Cementless Acetabular Components for Revision Total Hip Arthroplasty
Christopher E. Pelt
Wes Madsen
Christopher L. Peters
Case Presentation
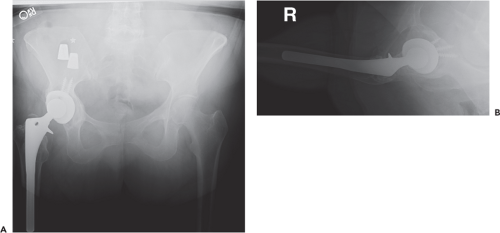
A 52-year-old female with a history of ankylosing spondylitis presents following multiple prior revision procedures with groin and buttock pain with activities of daily living (Fig. 109.1). The patient is otherwise healthy, taking narcotics chronically, married, and working. She denies smoking and illicit drug use. An infectious workup in our clinic was negative.
Introduction
Total hip arthroplasty remains among the most commonly performed and successful surgeries for the treatment of osteoarthritis (1). Despite the high success rate, as the volume of primary THA performed continues to increase, so too will the number of needed THA revisions (2). Common reasons for failure, and thus the indications for revision THA, include aseptic loosening, instability, osteolysis, and infection (3). The acetabular component is involved in the majority of revision THA surgeries and isolated acetabular revision accounts for at least 12% of all revisions (4).
Revision of the acetabular component often presents significant challenges to the treating surgeon, especially in the setting of deficient acetabular bone stock. Success depends on stable fixation and accurate positioning of the components. Given that instability remains a common cause of failure following revision THA, with dislocation rates reported to range from 9% to 21%, the necessity to achieve stable fixation must not compromise implant positioning (5,6,7).
Given the potential benefits of long-lasting biologic fixation, the relative ease of implantation, and good mid- to long-term results, the use of cementless acetabular revision
components is the most commonly used method for acetabular revision in North America (8,9,10,11). In the vast majority of revision THA cases a porous hemispherical cup (sometimes large diameter, or a so-called “jumbo cup”), typically with supplemental screw fixation and particulate bone graft, is appropriate for the acetabular revision. As host bone loss increases and available bone for fixation decreases, options become more complex.
components is the most commonly used method for acetabular revision in North America (8,9,10,11). In the vast majority of revision THA cases a porous hemispherical cup (sometimes large diameter, or a so-called “jumbo cup”), typically with supplemental screw fixation and particulate bone graft, is appropriate for the acetabular revision. As host bone loss increases and available bone for fixation decreases, options become more complex.
Preoperative Planning
Preoperative planning is imperative so that the surgeon may have available the most likely implants needed to successfully carry out the revision procedure. Proper surgical technique starts before entering the operating theater. Obtaining a thorough history and physical examination can provide valuable information about a patient’s prior postoperative course and potential mechanisms of failure. Further, it is always important to evaluate all failed or painful THA for the possibility of periprosthetic joint infection, given that treatment of infection is fundamentally different than aseptic failure.
High-quality plain radiographs are critical and can be used not only to identify component loosening but also to determine component positioning (Fig. 109.2) and to assess the remaining bone stock available for reconstruction. In some cases, advanced imaging such as computed tomography may be helpful in further determining bone loss and it can be used to objectively assess both acetabular and femoral component anteversion, if the scan includes the ipsilateral knee (Fig. 109.3). In our practice, we find the classification system of Paprosky most useful for preoperative planning, as the classification is not only predictive of the likely bone defects to be encountered, but can also help guide appropriate treatment.
Indications/Contraindications
Indications for using cementless hemispherical acetabular components include the ability to achieve osteointegration of the component to the host bone, which relies on the ability to obtain rigid fixation in the setting of both adequate host bone quality and quantity. As such, most cases classified as Paprosky types I and II are amenable to the use of cementless hemispherical acetabular components. Furthermore, in many types IIIA and IIIB, the acetabulum may be suitable for the use of a jumbo cup used alone or in conjunction with augments or bone graft.
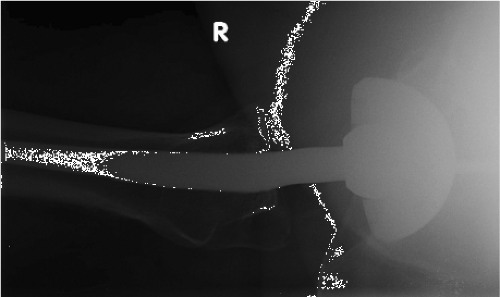 Figure 109.2. Shoot through radiograph showing acetabular component retroversion in a patient revised for recurrent instability. (Image courtesy of Craig Della Valle, MD.) |
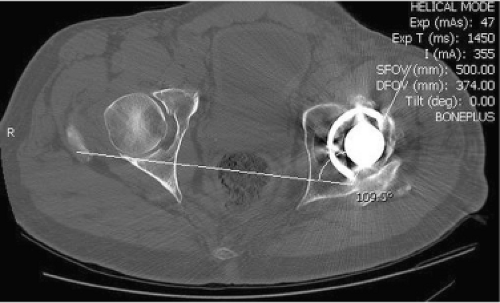 Figure 109.3. CT scan showing 19 degrees of acetabular component retroversion. (Image courtesy of Craig Della Valle, MD.) |
Cementless acetabular components should be avoided when the bone quality is compromised such that osteointegration cannot occur or if stable fixation cannot be achieved. Previous irradiation, typically greater than 5,000 cGy, or other host diseases can compromise the biologic activity of the bone and therefore the results of cementless acetabular revision (12). Pelvic discontinuity can create difficulty in the ability to achieve early rigid fixation, though posterior column plating may aid in achieving early stability and integration. Through the use of the various methods listed above, host bone contact can be increased or augmented via a variety of methods to increase the contact surface area available for osteointegration. Following these techniques (described in more detail in the following chapters), the vast majority of revisions can still utilize a cementless porous hemispherical shell.
Implant Design Considerations
The principles of implant design are no different than required in the setting of primary THA with appropriate pore size (50 to 300 μm) (13) and porosity (30% to 50%) with the reconstruction goals including minimal micromotion and gaps (<50 μm) (14) with satisfactory surface area contact between the component and host bone (15). In the setting of revision THA, the use of highly porous metals (Fig. 109.4), with their increased porosity (75% to 85%), biocompatible materials, a modulus of elasticity closer to that of bone, and a high surface roughness and coefficient of friction to aid in early stability, have largely replaced the use of more traditional shell designs for revision THA due to encouraging early and midterm results (16,17,18,19).
Supplemental fixation with screws is typically required to obtain rigid initial fixation, and the use of a multihole cup is recommended to increase both the number and location of screws for adjunctive fixation. Some of the highly porous revision cups are soft enough that the surgeon can drill through them, further increasing screw-placement options. Most modern porous cups have options for modular liner fixation, whereas others require a liner to be cemented inside the revision shell. Options for liners that can be placed into the cups include flat, elevated, face-changing and lipped polyethylene constrained liners or even ceramic liners. The use of highly cross-linked polyethylene, however, is generally used in our practice as it facilitates the use of larger-diameter heads which have been shown to decrease the risk of instability, the most common complication following revision THA (8). Some contemporary designs now offer the use of dual mobility bearings (Fig. 109.5), which may offer additional stability related to the added articulation after impingement along with a larger head diameter.
Surgical Technique
Regardless of the surgical approach, adequate exposure, while protecting nearby structures, is imperative to the successful revision THA. Our preference is a posterior approach which
is easily extended proximally under the abductors and distally along the lateral and posterior femur, including the use of an extended trochanteric osteotomy (ETO) (20), if indicated. In cases where patients have had prior surgical approaches, we will oftentimes utilize the same approach if reasonable.
is easily extended proximally under the abductors and distally along the lateral and posterior femur, including the use of an extended trochanteric osteotomy (ETO) (20), if indicated. In cases where patients have had prior surgical approaches, we will oftentimes utilize the same approach if reasonable.
Retention of the femoral component is frequent given the morbidity of removal of a well-fixed stem. However, the femoral component should only be retained if there are adequate modular head/liner combinations available and the stem is in adequate position to avoid the risk of instability postoperatively. In particular, we focus on the combined version of the cup and stem, so the femoral version must be appropriate to minimize the risk of dislocation. If the femoral component is to be retained, a pocket must be created superiorly for either anterior-superior (for the posterior approach) or posterior-superior (for the anterior approach) retraction of the femoral component (Fig. 109.6). For a posterior approach, release of the gluteal sling can further aid exposure of the acetabulum.
In cases where a well-fixed acetabular component is to be removed, the authors prefer using size-specific acetabular shell removal blades, such as the Explant Acetabular Cup Removal System (Zimmer, Warsaw, IN) or the CupX Acetabular Extraction System (Innomed, Savannah, GA) to help decrease bone loss (Fig. 109.7). These systems typically require an acetabular liner to be in place to centralize the head in the cup while cutting; however, acetabular fixation screws must be removed prior to attempted cup extraction. Larger heads are now available with these systems to facilitate the removal of monoblock metal-on-metal shells. Once the acetabular shell is removed all fibrous tissue, cement, or necrotic tissue needs to be meticulously debrided to expose the underlying healthy bone of the acetabulum where fixation of the new implant will occur; this also allows the surgeon to fully understand the acetabular defect encountered. The ilium, ischium, and pubis must be visualized and the bone stock continually assessed during the procedure noting any segmental or contained deficits.
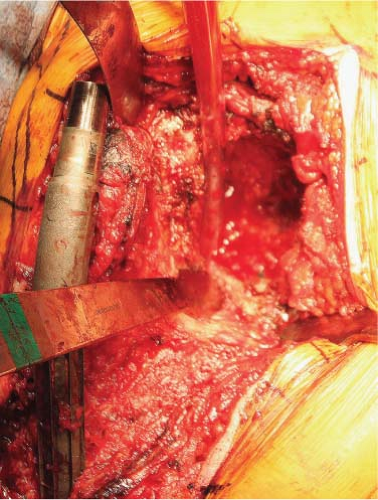 Figure 109.6. Posterior approach for revision THA showing retained femoral stem retracted anterior and superior to allow exposure of the acetabulum. |
Reaming should be performed in the position, inclination, and version of the intended cup placement. Positioning is aided by visualizing and palpating the remaining bone and comparing this to the preoperative plan (Fig. 109.8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree