Cervical Disk Degeneration
Eileen A. Crawford
Nader M. Hebela
CLINICAL PRESENTATION
Cervical disk degeneration results from the wear and tear that accompanies aging and physiologic stress on the cervical spine. The water content of intervertebral disks decreases over time starting at the end of the first decade of life, causing the disks to become flatter and less elastic. In most cases, this process is asymptomatic. With progressive degeneration, however, osteophytes form around the vertebral end plates and facet joints, and the disk may herniate or be resorbed, resulting in ankylosis. Patients affected by cervical disk degeneration may experience neck pain due to inflammation, stiffness, nerve or spinal cord impingement, vascular compression, or mechanical instability.
As a degenerative condition, patients who present with cervical disk disease are typically older and may have a history of labor-intensive employment. Men are affected slightly more often than women and tend to have more severe disease. The symptoms of cervical disk degeneration can be divided into axial neck pain, radiculopathy, and myelopathy.
Patients with axial neck pain typically describe an insidious onset of soreness or achiness in the posterior neck with radiation into the shoulder, periscapular, or occipital region. Stiffness and headaches occasionally accompany the pain. A history of morning stiffness and involvement of multiple joints suggests an inflammatory arthritis and deserves a rheumatologic workup.
Cervical radiculopathy manifests as sensory and motor symptoms related to a specific dermatome and myotome, respectively. Patients will describe a localized region of numbness, tingling, or paresthesias in addition to neck, shoulder, and upper extremity pain. They may report improvement in symptoms when raising the affected arm overhead (abduction sign).
Cervical myelopathy has a variable presentation, but classic complaints include difficulty with fine motor tasks and lower extremity weakness. Patients may report clumsiness with buttoning a shirt and deterioration of their handwriting. The recent use of walking aids, such as a cane or walker, is also suggestive of myelopathy. Diffuse hand numbness that is not restricted to a specific dermatome is more likely to be myelopathic in origin. Urinary incontinence, urinary retention, and fecal incontinence are rare and suggest advanced myelopathic involvement.
CLINICAL POINTS
Cervical disk degeneration is a ubiquitous condition that comes with aging due to normal physiologic stresses on the cervical spine.
Neck and shoulder pain, headaches, and neck stiffness are the most common complaints of patients with cervical disk degeneration.
Patients may also experience symptoms of radiculopathy or myelopathy as the degenerative process leads to compression of nerve roots of the spinal cord.
PHYSICAL FINDINGS
Neck range of motion is typically limited and painful in cases of cervical disk degeneration. Postural changes that either reproduce or alleviate the pain provide clues to its etiology. Whereas neck pain from degenerative disk disease tends to be worse with extension, myofascial pain presents with posterior neck pain worsened by flexion (Fig. 7-1). Anterior neck pain localized to the sternocleidomastoid muscle and aggravated by head rotation is usually indicative of a muscle strain. In radicular pain, extending the neck, rotating the head toward the affected side, and applying an axial load (Spurling maneuver) tend to aggravate the pain.
Function of the upper extremity dermatomes and myotomes should be tested to detect radiculopathy. In terms of motor function, a C5 radiculopathy is characterized by deltoid weakness, a C6 radiculopathy by wrist extensor and biceps weakness, a C7 radiculopathy by triceps weakness, and a C8 radiculopathy by grip weakness. The C2 to C4 nerve roots do not have associated muscle weakness findings. Biceps and triceps reflexes should be tested on both sides to compare the intensity of the response as patients may have generalized weak or brisk reflexes at baseline.
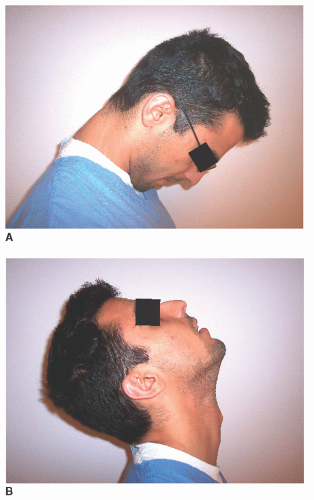 FIGURE 7-1. A and B: Patient demonstrating flexion and extension of the cervical spine during physical exam.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





