Childhood Obesity
William H. Dietz
Childhood obesity has now become the most prevalent nutritional disease of children and adolescents in the United States. Estimates from the 1999–2000 National Health and Nutrition Examination Survey (NHANES) indicate that approximately 15% of children in the United States are overweight. Furthermore, comparison of the prevalence of overweight in NHANES 1999–2000 with data from NHANES II completed in 1980 indicates that the prevalence of overweight doubled in 6to 11-year old children and tripled in 12to 17-year old adolescents. The prevalence of overweight, and its association with a variety of morbidities in childhood and adolescence, indicates that the prevention of overweight and the treatment of overweight among children and adolescents must become a high priority for pediatricians.
IDENTIFICATION
Childhood and adolescent overweight should be identified through the use of the body mass index (BMI) (weight in kg/height in m2). The BMI appears to be a reasonable index of adiposity, because it correlates reasonably well with the percentage of body weight attributable to fat among those with a BMI greater than or equal to the ninety-fifth percentile, it does not covary with height like the weight for height index, and an increased BMI predicts persistence and cardiovascular disease risk factors. The appropriate cutoff points for the identification of those at risk of being overweight and those who are overweight are the eighty-fifth and ninety-fifth percentiles, respectively, using the Centers for Disease Control and Prevention growth charts (http://www.cdc.gov/growthcharts and Chapter 5). The ninety-fifth percentile is the percentile identified by a BMI of greater than or equal to 30 in young adults, which corresponds to class I obesity in adults. Therefore, this approach makes the identification of childhood and adolescent obesity congruent with the criteria used to identify adult obesity.
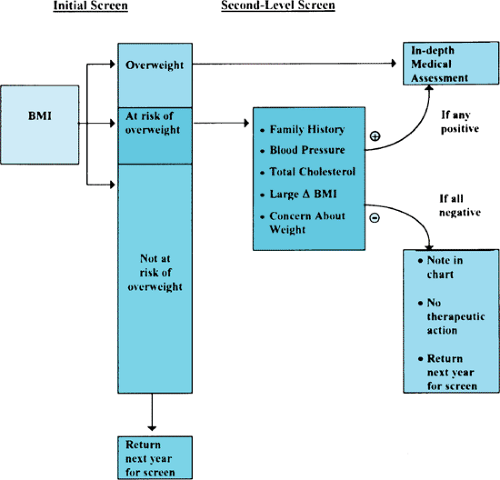
Because of the concern about spuriously labeling a child as overweight who may have an increased BMI because of an increase in muscle or bone mass, the approach indicated in Figure 376.1 should be followed in the assessment of a child with an increased BMI. One approach to distinguish children with an increased BMI attributable to fat from those whose BMI reflects an increase in fat-free mass or bone is the measurement of the triceps skinfold thickness (TSF). The TSF provides a relative but direct measure of body fat. If a child has an increased BMI, but normal TSF, the child is likely overweight, but not overfat. Both the child and the family should be reassured that the child’s increased BMI represents a growth variant, but that continued monitoring will be essential. If the child has an increased TSF, the additional screening tests noted in Figure 376.1 should be performed to assess whether an associated morbidity exists. Children whose BMI is at the eighty-fifth percentile or children who have had rapid weight gain of more than two BMI units annually should be considered at risk and followed carefully.
PERIODS OF RISK
Identification of the periods of risk for the development of childhood and adolescent obesity will help identify the times and populations that represent reasonable targets for counseling efforts. Young children at greatest risk for the development of adult obesity are children of two obese parents, regardless of the weight status of the child. Therefore, counseling with respect to diet and activity for children of two obese parents should begin early.
The first important period of risk for persistent obesity independent of the risk of parental obesity is the prenatal period. Children with birth weights greater than or equal to 4 kg have an increased risk of subsequent overweight. Maternal weight
gain during pregnancy is an important determinant of birth weight. The mechanisms that account for the effect of birth weight on subsequent growth include increases in cell number or alterations in brain growth or satiety centers.
gain during pregnancy is an important determinant of birth weight. The mechanisms that account for the effect of birth weight on subsequent growth include increases in cell number or alterations in brain growth or satiety centers.
A second potential period is the period of BMI rebound. After an initial increase in the BMI in the first year of life, the BMI begins to decline and reaches a nadir at 6 to 8 years of age. Thereafter, the BMI begins to increase again. Although it has been suggested that children in whom BMI rebound begins early are at increased risk for persistently increased BMI, this effect may be mediated by the BMI in early childhood rather than the time of BMI rebound. Inspection of the BMI growth charts indicates that children in the upper BMI percentiles have an earlier BMI rebound than do children in lower percentiles. The factors that affect fatness during this period remain uncertain. Factors in early childhood that affect food preference or alter regulation of food intake, or exposure of the child to environments that affect food or activity outside the home may alter energy balance to promote gains in body fat.
The third period of risk for the development of obesity or its complications is adolescence. Body fat increases in girls during adolescence, whereas body fat decreases in boys. In girls, however, body fat is deposited gluteally, whereas body fat in boys is deposited centrally. Visceral fat deposition increases the risk of a variety of cardiovascular morbidities such as hyperlipidemia, glucose intolerance, and hypertension. The risk of persistent obesity in adolescent girls is therefore greater than in boys, but the risk of subsequent mortality associated with obesity is greater in boys than in girls. Morbidity in adulthood associated with adolescent obesity is greater in both genders than in adults who were not obese during adolescence.
ASSOCIATED SYNDROMES AND COMPLICATIONS
The history and physical examination must exclude causes and associated complications of obesity. The quartet of signs that suggest an associated syndrome includes dysmorphic features, short stature, impaired vision, and hypogonadism or gonadal dysfunction. Their presence should initiate additional tests to exclude the more common syndromes listed in Box 376.1. At any age, obesity in children or adolescents is associated with an increased frequency of cardiovascular risk factors. Hypertension must be excluded by blood pressure determinations with an appropriately sized cuff. Elevated low-density lipoprotein cholesterol, decreased high-density lipoprotein cholesterol, and hypertriglyceridemia should be sought by a fasting lipoprotein profile. A fasting insulin determination helps exclude glucose intolerance. Although children or adolescents with acanthosis nigricans have been thought to be at particular risk for glucose intolerance, glucose intolerance and acanthosis nigricans appear more strongly related to the severity of obesity.
BOX 376.1 Syndromes Associated with Childhood Obesity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree