CHAPTER 13 Chiropractic practice, experience, and research related to somatovisceral interactions
Introduction
The broadest definition of chiropractic is that it is a healthcare profession providing non-drug, non-surgical treatment of conditions related to the neuromusculoskeletal system. Its approach to care is concerned with the relationship of structure – chiefly the musculoskeletal system – to function, as mediated chiefly through the nervous system (Christensen et al. 2005). The chiropractic healthcare model has traditionally emphasized the body’s natural recuperative power through a patient-centered and holistic approach emphasizing the relationship between structure and function, with manual procedures playing a central role.
In fact, chiropractic is often viewed as being synonymous with spinal manipulative therapy (SMT). Certainly SMT has been the cornerstone of the chiropractic approach to care, and 94% of SMT in the US is performed by chiropractors. However, SMT is not used solely by Doctors of Chiropractic (DC): references to its use are found in many cultures, including ancient Greece, where it is recorded that Hippocrates practiced manipulation (Gatterman 2004). Historical references to ‘bone setting’ show this form of traditional medicine to be learned through observation of functional movement of the human body and passed on through an apprenticeship model (Meeker & Haldeman 2002). Osteopathy and chiropractic arose from this tradition in the late 1800s, along with incorporation of the concept of vitalism – life force – that was current in the late 19th century. The original rationale for chiropractic treatment was that areas of joint dysfunction called subluxations caused interference to the nervous system and imbalance of innate intelligence, or vital force, and that SMT corrected this imbalance, thus allowing the body’s natural recuperative ability to restore normal function and health (Masarsky & Todres-Masarsky 2001).
SMT continues to play a central role in modern chiropractic practice. However, chiropractic is a profession, not a procedure, and chiropractors provide not only SMT, but a number of other conservative therapies, including soft tissue treatment and counseling on physical activity, diet and lifestyle (Meeker & Haldeman 2002). In clinical practice it is impossible to separate the effects of SMT from the other aspects of the clinical encounter, including not only various procedures and counseling, but also difficult-to-measure constructs such as patient and doctor expectations, the therapeutic effect of touch, and psychological effects of positive affect and belief (Cherkin & MacCornack 1989, Coulehan 1985, Coulter 1990, Oths 1994).
Further complicating assessment of the clinical effects of chiropractic care is the broad array of procedures used by different chiropractors, or even by the same chiropractor within a given clinical encounter. US DCs use an average of six different SMT techniques, as well as additional manual soft tissue treatment (Christensen et al. 2005) (Table 13.1).
Table 13.1 Manual procedures most commonly used by US chiropractors*
| Procedure | Description | % of US DCs |
|---|---|---|
| Manual technique | ||
| Diversified manipulation | High velocity, low amplitude | 96 |
| Trigger point therapy (myofascial release) | Soft tissue technique for muscle tension; not SMT1 | 91 |
| Massage therapy | Soft tissue technique; not SMT | 85 |
| Mobilization | Low velocity, low amplitude | 76 |
| Activator method technique | Instrument-assisted adjusting protocol; small amount of biomechanical force delivered | 70 |
| Acupressure | Soft tissue technique for muscle tension; not SMT | 58 |
| Flexion–distraction manipulation | Low-velocity mobilization of spine with use of specialized table; no or minimal rotation and extension | 57 |
| Sacro-occipital technique | Use of padded wedges to lever spinal segments into position with no direct application of biomechanical forces, rotation, or extension | 50 |
| Cranial technique | Low force manual procedure | 38 |
| Logan basic technique | Very low-force ‘reflex’ technique to correct vertebral misalignment/fixation | 26 |
| Counseling | ||
| Corrective exercise | Instruction to patient | 98 |
| Physical activity | Instruction to patient | 98 |
| Rehabilitation exercise | Instruction to patient | 88 |
* Source: Christensen et al. 2005.
1 SMT, spinal manipulative therapy.
Furthermore, DCs use an average of 12 adjunctive procedures in addition to SMT. These include not only manual procedures such as massage (85%), trigger point therapy (91%) and acupressure (58%), but also nutritional counseling and supplement advice (89%), electrical stimulation (77%), ultrasound (66%), and homeopathy (46%). Most US DCs also report using active procedures such as therapeutic exercise (98%) or rehabilitation exercise (89%) (Christensen et al. 2005).
‘Spinal manipulation’ refers to the application of biomechanical force to a spinal joint for the purpose of correcting joint dysfunction. In the array of SMT techniques they use, most DCs include techniques with varying amounts and applications of force, as summarized in Table 13.1. A high-velocity, low-amplitude (HVLA) procedure is most commonly used, to the extent that it is often considered to be synonymous with SMT. The biomechanical forces in the spectrum of SMT, for the more commonly used techniques, range approximately from 70 to 890 N (Fuhr 2005, Pickar et al. 2007). SMT may be applied manually or by means of instruments, specially designed tables, or padded wedges.
Chiropractic theory holds that SMT en- hances function and promotes the body’s self-healing capacity (Hawk 2007). However, to date theoretical constructs have not arisen to address possible differential effects of different modes of application of the biomechanical forces involved in SMT. Such theories might best be developed empirically, through both observational and experimental research. In the past 10 years, basic science investigations have begun to examine such effects (Cramer et al. 2006, Khalsa et al. 2006). Better knowledge of which specific protocols for delivering biomechanical force are most effective would greatly advance patient care. This would be an excellent application of translational research, which ‘refers to the “bench-to-bedside” enterprise of harnessing knowledge from basic sciences to produce new treatment options for patients’ (Woolf 2008).
However, the ‘bench-to-bedside’ approach might be enhanced by the addition of the ‘bedside-to-bench’ direction (Marincola 2003). Manual therapies were not developed by bench research, but, as described above, grew from observation and experience. Lessons learned in the clinical application of manual therapies can inform the direction and focus of bench research, just as discoveries in the laboratory can inform and refine clinical applications.
Issues affecting interpretation of results
Manual therapies affect patients through diverse mechanisms
It is also important to consider that chiropractic care and/or SMT may have systemic or unexpected beneficial effects as well as the targeted local ones, in keeping with chiropractic theory as well as the limitations of current knowledge (Leboeuf-Yde et al. 2005). Therefore, it is helpful to include global measures of health and, where possible, detailed qualitative information on patient outcomes.
Summary of chiropractic clinical research
Musculoskeletal conditions
Approximately 8% of Americans use chiropractic annually, and well over 90% of their chief complaints involve musculo- skeletal pain, usually spine-related back pain, neck pain, and headache (Christensen et al. 2005). Whether as cause or effect of the prevalence of musculoskeletal complaints in chiropractic practice, the preponderance of chiropractic research relates to these. Most of this large body of research is related to SMT rather than chiropractic care in general. Many SMT studies involved osteopathic or manual medicine practitioners, and sometimes physical therapists, as well as chiropractors. SMT now has a substantial body of evidence for its effectiveness in relieving musculoskeletal complaints, especially spine-related pain (Bronfort et al. 2008, Hurwitz et al. 2008).
Non-musculoskeletal (somatovisceral) conditions
Prevalence in chiropractic practice
Chiropractors do not commonly treat patients for non-musculoskeletal – or as they are often called, somatovisceral – conditions. According to the Job Analysis of Chiropractic, the profession’s largest and most authoritative survey on practice characteristics, conducted by the National Board of Chiropractic Examiners, in 1998, 5.3% and in 2003 2.5% of chiropractic patients’ chief complaints were non-musculoskeletal. All somatovisceral conditions were reported to be treated ‘rarely’ except for the following, which were reported to be treated ‘sometimes’ (on a 5-point scale from ‘never’ to ‘routinely’): allergies, diabetes, hypertension, menstrual problems, sinus problems, and vertigo/dizziness (Christensen et al. 2005).
A 2001 practice-based research study of 7527 chiropractic patients actively recruited DCs who felt they saw higher-than-average numbers of patients with non-musculoskeletal complaints, in order to investigate factors associated with seeking chiropractic for such complaints (Hawk et al. 2001). Table 13.2 details these complaints; similar results in terms of the most commonly reported complaints were found in a 2005 international practice-based research study (Leboeuf-Yde et al. 2005). The 2001 study’s results indicated that factors associated with seeking chiropractic care for non-musculoskeletal complaints were: age under 14 years; female gender; small town or rural resident; multiple complaints; under concurrent medical care for their complaint; and first experiencing chiropractic care prior to 1960. Factors associated with chiropractic practices with a higher proportion of patients with non-musculoskeletal complaints were: use of more uncommon chiropractic techniques and use of additional non-manual procedures, particularly diet, nutrition and supplement counseling, herbs, naturopathy and homeopathy. They were also less likely to accept insurance.
Table 13.2 Non-musculoskeletal chief complaints reported by at least 20 (0.3%) chiropractic patients in a practice-based research study (n=7527) (Hawk et al. 2001)
| Musculoskeletal complaints | 78.3% |
| Health maintenance | 9.9% |
| Missing or unclassifiable | 1.6% |
| All non-musculoskeletal | 10.2% |
| Gastrointestinal | 1.1% |
| Upper respiratory complaint | 0.9% |
| Allergies | 0.7% |
| Migraines* | 0.6% |
| Sinus problems | 0.6% |
| Fatigue | 0.4% |
| Cardiovascular/circulatory (including hypertension) | 0.4% |
| Dizziness/vertigo | 0.3% |
| Ear infection | 0.3% |
| Asthma | 0.3% |
| All other non-musculoskeletal† | 4.6% |
| 100.0% |
* Migraines were considered non-musculoskeletal since they have vascular and other components. Other types of headaches were classified as musculoskeletal.
† Complaints listed by 15–19 patients (> 0.2%, < 0.3%): ADHD (attention deficit/hyperactivity disorder), lower respiratory infection/COPD (chronic obstructive pulmonary disease), urinary tract infection and sleep disorders.
Clinical research related to the effect of chiropractic care and/or SMT on somatovisceral conditions
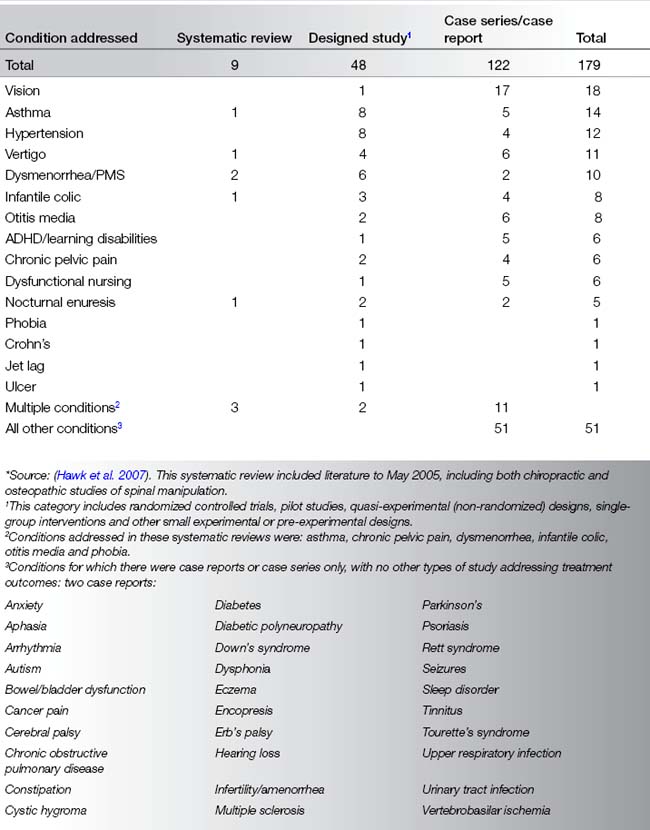
A 2007 systematic review of chiropractic care for non-musculoskeletal conditions, covering literature published up until mid-2005, identified 179 articles addressing treatment outcomes of either chiropractic care, which included manual procedures, or other types of care (such as osteopathy) which included spinal manipulation or mobilization (Hawk et al. 2007). The review included randomized controlled trials (RCTs), systematic reviews (SRs), cohort and case–control studies, other controlled studies including pilot and small randomized or nonrandomized studies, quasi-experimental, and pre-experimental case series and case reports.
Conditions addressed in clinical studies
According to the 2007 systematic review, the 179 articles identified addressed a plethora of conditions. Table 13.3 details the types of studies addressing each condition. Fifteen conditions were addressed by at least one designed study; for this purpose, ‘designed study’ refers to not only randomized controlled trials (RCTs) but also to cohort studies, quasi-experimental (non-randomized) studies, pre-experimental, pilot studies, and other small experimental or pre-experimental designs. Over 30 different conditions were addressed by case series or case reports only. In general, case reports far outweighed designed studies, with 122 case series/reports, 48 designed studies, and nine systematic reviews. This situation illustrates the difficulty of making inferences about causation.
Table 13.3 Articles addressing outcomes of chiropractic care and/or spinal manipulation for patients with non-musculoskeletal conditions, by condition and type of article*
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








