriate treatment profile. The continuum of articular cartilage disorders exists with normal cartilage on one end of the spectrum. As articular cartilage fails, chondropenia results. Chondropenia is defined as a loss of articular cartilage over time. Whereas osteopenia is a term used to describe the loss of bone form and function, chondropenia is an analogous term used to describe this process in articular cartilage. As cartilage loss continues, osteoarthritis results.
Various instruments have been used to stratify the subjective assessment ACDs and osteoarthritis. To date, there has been no effort to organize the subjective assessment tools to reflect the continuum that exists when describing articular cartilage disorders. As a consequence, patient population, age, and activity level are different. These differences are reflected in the scores. Therefore no consensus exists regarding an ideal scoring system.
The Cincinnati1,2 (Table 7–1), International Knee Documentation Committee (IKDC), and International Cartilage Repair Society (ICRS) (Fig. 7–1) rating scales are excellent subjective and objective knee scores. They allow the patient and the clinician to rate symptoms quantitatively in relation to severity and functional level in a spectrum from sedentary life to return to sport.
| Function |
|---|
| Overall Activity Level |
| 20—No limitation. I have a normal knee and I am able to do everything including strenuous sports or heavy labor. |
| 16—I can partake in sports including strenuous ones but at a lower performance level. I must guard my knee and limit it to some heavy labor. |
| 12—Light recreational activities are possible with RARE symptoms. More strenuous activities cause problems. Active in non-strenuous sports. |
| 8—No sports or strenuous activities possible. Walking activities possible with RARE symptoms. I am limited to light work. |
| 4—Walking activities and daily living cause moderate problems. I frequently limit my activity. |
| 0—Walking activities and daily living cause severe problems and persistent symptoms. |
| —I do not know what my real activity level is. I have not tested my knee. |
The IKDC Subjective Knee Form is a reliable and valid measure of symptoms, function, and sports activity experienced by individuals with a variety of knee conditions including ligament and meniscal injury, patellofemoral problems, and osteoarthritis. A recent revision includes new demographic, subjective, and quality-of-life modules. The Subjective module includes 18 questions categorized by symptoms, pain, swelling, locking, giving way, sports activity, and function. In addition the knee history and surgical documentation forms have been developed with the ICRS and document articular cartilage, meniscal, and ligamentous status. The updated knee examination form includes documentation of effusion, passive motion deficit, ligament examination, compartment findings, harvest site pathology, radiographic findings, and functional tests.
Additionally, a quality of life survey like the Rand Short Form (SF)-363 is helpful to optimally define the impact of the problem and interventions on the patient’s psychosocial and emotional lifestyle. Other accepted tools that have been utilized globally for assessment of articular cartilage lesions include the Hospital for Special Surgery Score, the Visual Analog Scale (VAS), the Lysholm, and the Tegener4 scores. The major collective disadvantage of these tools is their lack of uniform and universal acceptance.
Several subjective outcome measurements have been developed to assess knee osteoarthritis (OA) disease severity at both baseline and after intervention. It is important to note, however, that patient perspective and physician perspective may differ. Therefore, symptom assessment tools used during treatment for OA should include a combination of patient and physician assessment. The VAS combined with either of two self-administered, algofunctional questionnaires can help to eliminate this potential bias. In North America, the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC)5 has achieved widespread acceptance as the gold standard for the assessment of OA-related symptoms, whereas in Europe the Lequesne Algofunctional Knee Index6 has been preferred.
The WOMAC index is composed of pain, stiffness, and disability subscales.5 Each subscale, and a variety of subscale combinations, has been validated for use with surgical and pharmaceutical intervention. The WOMAC bears excellent reproducibility as well as intra-and interobserver reliability. A modification of the WOMAC index, termed the Knee Injury and Osteoarthritis Outcome Score (KOOS) (Table 7–2) has been proposed by Roos et al.7 for use in posttraumatic OA of the knee. The KOOS was developed as an instrument to assess patients’ opinions about their knee and associated problems. The KOOS is intended to be used for knee injury that can result in posttraumatic OA, such as anterior cruciate ligament (ACL) injury, meniscus injury, and chondral injury. KOOS has high test-retest reproducibility. KOOS is meant to be used over short and long time intervals, and to assess changes from week to week induced by treatment (medication, operation, physical therapy) or over years due to the primary injury or posttraumatic OA. KOOS consists of five subscales: pain, other symptoms, function in daily living (activities of daily living, ADL), function in sport and recreation (Sport/Rec), and knee-related quality of life (QOL). KOOS is patient-administered, the format is user friendly, and it takes ~10 minutes to fill out. The KOOS system is self-explanatory and can be administered in the waiting room or used as a mailed survey. KOOS includes WOMAC Osteoarthritis Index LK 3.0 in its complete and original format, and WOMAC scores can be calculated. WOMAC is valid for elderly subjects with knee OA. KOOS construct validity has been determined in comparison with SF-36, and the expected correlations were found. Moderate to high correlations were found when compared to the Lysholm knee scoring scale. The KOOS subscales Sport and Recreation Function and Quality of Life were more sensitive and discriminative than the WOMAC subscales Pain, Stiffness, and Function when studied in subjects meniscectomized 21 years ago and with definite radi-ographic signs of OA (mean age 57 years, range 38–76) compared with age-and gender-matched controls.
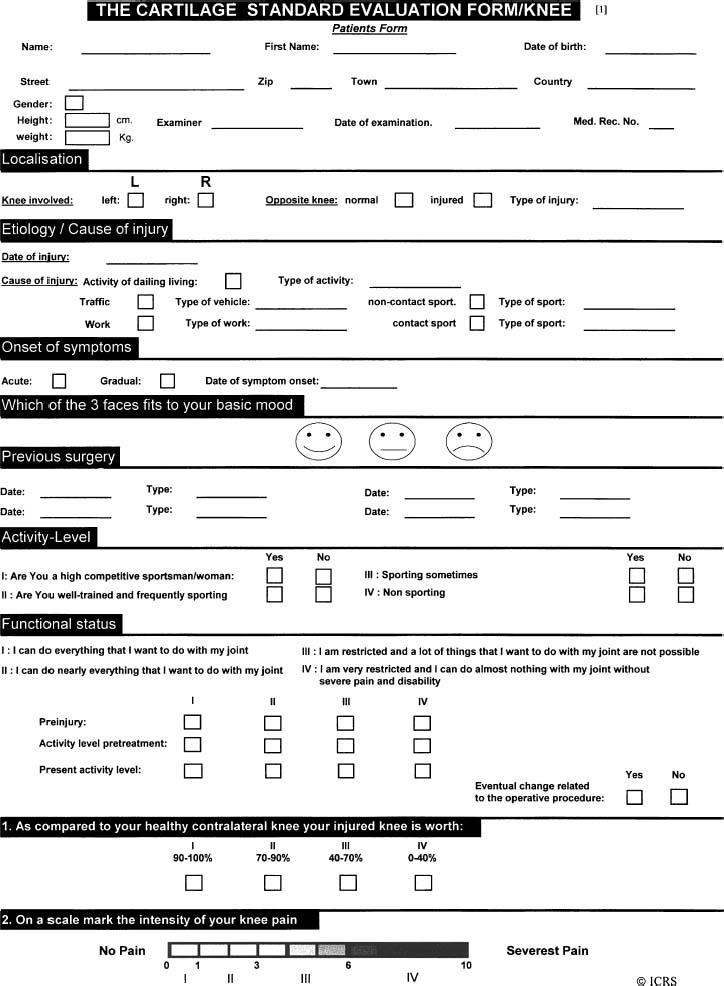
FIGURE 7–1 International Cartilage Repair Society (ICRS) Patient’s Subjective Rating System.
| Pain |
|---|
| P1 How often is your knee painful?___Never___Monthly___Weekly___Daily___Always |
| What degree of pain have you experienced the last week when…? |
| P2 Twisting/pivoting on your knee___None___Mild___Moderate___Severe___Extreme |
| P3 Straightening knee fully___None___Mild___Moderate___Severe___Extreme |
| P4 Bending knee fully___None___Mild___Moderate___Severe___Extreme |
| P5 Walking on flat surface___None___Mild___Moderate___Severe___Extreme |
| P6 Going up or down stairs___None___Mild___Moderate___Severe___Extreme |
| P7 At night while in bed___None___Mild___Moderate___Severe___Extreme |
| P8 Sitting or lying___None___Mild___Moderate___Severe___Extreme |
| P9 Standing upright___None___Mild___Moderate___Severe___Extreme |
| Symptoms |
| Sy1 How severe is your knee stiffness after first wakening in the morning? |
| ___None___Mild___Moderate___Severe___Extreme |
| Sy2 How severe is your knee stiffness after sitting, lying, or resting later in the day? |
| ___None___Mild___Moderate___Severe___Extreme |
| Sy3 Do you have swelling in your knee?___Never___Rarely___Sometimes___Often___Always |
| Sy4 Do you feel grinding, hear clicking or any other type of noise when your knee moves? |
| ___Never___Rarely___Sometimes___Often___Always |
| Sy5 Does your knee catch or hang up when moving? |
| ___Never___Rarely___Sometimes___Often___Always |
| Sy6 Can you straighten your knee fully?___Always___Often___Sometimes___Rarely___Never |
| Sy7 Can you bend your knee fully?___Always___Often___Sometimes___Rarely___Never |
| Activities of daily living |
| What difficulty have you experienced the last week…? |
| A1 Descending stairs___None___Mild___Moderate___Severe___Extreme |
| A2 Ascending stairs___None___Mild___Moderate___Severe___Extreme |
| A3 Rising from sitting___None___Mild___Moderate___Severe___Extreme |
| A4 Standing___None___Mild___Moderate___Severe___Extreme |
| A5 Bending to floor/pick up an object___None___Mild___Moderate___Severe___Extreme |
| A6 Walking on flat surface___None___Mild___Moderate___Severe___Extreme |
| A7 Getting in/out of car___None___Mild___Moderate___Severe___Extreme |
| A8 Going shopping___None___Mild___Moderate___Severe___Extreme |
| A9 Putting on socks/stockings___None___Mild___Moderate___Severe___Extreme |
| A10 Rising from bed___None___Mild___Moderate___Severe___Extreme |
| A11 Taking off socks/stockings___None___Mild___Moderate___Severe___Extreme |
| A12 Lying in bed (turning over, maintaining knee position)___None___Mild___Moderate___Severe___Extreme |
| A13 Getting in/out of bath___None___Mild___Moderate___Severe___Extreme |
| A14 Sitting None___Mild___Moderate___Severe___Extreme |
| A15 Getting on/off toilet___None___Mild___Moderate___Severe___Extreme |
| A16 Heavy domestic duties (shoveling, scrubbing floors, etc.___None___Mild___Moderate___Severe Extreme |
| A17 Light domestic duties (cooking, dusting, etc.)___None___Mild___Moderate___Severe___Extreme |
| Sport and recreation function |
| What difficulty have you experienced the last week…? |
| Sp1 Squatting___None___Mild___Moderate___Severe___Extreme |
| Sp2 Running___None___Mild___Moderate___Severe___Extreme |
| Sp3 Jumping___None___Mild___Moderate___Severe___Extreme |
| Sp4 Turning/twisting on your injured knee___None___Mild___Moderate___Severe___Extreme |
| Sp5 Kneeling___None___Mild___Moderate___Severe___Extreme |
| Knee-related quality of life |
| What difficulty have you experienced the last week…? |
| Q1 How often are you aware of your knee problems?___Never___Monthly___Weekly___Daily___Alway |
| Q2 Have you modified your lifestyle to avoid potentially damaging activities to your knee?___Not at all___Mildly___Moderately____Severely___Totally |
| Q3 How troubled are you with lack of confidence in your knee?____Not at all____Mildly____Moderately____Severely_____Totally |
| Q4 In general, how much difficulty do you have with your knee?____None____Mild____Moderate____Severe____Extreme |
| Scoring: |
| Each item is scored 0 to 4 and the raw score for each section is the sum of item scores. |
| Scores are then transformed to a 0 to 100 scale. A higher score indicates fewer problems. |
| Scale Raw score Transformed score MDC90 |
| Pain/ 36 12points |
| Symptoms/ 28 8points |
| ADL/ 68 10points |
| Sport/Rec/ 20 19points |
| QOL/ 16 |
| range score raw Possible |
| 100 × score raw Actual Example: a pain raw score of 16 would be transformed as follows: |
| – 100 |
| 56 |
| 36 |
| 100) × (16 13 points |
| – 100 |
The KOOS’s responsiveness has been determined in two separate studies. Significant improvement was found after reconstruction of the ACL, after physical therapy, and 3 months after arthroscopic partial meniscectomy. High effect sizes (mean score change/preoperative standard deviation, SD) were found, indicating fewer subjects needed to yield statistically significant differences. The subscales Sport and Recreation Function and Quality of Life were the most responsive, with effect sizes ranging from 1.16 to 1.65.
The addition of two subscales was found in an initial analysis of the KOOS to add significantly to the data generated by the WOMAC index when applied to patients who had undergone prior meniscectomy.8 The two additional subscales are Sports and Recreation Function and Knee-Related Quality of Life. The clinometric properties of the KOOS have been found to be favorable in preliminary investigations.7 Further, the KOOS reflects response to physical therapy and surgery, including ACL reconstruction. The use of this expanded form of the WOMAC instrument was specifically designed to measure several subsets of knee function and quality of life in response to meniscal injury. The KOOS provides excellent subjective information regarding the baseline and postintervention status of patients undergoing meniscal transplantation. Work on the validation KOOS is ongoing. The KOOS is currently being used in several clinical studies involving patients with meniscus injury, ACL injury, cartilage injury, or posttraumatic osteoarthritis. The KOOS is currently available in three languages: American English, Swedish, and Danish.
The Lequesne Index6 also generates a score based on pain and functional limitations in response to various daily situations. To date, there have been few direct comparisons of the WOMAC and Lequesne instruments. Theiler et al9 compared the WOMAC and Lequesne-Algofunctional Index in patients with osteoarthritis. This study suggests similar sensitivity to change in pain and quality of life after treatment. The WOMAC tends to display better performance in the pain subscale than the self-administered version of the Lequesne symptom sections.10 Generally the data obtained from the two instruments is thought to be complementary, and the use of both scales may be advantageous.
Quality of life in osteoarthritis has been evaluated using the medical outcomes SF-36,3 a well-documented health-related quality-of-life (HRQOL) instrument consisting of 36 questions compressed into eight scales and two primary dimensions: the physical and mental component scores. This questionnaire provides an assessment of HRQOL that is not specific to osteoarthritis, but it provides data complementary to the WOMAC instrument when applied to patients with osteoarthritis.11
 Objective Methods of Assessment
Objective Methods of Assessment
Objective assessment of articular cartilage by both nonoperative and operative methods provides unbiased data regarding lesion size, depth, and location. Nonoperative tools include physical examination and imaging. Although this nonoperative assessment may provide vital information, the gold standard for lesion evaluation includes arthroscopy. Arthroscopic grading tools are presented in this section.
Physical Examination and Functional Assessment
Physical examination of the knee provides a functional assessment of articular cartilage status. Important elements include range of motion, effusion, and joint line tenderness. Additionally, varus or valgus malalignment and ligamentous integrity provide insight on the knee macroenvironment and possible forces transferred through an articular cartilage defect. The KT-1000 or -2000 Knee Ligament Arthrometer (Medmetric Corporation, San Diego, CA) allows measurements and side-to-side comparisons of anterior and posterior translation of the tibia on the femur. Isokinetic strength measurements are helpful to assess extremity and joint strength. Functional assessments such as the shuttle and the single leg hop define activity levels. Each of these physical examination tools is used to gather insight into the articular cartilage integrity and the lesion’s effect on knee function.
Imaging Techniques
Radiography
Popular diagnostic techniques for the measurement of the structural integrity of cartilage of the knee include plain radiography and magnetic resonance imaging (MRI). Because cartilage is not visible on plain radiography, the joint space width seen on weight-bearing x-rays has been employed as a proxy for cartilage integrity. In addition, calculation of mechanical axis and patellofemoral alignment is essential in the pre-and postoperative assessment of alignment.
Plain radiographic systems have distinct advantages in cost and availability over MRI and arthroscopy. But standard radiographs are limited by magnification errors,12 poor reproducibility,13 and limited interobserver reliability.14 The accuracy, reliability, and sensitivity to change of plain radiographs in patients with articular cartilage disorders of the knee can be optimized by correcting magnification errors, adhering to published protocols for radiographic technique, and using microfocal magnification and computerized interpretation of digitized radiographs.15 Despite these protocols and techniques, radiographs remain unable to detect subtle changes in cartilage morphology associated with articular cartilage defects, chondropenia, and early OA.16 In spite of these limitations, standardized enhanced plain radiographs remain the primary outcome measurements of choice for all studies of cartilage disorders of the knee. Standard radiologic projections include weight bearing anteroposterior (AP) projections, flexed 45-degree posteroanterior (PA), patella—femoral views, and lateral views. The most widely accepted quantitative radiographic assessment tool of articular cartilage disorders are the Kellgren-Lawrence and the Ahlbachk scoring systems.17 These tools quantify the degree of mild, moderate, or severe joint space narrowing, subchondral sclerosis, osteophytes, and cysts.
Magnetic Resonance Imaging
Interest has centered on the ability of MRI to image articular cartilage. In the first report on the ability of MRI to assess articular cartilage, Yulish and colleagues18 claimed that MRI could reliably diagnose early and late stages of osteoarthitis in the patella. These have been characterized by highly variable and generally not reproducible results. Nearly 13 years after the initial description of the use of MRI to assess articular cartilage, there remains a lack of consensus among investigators on what constitutes the normal MRI appearance of articular cartilage. Investigators have applied a wide variety of MRI pulse sequences toward the depiction of articular cartilage and have reached as many varied conclusions regarding its appearance as there have been published articles.6,7 On high-resolution MRI, articular cartilage demonstrates a multilaminar appearance. However, there is lack of consensus on both the different numbers of layers in normal articular cartilage and on the histologic correlate of what these apparently different layers represent. Several investigators have suggested that the multilaminar appearance can be attributed to technical (truncation) and artifactual (“magic” angle) factors.8,9
Magnetic resonance imaging has improved dramatically in recent years and now has the potential to replace plain radiographs in assessing articular cartilage structural outcome.13 The use of contrast enhancement through either direct or indirect injection increases the ability of MRI to detect articular cartilage lesions. A preliminary study demonstrated good correlation between an MRI-based quantification of cartilage damage and arthroscopic findings.19 Other investigators have explored the statistical attributes of MRI-based measurements of cartilage thickness and volume20 and the assessment of chondropenia and OA progression. Interobserver agreement, reproducibility, and accuracy remain significant problems for MRI-based evaluation of the severity of knee articular cartilage.21 Moreover, optimal imaging protocols are evolving.3 In the past, spinecho (SE) sequences have shown poor sensitivity for detection of articular cartilage defects. Most recently the fat-suppressed T1-weighted 3D gradient echo, fast spin echo, or magnetic resonance (MR) arthrographic techniques with gadolinium have enhanced the sensitivity to over 85% in grade III and IV lesions. In addition, MR has been helpful as an adjunct in the assessment of articular cartilage repair in observing defect fill, continuity of surface, status of medullary bone, and definition of histology of repair tissues. Thus, the MRI as a diagnostic and outcome measurement tool for studies of articular cartilage disorders continues to evolve.
Arthroscopy
Arthroscopy provides direct visualization of articular cartilage and the knee macroenvironment. Articular cartilage defects can then be documented on operative reports, videos, photographs, and diagrams (grids and maps). These data can then be combined with subjective and objective findings obtained during history and physical examination. As a consequence, via arthroscopic lesion visualization, the clinician can define and classify the local, regional, and systemic factors that may influence lesion progression, joint degeneration, or defect regeneration. The following factors should be considered when visualizing articular cartilage defects:
1. Etiology: Is the defect acute or chronic? Was there a specific mechanism of injury or is the defect a consequence of chronic repetitive injury? This differentiation is often a difficult element to determine because there is typically a blend of acute and chronic etiologies.
2. Defect thickness: What is the thickness or depth of the defect? The most accepted method of depth classification is the Outerbridge Classification22). Recently, Brittberg and Winalski23 modified the Outerbridge Classification (Fig. 7–2). Normal articular cartilage is grade 0, softening is grade I, fibrillation is grade II, fissuring is grade III, and full-thickness defect, with exposed subchondral bone, is grade IV. Grade I and II lesions are considered partial lesions, whereas grade III and IV lesions are full thickness. Tidemark penetration, avascular necrosis, bone bruises, or infarctions are also important factors to consider in the assessment of these defects.
3. Size: A probe can be used to accurately measure defect size. Defects less than 2 cm2 are considered small, lesions between 2 cm2 and 10 cm2 are considered moderate, and lesions greater than 10 cm2 are large.
4. Degree of containment: Lesion containment refers to the presence of an adequate margin of surrounding healthy articular cartilage. This margin can often be visualized on sagittal MRI images.
5. Location: What is the defect’s location? Is it monopolar; bipolar, that is, a “kissing lesion” (medial femoral condyle and medial tibial plateau, for example); or multipolar? Each of these examples has different reparative and degenerative variables (Fig. 7–2).
6. Ligament integrity: Are the ACL and posterior cruciate ligament (PCL) intact? If there is ligamentous disruption, is there a combined rotatory instability? If there has been ligamentous reconstruction, has joint stability been re-created?
7. Meniscus integrity: Are the menisci intact? If not, has partial, subtotal, or complete meniscectomy been performed? Has meniscal repair or allograft meniscal replacement been considered?
8. Previous management: Has there been prior debridement and chondroplasty, drilling, microfracture, bone graft, allograft, autologous chondrocyte implantation, or mosaicplasty?
9. Status of repair (Fig. 7–3): If there has been previous management, repair tissue can be evaluated both biomechanically and histologically. An articular cartilage resilience and stiffness probe has been developed24 to test arthroscopically the mechanical repair characteristics. Additionally, the ICRS visual histologic score25 can be used to assess hyaline versus fibrocartilage repair.
10. Biochemical synovial markers: Synovial biopsy can be done during arthroscopy for evaluation of synovial disorders as well as joint microenvironment modifiers including stromelysin (matrix metalloproteinases MMP-1 and MMP-3) and other cytokines.




