, Antonio Cesarani2 and Guido Brugnoni3
(1)
“Don Carlo Gnocchi” Foundation, Milano, Italy
(2)
UOC Audiologia Dip. Scienze Cliniche e Comunità, Università degli Studi di Milano, Milano, Italy
(3)
Istituto Auxologico Italiano, Milano, Italy
Abstract
Cervicogenic balance disorders (CBD) were first described as “cervical vertigo” by Ryan and Cope in 1955. Other terms used for the same disorder are proprioceptive vertigo, cervicogenic vertigo and cervical dizziness Cervicogenic balance disorders may be caused by a specific lesion mechanism like whiplash injury. More frequently, no apparent cause is revealed. Spontaneous neck pain may be present or not. A case history of cervicoartrosis or neck dysfunction, in general, may be present or not. The key impairment of CBD is head and neck motion intolerance not provoked by a whiplash mechanism nor a labyrinth lithiasis. The key lesion is the oversensitivity of spinal proprioceptors and a mismatch with vestibular cues. The treatment is a four-step programme as follows: (1) removing cervico-cephalic sensorimotor disturbances by means of manual medicine techniques including also vertebral manipulations performed by the physician, (2) amelioration of lifestyle through adequate counselling based on case history and accurate examination of the neck and the spine, (3) leading the patient to an awareness of own body and learning breath and neck tension control through physical exercises performed with a physiotherapist and (4) maintaining the results through home exercises.
Cervicogenic balance disorders (CBD) were first described as “cervical vertigo” by Ryan and Cope in 1955 [1]. Other terms used for the same disorder are proprioceptive vertigo, cervicogenic vertigo and cervical dizziness [2, 3].
Although the diagnosis has remained controversial since its introduction, several observations have led to the proposal of a plausible pathophysiologic mechanism:
The deep intervertebral muscles in the cervical spine possess a high density of muscle spindles and are assumed to play an important role in postural control [4–6].
Cervical afferents are known to be involved in the cervico-collic reflex, the cervico-ocular reflex and the tonic neck reflex, which work in conjunction with other reflexes influenced by the visual and vestibular systems to stabilize the head, the eyes and posture.
Vestibular and proprioceptive inputs are linearly combined for computing egocentric, body-centred coordinates [7–11].
Anaesthetic injections to the upper cervical dorsal nerve roots can produce dizziness and nystagmus [12, 13].
Brandt and Bronstein [3] proposed a mechanism where changed firing characteristics of cervical somatosensory receptors due to neck pain lead to a sensory mismatch between vestibular and cervical input, resulting in cervical vertigo. This mechanism seems to agree with the most recent findings about vestibular–somatosensory convergence in head movement control [16–18].
Cervicogenic balance disorders may be caused by a specific lesion mechanism like whiplash injury. More frequently, no apparent cause is revealed. Spontaneous neck pain may present or not. A case history of cervicoartrosis or neck dysfunction, in general, may be present or not.
In the case of a CBD due to whiplash, the patient has to be treated as explained in Chap. 12.
Generally, vertigo or dizziness due to a cervicogenic mechanism appears suddenly, after a more or less brisk movement of the head or of the body, usually in the sitting position, frequently after some time spent watching television or working at a PC. After the onset, symptoms may be caused by any kind of movement of the head/body, and even if cervical vertigo may be confused with benign paroxysmal positioning vertigo, the specific tests explained in the Chap. 8 lead to the correct diagnosis.
The key impairment of CBD is head and neck motion intolerance not provoked by a whiplash mechanism nor a labyrinth lithiasis. The key lesion is the oversensitivity of spinal proprioceptors and a mismatch with vestibular cues [19].
Accurate case history and proper clinical examination are usually the diagnostic key, but sometimes instrumental diagnosis is necessary to confirm and to help adequate therapeutic planning.
Instrumental diagnosis is aimed to evaluate cervical role on static postural control (static posturography), dynamic head-to-trunk stabilization (cranio-corpo-graphy) and cervico-oculomotor interaction (smooth pursuit neck torsion test, SPNTT) (see also Chap. 3). Cervical x-rays and neuroimaging (CT, MRI) are useless for this kind of diagnosis.
9.1 Static Posturography
The upright position is controlled by three distinct sensorial cues: visual, somatosensorial (from spine proprioceptors and pressure sensors in the feet) and vestibular (mainly from otolithic maculae). Posture is more stable when all the sensory systems operate and the head is aligned with the trunk. Routinely, posturography (PG) recording is performed under two basic conditions, patient standing on the platform with eyes open (EO) and with eyes closed (EC). Besides these basic tests to verify the presence of a latent postural disorder, cervical destabilizing tests are usually employed to identify a cervical origin of the dizzy symptoms. Through tests performed with rotation (“cervical dynamic activation” [20, 21], “head turned” [22] and retroflexion of the head [23]), it is possible to obtain some information about cervical destabilizing inputs. However, positive results obtained with the above-mentioned tests must be evaluated within the entire clinical context, because they cannot be considered as pathognomonic.
9.2 Cranio-corpo-graphy
Head destabilization seems to be the specific target to investigate equilibrium disturbances in whiplash patients and thus in CBD. Since 1968, cranio-corpo-graphy (CCG) has been used as a simple procedure to evaluate head-to-trunk stabilization in vestibular disorders [24] (Fig. 9.1).
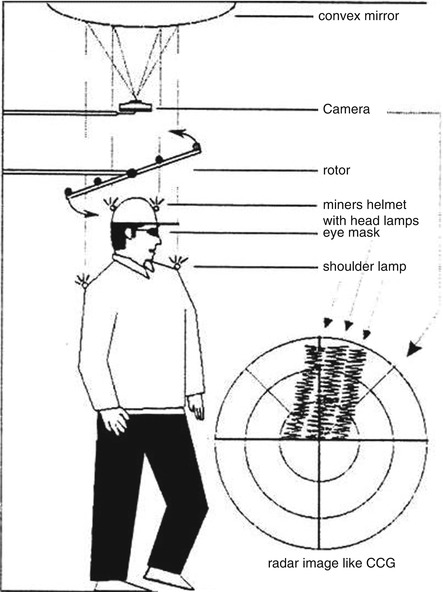
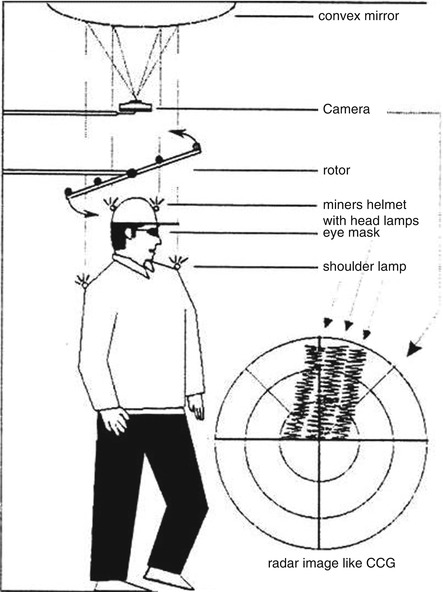
Fig. 9.1
A schematic representation of cranio-corpo-graphy. Subjects walk in place in a dark room, and movements of the light bulbs placed on the head (helmet) and shoulder impress the film in an instant Polaroid camera in order to obtain four light traces on a black imagine
It has proved to be one of the most efficient, quick, objective and quantitative tests for screening equilibrium function for nearly 20 years, and the West German Labour Security Surveillance Board introduced it for occupational medical ability testing in 1983. Cranio-corpo-graphy (CCG) has been successively digitalized (dCCG) on the basis of the optoelectronic technology [25]. Digital cranio-corpo-graphy (dCCG) was a non-invasive assessment based on a 50 Hz CCD camera for acquiring the position of four markers placed on the subject who walks in place (Fukuda stepping test) (Fig. 9.2).
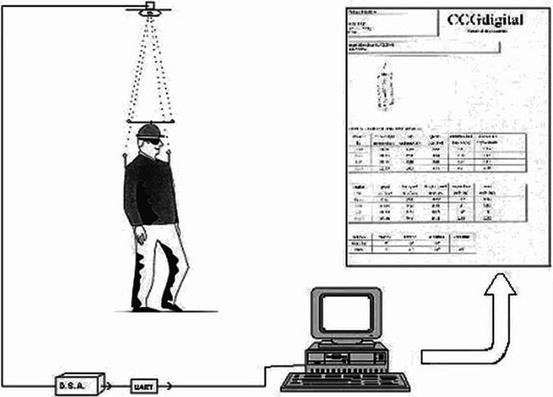
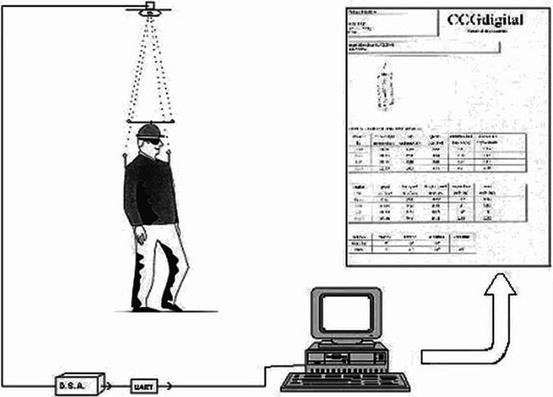
Fig. 9.2
Two passive reflective markers (front and rear) are set at the extremities of a stick attached to a worker’s hardhat, while two markers (left and right) are attached on rigid shoulder supports
Investigations performed with dCCG suggested that the most specific parameter able to discriminate between normal and pathological cervico-cephalic control is the ratio between head and trunk displacements. It is also possible to detect directly head and trunk sagittal (Y) and lateral (X) movements using a commercial equipment that uses two accelerometers that are 2D-sensitive (e.g. Delos, Turin, Italy) [26], respectively, fixed to the occiput and to the sternum in order to record sagittal and lateral displacements of the two body segments (Fig. 9.3).


Fig. 9.3
An accelerometer is fixed on the head and the other on the trunk in order to record sagittal and lateral displacements of the two body segments. Software calculates mean displacement velocities of the segments (°/s) and the ratio between head and trunk displacements
The equipment records 20″ body segment movements each test. Head-to-trunk stabilization (ratio between X and Y head and trunk displacements) during walking-in-place is thus calculated: a ratio <1 indicates stabilization of the head with respect to the trunk. Normal values range from 0.6 to 0.8. Values around 1 are considered borderline, while ratios >1 are pathological (Fig. 9.4).
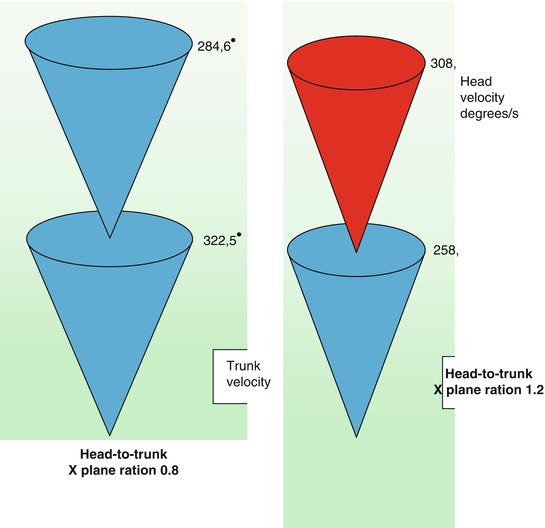
Fig. 9.4
Head and trunk sway are represented as superimposed cones. In normal, (left) cervico-cephalic control the head cone is smaller than the trunk cone, and head-to-trunk ratio is less than 1, while in a patient with pathological cervico-cephalic control (right), the pattern is reversed
9.3 Smooth Pursuit Neck Torsion Test (SPNT)
In 1998 Tjell and Rosenhall [27] firstly described a specific oculomotor test, named smooth pursuit neck torsion test (SPNTT), successively improved by Treleaven et al. [28].
The test is performed with the patient sitting on a chair free to rotate. SPNTT compares the gain of eye movements following a target (smooth pursuit) with the head in neutral position and with the body turned 45° right- and leftward (neck torsion). In this way the head counteracts the body rotation, but the eyes remain and labyrinths are not stimulated. To avoid “cervical bias,” it is necessary to slowly rotate the chair and to use a headrest to avoid neck fatigue and head sway. Any modification of smooth pursuit performance may only be due to cervical inputs, both proprioceptive and nociceptive.
Generally the test is performed using electrooculography (EOG) that measures and records eye movement while following a moving target. The target consists of a light spot projected into a TV screen through a visual angle of 30°. The smooth pursuit (SP) gain is calculated with the neck in a neutral position and also with the neck in a torsioned position. The difference between the gain in neutral and the average values in torsion equalled the smooth pursuit neck torsion difference ((SPNT–diff): gain[neutral] − (gain[left] + gain [right])/2).
The SPNT–diff thus equals 0 if the smooth pursuit eye movement performance did not differ between the neutral and the rotated positions.
Electrooculography may be used also to perform the Head Tracking Test (HTT) explained in Chap. 3. In this case the more efficient the cervico-ocular interaction, the lesser the movements of the eyes, that is to say, the lower the gain of smooth pursuit.
9.4 Treatment
The specific treatment is based on manual therapy interventions just like cervical pain and cervicogenic headache [29–31]. Physiotherapy and counselling consolidate the therapeutic result.
The treatment is a four-step programme as follows:
1.
2.
Amelioration of lifestyle through adequate counselling based on case history, accurate examination of the neck and the spine [34] and, eventually, some specific cervical function questionnaires like the Core Outcome Measurement Index for neck pain (COMI-neck), a short, multidimensional outcome instrument [35]
3.
Leading the patient to an awareness of her/his own body and learning breath and neck tension control through physical exercises performed with a physiotherapist
4.
Maintaining the results through home exercises
9.4.1 Manual Medicine
Manual medicine (MM) is a medical discipline based on the use of palpation and operator-directed techniques to aid in the diagnosis and treatment of musculoskeletal disorder. Manual medicine treatment includes the use of but is not limited to thrust/impulse (also the so-called high-velocity low-amplitude, HVLA) spinal manipulation, soft tissue mobilization (also the so-called low-velocity high-amplitude, LVHA), myofascial release and functional release. Manual medicine identifies a specific manipulable lesion, which is treated with an appropriate manipulative technique to resolve the condition [32]. The goal of manipulation is to restore maximal pain-free movement of the musculoskeletal system in postural balance.
Manual medicine is as old as medicine itself. It was practiced in Thailand 4,000 years ago and used in ancient Egypt. Hippocrates, the founder of modern medicine, used traction and leverage techniques to treat spinal disorders. In the nineteenth century “bone setters” were popular in Europe and the United States. Dr. Edward Harrison, in 1784; Andrew Taylor Still, in 1874; and D.D. Palmer, in1896, began what is known today as manual medicine, osteopathy and chiropractic, respectively. In the twentieth century James Mennell and Edgar Cyriax began the modern use of manual medicine in Europe. Manual medicine has found application in orthopaedic, neurologic, rheumatologic, physical medicine and rehabilitation.
Standardization of the appropriate diagnostic course to identify specific manipulable lesion is mainly due to Robert Meigne’s researches [33]. This author defined the so-called painful minor intervertebral dysfunction (PMID) as the basis of the treatment diagnosis of a spinal musculoskeletal disorder [34].
The identification of PMIDs at different spine levels allows a specific conservative and manual treatment of the biomechanic dysfunctions that lead to cervicogenic balance disorders (CBD).
On the basis of clinical and instrumental evaluation of the patient affected with CBD, appropriate combination of different manual techniques may be planned.
Generally speaking, a proper treatment may be stepped as follows:
1.
Soft tissue treatment, that is to say, delicate massage of superficial and deeper layers of the muscle and connective tissue of the shoulders and the neck in order to enhance function, decrease muscle reflex activity and inhibit motor-neuron excitability.
It includes manoeuvres directed toward the muscles and fascia throughout the body. It involves a doctor or therapist using his/her hands to stretch or relax dysfunctional soft tissue structures. While these techniques can be applied almost anywhere, they are especially useful for the paraspinal musculature that surrounds each vertebra of the spine [36].
2.
Spinal mobilization (LHVA), a type of passive movement of a spinal segment or region.
Spinal mobilization has been described as a gentle, often oscillatory, passive movement applied to a spinal region or segment to gently increase the passive range of motion of that segment or region [37].
3.




Muscle energy technique [38], a direct and active technique; meaning it engages a restrictive barrier and requires the patient’s participation for maximal effect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







