Cervical Laminoplasty
Patient Selection
Indications

Figure 1T2-weighted sagittal MRI demonstrates multilevel cervical stenosis secondary to spondylosis.
Cervical myelopathy due to ossification of posterior longitudinal ligament (OPLL) and multilevel spondylosis involving three or more motion segments (Figure 1)
Spinal cord decompression to salvage failed anterior cervical decompression and fusion (ACDF)
Recurrent myelopathy due to adjacent segment disease after anterior cervical decompression and fusion
Myelopathy in patients at increased risk for nonunion (smokers, patients with metabolic bone disease)
Developmentally narrow spinal canals (midbody AP diameter <12 mm)
Contraindications
Epidural fibrosis, following infection or prior posterior surgery
“Hill-shaped” lesions of OPLL occupying 50% to 60% of AP canal diameter
Axial neck pain as primary clinical symptom
Morbid obesity and diabetes mellitus (two- to eightfold increase in surgical site infections)
Lordotic or straight spines have significantly higher functional recovery than kyphotic or sigmoid-shaped curves; lordotic alignment not prerequisite for performing laminoplasty
Fixed kyphosis (5° to 13°); patients with cervical spines ranging from lordotic to 13° or less of kyphosis are ideal candidates if no cord signal change on T2-weighted MRI; if signal change present, upper limit of kyphosis is 5°
Types of Laminoplasty
Two main types derive from Hirabayashi “open-door” procedure and Kurokawa “French-door” technique
Preoperative Imaging
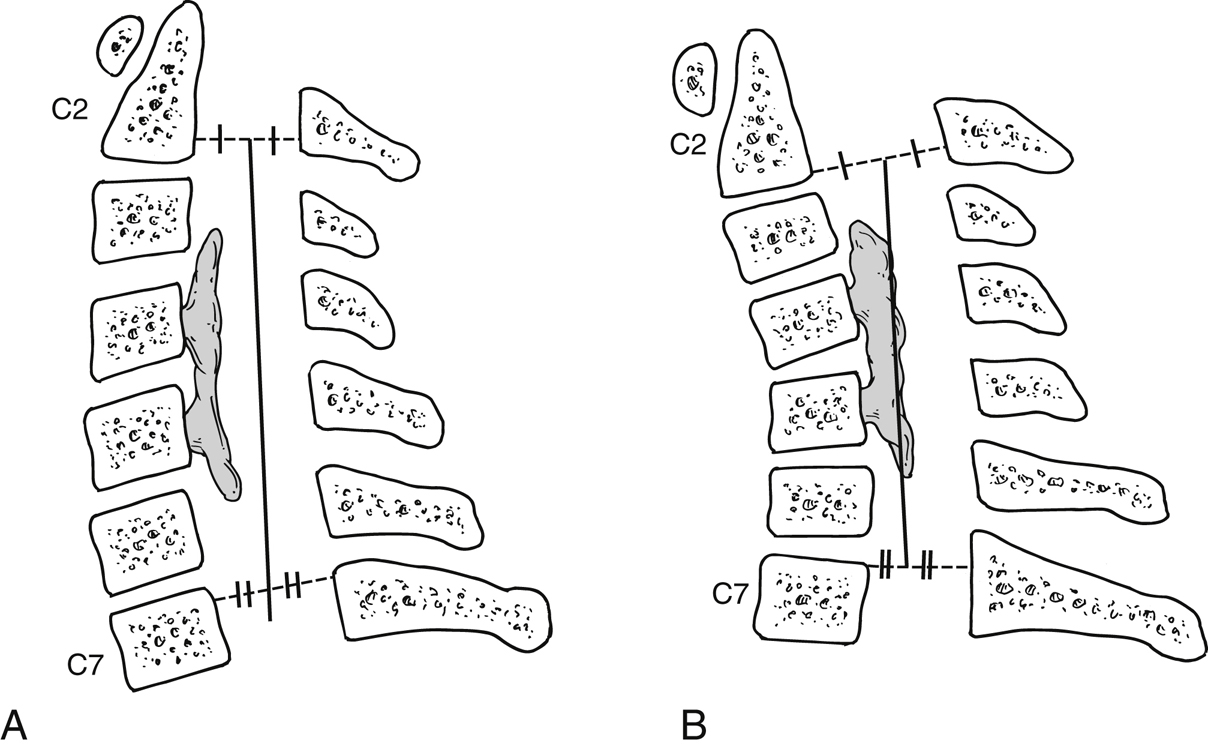
Figure 2Illustrations demonstrate the Kyphosis line (K-line) concept. A positive (+) K-line (A) occurs when the compressive pathology ossification of the posterior longitudinal ligament remains ventral to the line. A negative (−) K-line (B) is defined by the pathology extending dorsally to or across the line.
AP, lateral, and flexion-extension radiographic views
Kyphosis line (K-line) helps determine success of laminoplasty in OPLL; connects midpoints of spinal canal at C2 and C7 on lateral cervical radiograph (Figure 2)
MRI helps determine which levels to include in laminoplasty; helps determine whether C2 dome laminectomy should accompany laminoplasty
CT affords precise appreciation of bony anatomy including OPLL, ossified ligamentum, foraminal stenosis with osteophyte formation; surgeon can address foraminal stenosis detected on CT with foraminotomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


