Cervical Strain: Whiplash
Eileen A. Crawford
Nader M. Hebela
CLINICAL PRESENTATION
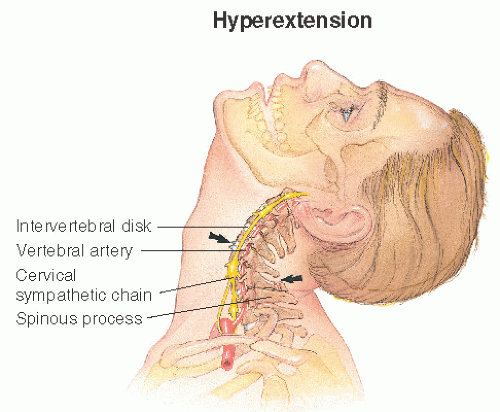
Whiplash, or cervical strain, is a term used to describe the cervical injury that occurs when the torso accelerates faster than the head, typically in a rear-end motor vehicle collision (MVC). Sports injuries and falls are other causes of whiplash. The injury does not result from a pure hyperextension force but rather a combination of extension of the lower segments and flexion of the upper segments (e.g., as the head strikes the headrest) that gives the cervical spine an S shape, like that of a cracking whip (Fig. 6-1). This abnormal combination of forces can disrupt the muscles, ligaments, facet joints, and intervertebral disks of the cervical spine.1 The symptoms that result from this injury are also commonly referred to as whiplash.
The primary symptom of whiplash is neck pain. Patients may report midline, bilateral, or unilateral pain, often referred to the trapezium and shoulders and sometimes even to the face. Neck pain caused by an MVC does not always arise immediately. Approximately 20% of individuals who experience chronic neck pain following an MVC do not experience neck pain the day of the accident.1 Radicular pain and paresthesias in the upper extremity may arise following a whiplash injury that produces a disk herniation or spinal stenosis. However, one should be cautious in ascribing all shoulder and upper extremity symptoms to the whiplash injury as MVCs can produce multiple distinct orthopaedic injuries. For instance, shoulder impingement syndrome and traumatic median neuropathy are seen in conjunction with whiplash injury following MVC.1
Headaches that result from whiplash injury are known as cervicogenic headaches. They are typically unilateral, starting in the neck or base of the skull and radiating to the crown of the head.
Patients seeking medical attention for a whiplash injury may report a variety of other symptoms that tend to occur with whiplash injury. They are known as “whiplash-associated disorders” and include low back pain, dizziness, tinnitus, visual abnormalities, fatigue, insomnia, poor concentration, and memory loss. Psychological disorders such as depression and posttraumatic stress disorder are seen in similar frequency to patients who experience other types of chronic musculoskeletal pain.1
CLINICAL POINTS
Whiplash is a sprain or strain of the muscles, ligaments, facet joints, and intervertebral disks of the cervical spine.
Neck and shoulder pain are the primary symptoms of whiplash.
Whiplash-associated disorders include headaches, low back pain, dizziness, tinnitus, visual abnormalities, fatigue, insomnia, poor concentration, memory loss, and psychological disorders.
PHYSICAL FINDINGS
Patients presenting for evaluation of whiplash are often wearing a cervical orthosis. Before removal of the orthosis, the examiner must assess for altered mental state (e.g., intoxication) or distracting injuries that could mask true abnormalities in the physical exam or prevent a patient from safely cooperating with the exam. The bilateral upper and lower extremity neurologic exam should also be performed prior to removal of the cervical orthosis.
Once these are ruled out, the patient should be reminded to hold the neck still while the orthosis is carefully removed. The skin may show signs of trauma such as ecchymosis or abrasions. Abnormalities in head positioning or alignment should also be noted. Tenderness to palpation of the paraspinous muscles is to be expected following whiplash injury, but tenderness along the spinous processes and palpable step-offs are signs of more extensive injury and should prompt replacement of the cervical orthosis without immediate range of motion testing. If no bone abnormalities are noted on examination of the neck, the patient should be directed to slowly flex and extend the neck, bend laterally toward each shoulder, and rotate the head, remarking on any discomfort. Neck range of motion is often fairly limited following whiplash injury because of the pain caused by stretching and contracting the injured tissues.
STUDIES (LABS, X-RAYS)
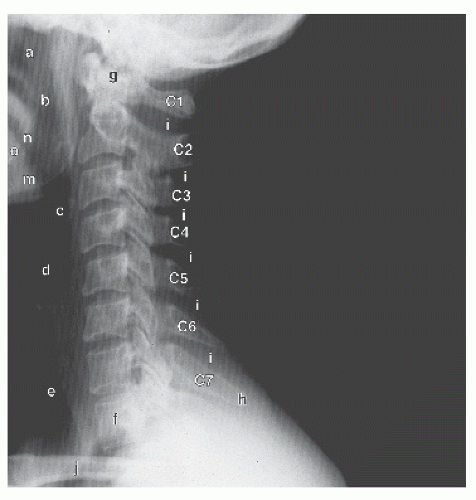
Whiplash is primarily a clinical diagnosis made from careful history and physical examination, so additional diagnostic studies are not required (Fig. 6-2). Signs that should prompt the clinician to obtain cervical spine radiographs include point tenderness along the spinous or transverse processes, severe pain with neck range of motion, and the presence of any neurologic disturbances. The Canadian C-Spine Rule (Table 6-1) is a clinical decision tool designed to determine if cervical radiographs are indicated for a patient presenting with neck pain following a trauma. It has a sensitivity of 99.4%, a specificity of 45.1%, and a negative predictive value of 100%.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree