Cervical Disk Herniation
Eileen A. Crawford
Nader M. Hebela
CLINICAL PRESENTATION
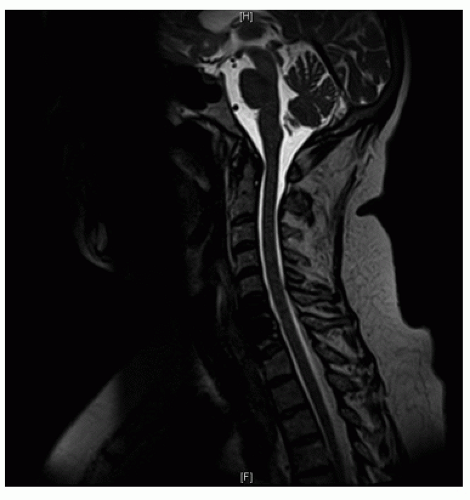
Herniated disk of the cervical spine refers to the displacement of part of the intervertebral disk material into the spinal cord or nerve roots of the cervical spine. Herniated disks of the cervical spine manifest in a variety of ways, from sporadic pain to progressive neurologic deterioration.
Intervertebral disks are composed of an outer layer called the annulus fibrosis, which surrounds and contains the inner layer, the nucleus pulposus. The inner layer, made of more gelatinous material, helps to act as a shock absorber, converting axial compression into tensile stresses, which are in turn absorbed and dissipated by the surrounding annulus fibrosis. The coordinated transfer to energy from axial load to tensile stress can be altered by changes in the nucleus pulposus, the annulus fibrosis, or both. A defect in the annulus fibrosis may result in migration of the gelatinous nucleus pulposus from the inner confines of the disk space, posteriorly into the spinal canal. Degeneration of the nucleus pulposus, the result of gradually deceasing water content as the result of age-related changes, may cause excessive tensile stresses on the outer annulus, causing tears that if large enough cannot contain in inner gelatinous material.
While the terms “bulging disk” and “herniated disk” are sometimes used interchangeably, they are distinct problems along the spectrum of disk degeneration. A bulging disk describes a broad prominence of the intact intervertebral disk beyond its normal vertebral border that is ubiquitous in the aging population and usually does not cause symptoms. With a true herniated disk, the annulus fibrosis is disrupted and a discrete portion of the nucleus pulposus protrudes beyond the normal border, often with compression of the nerve roots or spinal cord.1 In severe cases of disk herniation, fragments of the intervertebral disk can separate and become sequestered in the spinal canal as free fragments.
Cervical disk herniation is most common in the fourth decade of life and tends to affect men slightly more often than women. In acute cases, patients often report a specific incident, such as a fall or a motor vehicle collision. Chronic cases are more common in older patients. Cigarette smoking is another factor associated with cervical disk herniation.
While some people may be symptomatic only briefly, others may experience prolonged numbness and tingling, usually of the affected upper extremity. When herniated disks cause significant spinal cord compression, gait and balance difficulties, upper motor neuron findings (e.g., hyperreflexia, clonus, Babinski sign), and loss of strength may also result.
Patients may report pain after an acute traumatic event or pain that gradually worsens over a prolonged period of time. They may describe the pain as sharp, burning, or electric shock-like. Associated numbness and tingling may be present. Weakness may develop either acutely or over a more protracted time course. Patients often describe pain that starts in the lower cervical spine and radiates either to the left or the right in cases of unilateral disk herniations. The pain migrates into the periscapular region and then radiates along either arm into the elbows and finger tips. Pain and numbness at night are
common. Associated shoulder pain is frequently reported, but unlike pain that results from shoulder pathology, such as rotator cuff tears or glenohumeral arthritis, patients with cervical radiculopathy do not consistently report pain with overhead activities. Patients may also report stiffness and arm weakness. Symptoms may be specific and radiate along a specific nerve distribution or may be generalized along either arm diffusely.
common. Associated shoulder pain is frequently reported, but unlike pain that results from shoulder pathology, such as rotator cuff tears or glenohumeral arthritis, patients with cervical radiculopathy do not consistently report pain with overhead activities. Patients may also report stiffness and arm weakness. Symptoms may be specific and radiate along a specific nerve distribution or may be generalized along either arm diffusely.
In cases of central disk herniations that result in significant spinal cord compression, patients often describe difficulty with gait and balance, occasionally volunteering that “it feels like I’m walking as if I was drunk.” Unlike patients with lumbar stenosis, complaints of pain in the buttocks and radicular lower extremity pain are usually not reported. With spinal cord compression, difficulty with fine motor function may also be described.
CLINICAL POINTS
Symptoms of cervical herniated disks include neck and upper extremity pain, numbness, and weakness (nerve root compression).
Symptom onset may be acute (following a trauma) or insidious in onset.
Pain with overhead activities is more typical of shoulder pathology than cervical radiculopathy.
Difficulty with gait or balance, bilateral upper extremity weakness, and upper motor neuron signs may be the result of more severe pathology (spinal cord compression).
PHYSICAL FINDINGS
A thorough upper extremity examination helps gauge the severity of a patient’s complaints, especially in cases where there is reported weakness. The deltoid, biceps, wrist extensor, triceps, finger flexors, and hand abductor and adductor muscles are all tested on both sides (Table 8-1). Weakness generally manifests as an inability to fully resist the examiner’s counterforce. Cogwheel motions that initially start out as full strength and are followed by sporadic unexplained muscular weakness may be the result of pain, and distinguishing between the two helps the examiner to understand the true pathology caused by a herniated disk in the cervical spine.
Sensation to light touch is almost always preserved although more subtle two-point discrimination may be affected in the hands and fingers. Simply asking the patient of any subjective changes in their sensory examination suffices in determining the affected side and occasionally even the suspected level of disk herniation.
Reflex testing of the biceps (C5), brachioradialis (C6), and triceps (C7) is perhaps one of the most important aspects in understanding the effects of a herniated disk on the cervical spinal cord and nerve roots. Absent or blunted reflexes indicate compression of a specific nerve root, whereas hyperreflexia may be indicative of a more central herniation causing significant spinal cord compression and changes in the feedback loops that control peripheral deep tendon reflexes. For example, a herniated disk at C5-6 that compresses the exiting C6 nerve root may result in blunted brachioradialis or even triceps or biceps reflexes that are asymmetrical when compared to the unaffected side. However, a central herniation causing significant spinal cord compression may cause bilateral upper extremity hyperreflexia below the level of the disk herniation.
Perhaps nothing is as valuable in distinguishing cervical radiculopathy from cervical myelopathy as watching patients walk, especially as they turn. Subtle jerking motions of the lower extremity that exhibit an almost robotic gait pattern are characteristic findings in patients with cervical myelopathy and are absent in patients with isolated nerve root compression.
Provocative maneuvers also aid in this distinction between upper motor neuron compression (at the level of the spinal cord) and lower motor nerve compression (just distally, at the level of the neural foramen or below). A positive Hoffmann sign is a reasonable indicator of cervical spinal cord compression, especially in the presence of hyperreflexia and a myelopathic gait. Additional tests for diagnosing cervical disk herniation are Lhermitte sign and Spurling test, although they are neither very sensitive nor specific. Lhermitte sign refers to an electric-like sensation that occurs in the affected nerve distribution upon maximal forward flexion of the neck. A positive Spurling test involves reproduction of the described pain with extension of the neck while rotating the head toward the affected side and applying an axial load, thereby decreasing the space available for the spinal nerve roots in the neural foramen (Fig. 8-1). In contrast, holding the arm over the head, the abduction sign, often ameliorates the pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree