Cervical Nerve Root Lesions
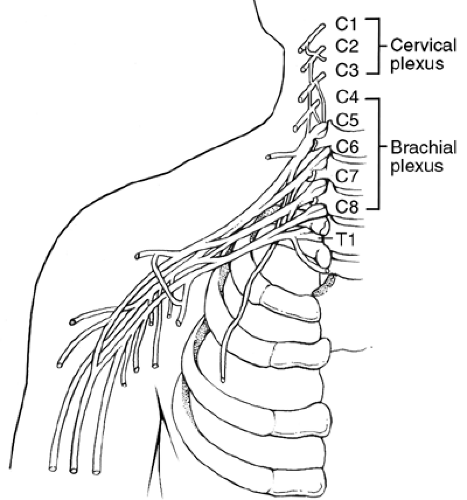
The cervical spine consists of eight pairs of spinal nerves. Each spinal nerve consists of a dorsal root (sensory component) and a ventral root (motor component). These nerve roots emerge from the spinal column through lateral intervertebral foramina. The first four cervical nerves collectively form the cervical plexus. The second four nerves, together with the first thoracic nerve, form the brachial plexus (Fig. 4-1).
If a nerve root lesion is suspected, you must evaluate three clinical aspects of the neurological examination: sensory, motor, and reflex dysfunction. Sensory testing attempts to delineate the segmental cutaneous innervation to the skin. It is done with a sterile or disposable Neurotip or pinwheel in specific dermatomal patterns.
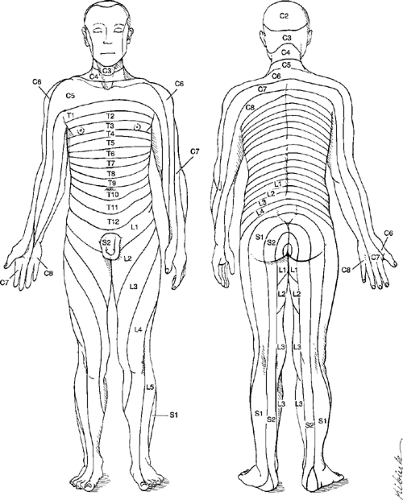
Two dermatomal maps are provided. Figure 4-2 is based on the body areas of intact sensation when roots above and below an isolated root were interrupted; sensation loss when one or more continuous roots were interrupted; or the pattern of herpetic rash and hypersensitivity when there is isolated root involvement. Figure 4-3 is based on the hyposensitivity to pin scratch in various root lesions and is consistent with electrical skin resistance studies showing axial dermatomes extending to the distal extremities. This pattern is useful in evaluating paresthesias and hyperesthesias secondary to root irritation. This is the pattern this chapter delineates to evaluate sensory root dysfunction. A fair amount of segmental overlap exists; therefore, a single unilateral lesion may affect more than one dermatomal level.
Motor function is evaluated by testing the muscle strength of specific muscles innervated by a particular nerve root or roots using the muscle grading chart adopted by the American Academy of Orthopaedic Surgeons (Box 4-1). The reflex arc is tested by evaluating the superficial stretch reflex associated with the particular nerve root. These arcs are graded by the Wexler Scale (Box 4-2).
The clinical presentation of nerve root lesions depends on two important factors: location and severity of the injury or pathology. These two factors together determine the injury’s clinical presentation. The possibilities are endless, ranging from no clinical presentation or slight clinical manifestation, such as slight loss of sensation and pain, to total denervation with loss of total function to the structures innervated by that nerve root (motor, reflex, and sensory).
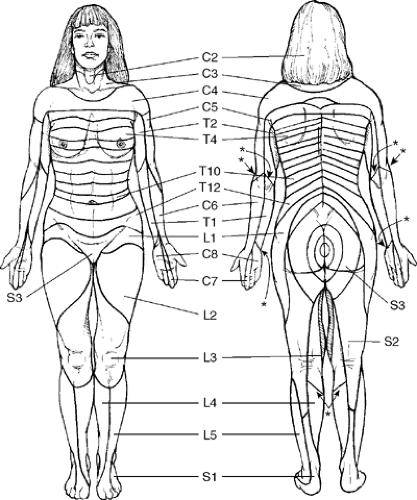 Figure 4-2. Adapted with permission from Haymaker and Woodall. Peripheral Nerve Injuries. 2nd ed. Philadelphia: WB Saunders, 1954. |
Box 4-1 Muscle Grading Chart
| 5 | Complete range of motion against gravity with full resistance |
| 4 | Complete range of motion against gravity with some resistance |
| 3 | Complete range of motion against gravity |
| 2 | Complete range of motion with gravity eliminated |
| 1 | Evidence of slight contractility, no joint motion |
| 0 | No evidence of contractility |
Each nerve root has its own sensory distribution, muscle test or tests, and a stretch reflex; these are grouped to facilitate the identification of the suspected level.
The clinical evaluation is not made solely on one aspect of the neurological package but is instead determined by the combination of history, inspection, palpation, the three individual tests (motor, reflex, and sensory) and appropriate diagnostic imaging and/or functional neurological testing, such as electromyography. Furthermore, the injury or pathology under evaluation may not necessarily be affecting a nerve root, but it may be affecting the brachial plexus, a trunk of that plexus, or a named nerve. Depending on the severity and location of the injury or pathology, various combinations of neurological dysfunction may be elicited.
Clinical Signs and Symptoms
Cervical pain
Upper extremity paresthesia
Diminution or loss of upper extremity sensation
Diminution or loss of upper extremity reflexes
Decrease or loss of muscle strength
Atrophic upper extremity lesions
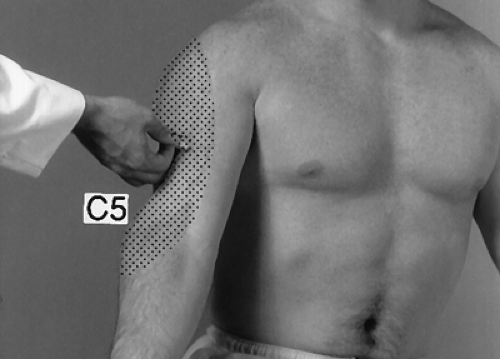
C5
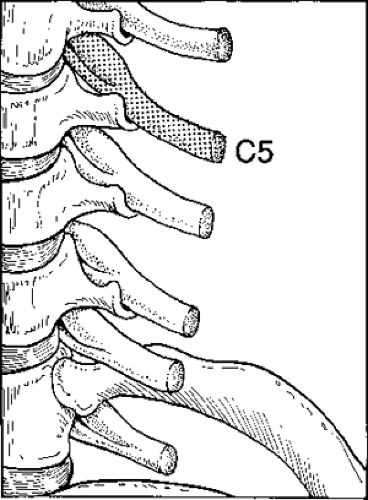
The C5 nerve root exits the spinal canal between the C4 and C5 vertebrae and may be affected by the C4 intervertebral disc (Fig. 4-4).
Motor
 |
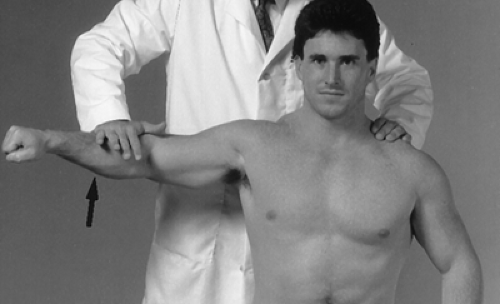
Procedure
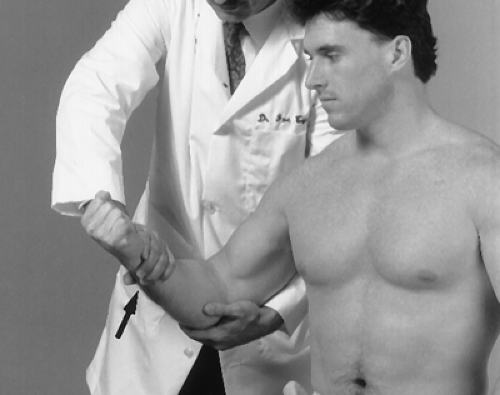
Stand behind the seated patient and place your hand at the lateral aspect of the elbow. Instruct the patient to abduct the arm against resistance (Fig. 4-5). Grade the strength according to the muscle grading chart. Perform this test bilaterally and compare each side.
Procedure
With the patient in the seated position and the forearm flexed, stabilize the patient’s elbow with one hand and grasp the anterior aspect of the patient’s wrist with your opposite hand. Instruct the patient to flex the forearm against resistance (Fig. 4-6). Grade the strength according to the muscle grading chart and compare each side.
Rationale
A grade of 0 to 4 unilaterally may indicate a neurological deficit of the C5 or C6 nerve roots, upper trunk of the brachial plexus, or musculocutaneous nerve. A weak or strained biceps muscle may be suspected if the sensory and reflex portions of the C5 neurological package are intact.
Reflex
 |
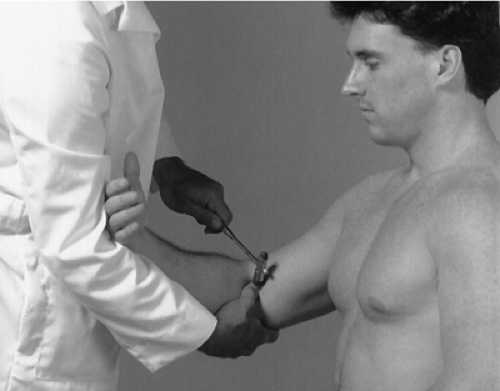
Procedure
Place the patient’s arm across your opposite arm with your thumb on the biceps tendon. Strike your thumb with the narrow end of the reflex hammer (Fig. 4-7). The biceps muscle should contract slightly under your thumb. Grade your response according to the reflex chart and evaluate bilaterally.
C6
The C6 nerve root exits the spinal canal between the C5 and C6 vertebrae and may be affected by the C5 intervertebral disc (Fig. 4-9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree