Chest and Abdominal Wall
Sami F. Rifat
Injuries to the chest and abdominal wall can occur in any sport but are more common in contact or collision sports such as hockey, football, and soccer. It is important that the treating physician differentiates benign chest and abdominal wall injuries from those that are potentially life threatening. This chapter focuses on injuries to the chest and abdominal walls although it is important to recognize that there is often an overlap between these conditions and injury to the viscera and extremities. Injuries to the deep structures and viscera are discussed elsewhere.
Chest
Blows to the chest are common in athletics. Blunt trauma can result in general injury to the chest wall or an injury to a specific structure, such as the sternum, sternoclavicular (SC) joint, clavicle, or ribs.
Chest Wall Contusion
Chest wall contusions usually result from blunt trauma. For all chest contusions, the physician should inspect the involved area to evaluate for gross deformity and abnormal, asymmetrical or paradoxical movement of the chest. Palpation for focal tenderness and crepitation should be performed. Auscultation of the heart and lungs for evidence of cardiac or pulmonary damage should be done. Severe blows to the chest can lead to comotio cordis, cardiac or pulmonary contusion, hemothorax, and pneumothorax. These entities are discussed elsewhere.
Treatment of minor, nonspecific chest wall contusions involves relative rest, ice, and consideration of an elastic bandage for support. Ace wraps should be used with caution because they may cause the athlete to take shallow breaths potentially leading to pulmonary atelectasis and pneumonia. Acetaminophen or a nonsteroidal anti-inflammatory agent may be used for analgesia. Large hematomas may require incision and drainage. Fortunately, most contusions heal after several days of conservative treatment. The athlete may return to competition when symptoms allow. Rib pads or a flak jacket may be required for protection in the short term.
Sternum Fractures
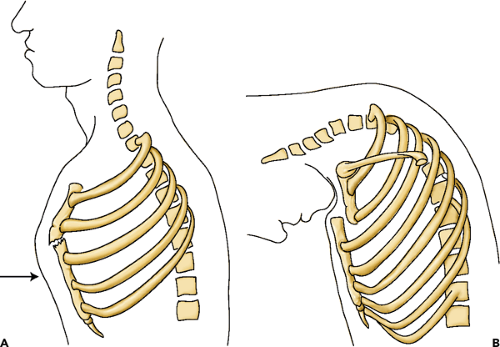
Sternal fractures are rare in sports. Although the fracture itself may not be that significant there is a high incidence of associated chest trauma such as cardiac and pulmonary contusions and injury to the internal mammary vessels. These injuries typically occur as a result of a direct high-impact blow, although a flexion-compression mechanism has also been reported (see Figure 28.1). Most commonly, a direct blow to the sternum causes a portion of the bone to displace inward resulting in fracture or sternomanubrial disruption. In the flexion-compression mechanism, flexion of the cervical spine drives the chin into the manubrium displacing it posteriorly.
Typically, the athlete presents with a history of trauma and localized pain over the sternum. A palpable defect is sometimes present. The pain is usually aggravated by deep inspiration. Plain radiographs, particularly a lateral chest film best demonstrate the fracture. Computed tomography (CT) is useful if the fracture is displaced and there is concern of damage to underlying structures.
Treatment of sternal fractures depends on whether displacement is present or not. Nondisplaced fractures
are treated symptomatically with rest, ice, and analgesics. The athlete may return to noncontact participation once sufficient healing has been accomplished. Return to contact sports generally can occur in 6 to 12 weeks. Displaced fractures often need to be reduced. They may be reduced in a closed or open manner depending on the degree of displacement. Referral is indicated and close monitoring of the patient’s cardiac and respiratory function is essential because of the high association with intrathoracic trauma.
are treated symptomatically with rest, ice, and analgesics. The athlete may return to noncontact participation once sufficient healing has been accomplished. Return to contact sports generally can occur in 6 to 12 weeks. Displaced fractures often need to be reduced. They may be reduced in a closed or open manner depending on the degree of displacement. Referral is indicated and close monitoring of the patient’s cardiac and respiratory function is essential because of the high association with intrathoracic trauma.
Sternoclavicular Joint
SC joint injuries may be either traumatic or atraumatic. Symptoms arising from an inherent (atraumatic) instability of the joint are relatively rare and therefore most SC injures encountered in athletes are traumatic in nature. Acute SC joint injuries include subluxation, fracture, and dislocation. The medial clavicular physis is vulnerable to fracture in skeletally immature individuals. Dislocation of the proximal clavicle relative to the sternum may be in either the anterior or posterior direction. Anterior dislocation is much more common. Posterior dislocation is a medical emergency and requires immediate attention due to the potential involvement of the great vessels, trachea, and esophagus.
The mechanism of SC joint injury may be either direct or indirect. Direct blow to the joint can occur from another player, surface, stick, puck or ball. Indirect SC injury may occur when a compression or traction force is applied across the joint. In the compression mechanism the athlete often falls onto his lateral shoulder and another player lands on top of him or her. This (indirect) blow causes the SC joint to buckle. Alternatively, the joint may be injured by a traction mechanism in which the athlete’s outstretched shoulder abducted to 90 degrees is forcibly extended.
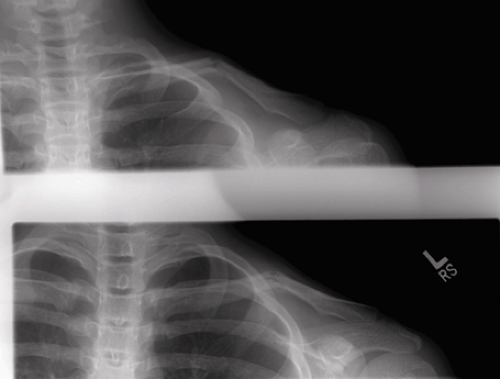
Athletes suffering a SC injury usually complain of severe pain, especially with movement of the arm. The pain is usually worse with the individual in the supine position. Physical examination reveals swelling, deformity, and local tenderness. The physician should carefully assess the patients respiratory and neurovascular status to rule out pressure on the underlying vital structures. Specifically, the physician should evaluate for pulselessness of the ipsilateral arm, extremity swelling, claudication, and dysthesias. Hoarseness, dyspnea, and dysphagia are signs of tracheal or esophageal involvement. Plain x-rays including the serendipity view (see Figure 28.2) (Anteroposterior [AP] radiograph of the SC joints with a 40 degree cephalic tilt) should be obtained. A CT scan is the test of choice if x-rays are inconclusive or posterior displacement is suspected.
Anterior subluxation, dislocation, and nondisplaced fractures of the proximal clavicle are usually treated conservatively and do not require reduction or surgery.
Generally a sling for comfort, ice, and analgesics are all that is required. Activity may be resumed as symptoms allow or once adequate bony healing takes place. Complete anterior dislocations usually require closed reduction. The patient is placed in the supine position and the shoulders are drawn backward while applying traction to the ipsilateral arm. A sandbag placed between the patient’s shoulder blades is often helpful. A figure-of-eight bandage should be used post reduction for 4 to 6 weeks. The patient should be advised that there may be a persistent deformity of the joint.
Generally a sling for comfort, ice, and analgesics are all that is required. Activity may be resumed as symptoms allow or once adequate bony healing takes place. Complete anterior dislocations usually require closed reduction. The patient is placed in the supine position and the shoulders are drawn backward while applying traction to the ipsilateral arm. A sandbag placed between the patient’s shoulder blades is often helpful. A figure-of-eight bandage should be used post reduction for 4 to 6 weeks. The patient should be advised that there may be a persistent deformity of the joint.
 Figure 28.2 Serendipity view, anteroposterior (AP) radiograph of the sternoclavicular (SC) joints with a 40 degree cephalic tilt. |
Posterior dislocations of the SC joint should be evaluated in the emergency department. These are potentially serious injuries and any attempt at treatment should be performed in a setting where surgeons are available to address possible complications, such as injury to the great vessels. Closed reduction is performed in the manner discussed in the preceding text.
Clavicle Fractures
Clavicle fractures are common in sports. They can result from direct or indirect trauma. Individuals participating in stick sports such as hockey or lacrosse may sustain direct bony injury. Clavicle fractures can also occur from indirect trauma as a result of a fall or blow to the lateral shoulder or upper arm. Clavicle fractures can occur anywhere along the length of the bone with the midshaft being the most common location.
The patient usually recalls a clear history of trauma and complains of pain at the fractured site. The arm on the affected side is usually held in a guarded position. A deformity is often obvious. Evaluation involves palpation to assess for pain, deformity, and crepitance. A careful neurological and vascular examination is essential. Auscultation of the chest is important to evaluate for pulmonary injury. Clavicle radiographs should be obtained (see Figure 28.3) although proximal clavicle fractures are sometimes difficult to visualize with plain radiography and CT is sometimes required.
Treatment of midshaft clavicle fractures is relatively straightforward. Most midshaft clavicle fractures respond well to supportive treatment consisting of a sling or figure-of-eight bandage, analgesic medications, and ice. Figure-of-eight harness does not offer an advantage and the simple sling is often more comfortable (1). There is debate over the indications for surgical management of clavicle shaft fractures. Table 28.1 lists some potential indications for surgery (2).
TABLE 28.1 Surgical Indications for Acute Clavicle Fracture | |
|---|---|
|
The treatment of proximal clavicle fractures is similar to SC joint injury and has been already discussed. Treatment of distal clavicle fractures is more controversial. Nondisplaced distal clavicle fractures can be treated conservatively similar to a shaft fracture. Displaced distal clavicle fractures may require surgical intervention and referral is indicated.
Rib Injuries
Rib fractures are one of the most common injuries to the chest wall (3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree