Classification of Acetabular Defects in Revison Total Hip Arthroplasty and an Overview of Surgical Techniques
Ryan Caufield
Scott M. Sporer
Wayne G. Paprosky
Introduction
The aging of the population and the expansion of the number of younger patients with degenerative conditions of the hip have led to an increase in the number of primary total hip arthroplasty (THA) procedures. The burden of revision surgery is expected to increase in the coming years due to the greater prevalence of patients living with a hip arthroplasty along with overall greater life expectancy. The indications for acetabular revision include symptomatic aseptic loosening, instability, periprosthetic infection, periprosthetic osteolysis, and bearing surface wear. Revision surgery may also be indicated in an asymptomatic patient with progressive osteolysis, severe wear, or bone loss that could compromise a future reconstruction. One of the more challenging aspects of acetabular revision is the identification and management of the bone loss encountered intraoperatively. Substantial bone loss can complicate implant fixation and stability and thus result in a recurrent failure of the reconstruction.
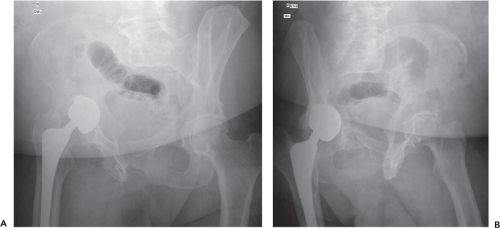
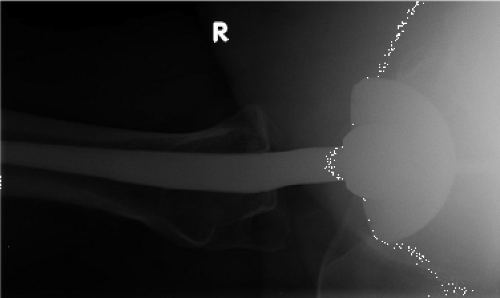
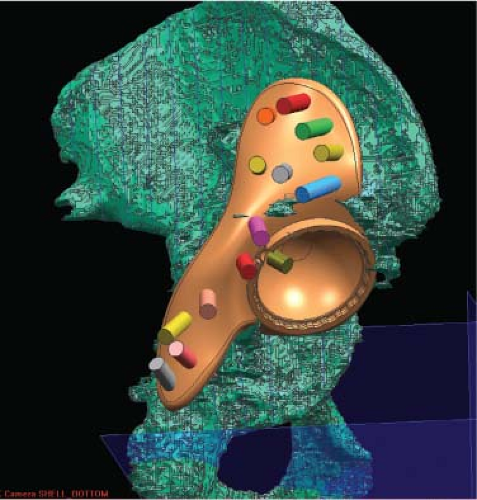
Appropriate preoperative planning is essential in preparing for revision procedures. One aspect of preoperative planning is a complete radiographic assessment. Plain radiographs (including an AP pelvis and AP/lateral of that hip to include the entirety of the prosthesis) are assessed for component position, signs of component loosening, polyethylene wear, and the location and degree of osteolysis and associated bone loss. Judet views may also assist surgeons in evaluation of the anterior and more importantly the posterior column (Fig. 108.1A,B), while a shoot through lateral (Fig. 108.2) can provide important information regarding acetabular component anteversion and the integrity of the posterior column. While not crucial to obtain in every case, advanced imaging techniques such as computed tomography (CT) scans can assist the surgeon in evaluating the severity of bone loss, particularly if three-dimensional (3D) reconstructions are available. A CT scan can provide a more accurate estimate of volumetric bone loss secondary to osteolysis (Fig. 108.3) and can also provide a more accurate evaluation of the acetabular component orientation, particularly in cases of recurrent instability (Fig. 108.4). In addition, CT scans can be helpful while evaluating insufficiency fractures, provide cross sectional images to construct custom implants as well as provide the ability to generate a 3D model to assist preoperative planning (Fig. 108.5).
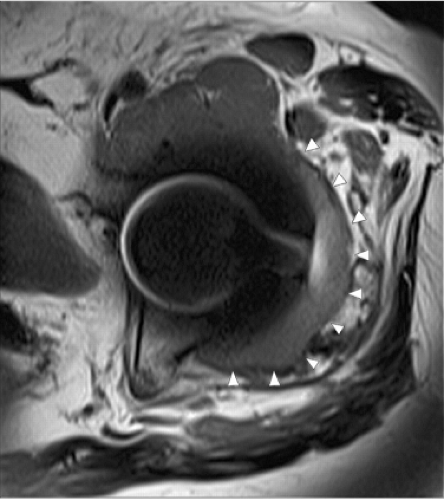
The routine use of magnetic resonance imaging (MRI) to date has had a limited role in preoperative planning for revision surgery. Metallic artifact reduction software (MARS) protocols may be beneficial to visualize and quantify a soft tissue mass or fluid collection associated with failed metal-on-metal THA or corrosion reactions (Fig. 108.6).
Acetabular reconstruction options will ultimately be dependent upon the location and amount of remaining host bone, local biologic potential, and the ability to achieve stable fixation. A useful classification system should accurately predict the severity and location of bone loss, guide treatment options, and permit surgeons to compare outcomes among patients. Furthermore, a classification system should remain simple enough to ensure a high degree of intra- and interobserver reliability, yet be detailed enough to alert surgeons when alternative reconstruction methods or special equipment is required including the need for allograft bone, structural augments, or cages.
Aaos Acetabular Defect Classification
The American Academy of Orthopaedic Surgeon classification of bone defects, described by D’Antonio et al., identifies the pattern and location of bone loss (1,2). This is a
descriptive classification system which categorizes acetabular defects as segmental (type I), cavitary (type II), combined contained/segmental (type III), pelvic discontinuity (type IV), or ankylosis (type V). Type I defects represent a complete loss of bone in the supporting portion of the acetabulum. The specific location can be in either at the periphery (superior, anterior, posterior) or central (medial wall). Type II defects represent volumetric bone loss within the acetabulum. The location can again be either in the periphery (superior, anterior, posterior) or central (medial wall). One unique attribute of this classification system is that a deficient acetabulum may actually contain several defect types. In addition, this classification does not quantify the degree of bone loss. Benefits of this classification system include its ease of use. The AAOS classification system is based primarily upon intraoperative findings and does not attempt to classify defects based solely upon preoperative radiographs. Therefore this system is of marginal value during the preoperative planning of acetabular revisions.
descriptive classification system which categorizes acetabular defects as segmental (type I), cavitary (type II), combined contained/segmental (type III), pelvic discontinuity (type IV), or ankylosis (type V). Type I defects represent a complete loss of bone in the supporting portion of the acetabulum. The specific location can be in either at the periphery (superior, anterior, posterior) or central (medial wall). Type II defects represent volumetric bone loss within the acetabulum. The location can again be either in the periphery (superior, anterior, posterior) or central (medial wall). One unique attribute of this classification system is that a deficient acetabulum may actually contain several defect types. In addition, this classification does not quantify the degree of bone loss. Benefits of this classification system include its ease of use. The AAOS classification system is based primarily upon intraoperative findings and does not attempt to classify defects based solely upon preoperative radiographs. Therefore this system is of marginal value during the preoperative planning of acetabular revisions.
Gross Acetabular Defect Classification
The classification system described by Saleh et al., is based upon the degree of bone loss seen on preoperative standard AP and lateral radiographs of the hip and consists of five
distinct categories (3). A type I defect demonstrates minimal bone loss and does not require revision components. A type II defect consists of a contained loss of bone stock while a type III defect is uncontained with <50% host bone compromise. A defect is considered uncontained if morselized bone graft cannot be used to fill the defect. Type IV defects represent uncontained bone loss >50%. These defects have severe column deficiencies. The defect is classified as type V if a pelvic discontinuity is encountered regardless of the amount of remaining host bone. This classification system has been shown to demonstrate a high degree of inter- and intraobserver reliability as well as a high degree of validity based upon intraoperative findings. This classification system is helpful in preoperative planning but lacks the ability to describe the specific location of bone loss.
distinct categories (3). A type I defect demonstrates minimal bone loss and does not require revision components. A type II defect consists of a contained loss of bone stock while a type III defect is uncontained with <50% host bone compromise. A defect is considered uncontained if morselized bone graft cannot be used to fill the defect. Type IV defects represent uncontained bone loss >50%. These defects have severe column deficiencies. The defect is classified as type V if a pelvic discontinuity is encountered regardless of the amount of remaining host bone. This classification system has been shown to demonstrate a high degree of inter- and intraobserver reliability as well as a high degree of validity based upon intraoperative findings. This classification system is helpful in preoperative planning but lacks the ability to describe the specific location of bone loss.
 Figure 108.3. Coronal CT image showing severe osteolysis following a right total hip arthroplasty. (Image courtesy of Craig J. Della Valle, MD.) |
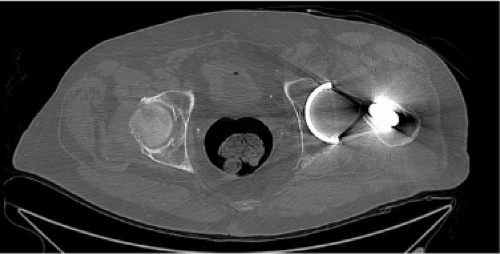 Figure 108.4. CT scan of the pelvis showing minimal anteversion of the implanted acetabular component. (Image courtesy of Craig J. Della Valle, MD.) |
Paprosky Classification for Acetabular Defects
The acetabular classification system of Paprosky is commonly used to assist in preoperative planning and is based upon the severity of bone loss and the ability to obtain stability of the revision component with a cementless acetabular component for a given pattern of bone loss (4).
Radiographic Correlation
A preoperative AP pelvis radiograph is used to predict the type of defect present and allows the surgeon to plan accordingly for the acetabular reconstruction. Four criteria on the preoperative AP pelvis radiograph are the basis of the Paprosky classification: (1




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree