Cemented Femoral Revision
Lucian B. Solomon
Margaret A. McGee
Donald W. Howie
CASE PRESENTATION
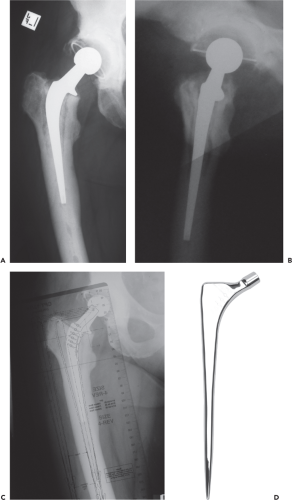
Mrs IL was 66 years old in 2001 when she presented with increasing pain in her left groin 4 years after a primary left total hip replacement (Fig. 124.1). Radiographic examination of the hip indicated loosening of both the femoral and acetabular components. The preoperative radiographs revealed a type IIIa femoral bone deficiency (1) in a moderately deformed femur.
Indications/Contraindications
At revision hip replacement, the choices for femoral reconstruction include cemented or cementless fixation. Cemented fixation may be with a long stem without the use of impaction grafting, so called cement alone revision, or with impaction grafting which restores femoral bone and enhances cement fixation. The most common indications for cemented long-stem revision are aseptic loosening, recurrent dislocation, second stage revision for infection in older patients, and type B periprosthetic fractures that can be easily reduced and held with cables and occasionally a plate.
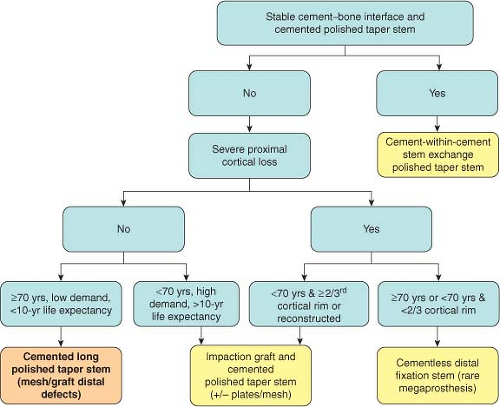
The factors that influence our decision whether to use cement alone revision include age, life expectancy, and activity of the patient and the extent of proximal segmental bone loss and loss of endocortex (Fig. 124.2). In general, we use long cemented stems in patients aged 70 years or older except for severe proximal cortical bone deficiency or extensive femoral endocortical loss after multiple stem revisions for which cementless distal fixation is used or rarely a cemented megaprosthesis.
In patients less than 70 years of age we use femoral impaction grafting with a cemented standard length or mid-length stems unless the patient has a life expectancy of less than 10 years in which case a cement alone long stem is used or for severe proximal bone deficiency in which cementless distal fixation is used. When distal cementless fixation is indicated, but the diameter of the distal femur is too large, femoral impaction grafting with a long cemented stem is used in these younger patients or a cemented megaprosthesis is used in the elderly (refer to Chapter 122).
Stem length for cement alone revision should be 200 mm or longer. Cemented long stems can be used for cortical deficiencies involving less than two walls of the canal that extend to 2.5 cm below the lesser trochanter, and up to 5 cm in elderly low demand patients in which case wire mesh and cement are used to reconstruct the cortical deficiency. Stems of 180 mm, but no shorter, should only be used for cement only revisions in the uncommon situations of relatively small femurs and when the medial femur is intact below the lesser trochanter or when combined with femoral impaction grafting (refer to Chapter 122).
Advantages of a polished, relatively narrow tapered stem are that when combined with cement, these stems fit within the damaged femur without the need to remove bone and moderate deformity of the femur can usually be treated without the need for a femoral osteotomy. Further, leg-length adjustments can be achieved easily by either seating the stem slightly proud or slightly recessed. Other advantages include rigid fixation which allows immediate full weight bearing and early rehabilitation; a particular advantage in older patients who cannot easily comply with partial weight bearing. A further advantage of a collarless, polished tapered stem is that it is effectively a modular stem within the cement mantle. This allows for stem removal from the cement in cases of re-revision for instability or acetabular revision for other causes followed by cement-within-cement stem revision and we and others have reported excellent results of this technique (2,3,4).
Early reports of revision hip replacement using either cemented or cementless femoral stems were typically poor. The results improved with better stem design and advances in surgical techniques and usually by the use of longer stems. In the case of cemented stems, better cementing techniques and possibly the use of tapered stems also lead to improved outcomes (5,6). We use a collarless polished double taper femoral stem (Fig. 124.1D) which is designed to undergo self-limiting subsidence within the cement. This enhances stability and transmits the compressive loads through the cement to the bone which thereby protects the cement–bone interface (7). This taper-slip principle has proven successful in primary hip replacement and, based on our experience and others, good results are now reported in femoral revision (8,9). The relatively thin distal stem also optimizes cement mantle thickness.
While our early experience included the use of standard stems, we have, in general preferred the use of cemented
long stems if a cement alone revision is performed. In our previous study of 206 hips that underwent femoral revision to a standard or long collarless polished tapered stem, it was found that at long-term follow-up that while overall clinical and radiographic failure due to loosening was very low, there was a trend for long stems to have a lower prevalence of loosening when compared to standard length stems (8). Moreover, the medium to long-term results with cemented long stems were as good or better than for many cementless stems even though more than 70% of femurs were classified as Paprosky type IIIa or worse, indicating moderate to severe bone loss. After cemented revision, severe stress shielding and osteolysis were found to be rare. To minimize stress risers and the potential for periprosthetic fracture, we bypass cortical defects by two canal diameters (10) and extend the femoral stem 5 cm past the areas of major endocortical damage.
long stems if a cement alone revision is performed. In our previous study of 206 hips that underwent femoral revision to a standard or long collarless polished tapered stem, it was found that at long-term follow-up that while overall clinical and radiographic failure due to loosening was very low, there was a trend for long stems to have a lower prevalence of loosening when compared to standard length stems (8). Moreover, the medium to long-term results with cemented long stems were as good or better than for many cementless stems even though more than 70% of femurs were classified as Paprosky type IIIa or worse, indicating moderate to severe bone loss. After cemented revision, severe stress shielding and osteolysis were found to be rare. To minimize stress risers and the potential for periprosthetic fracture, we bypass cortical defects by two canal diameters (10) and extend the femoral stem 5 cm past the areas of major endocortical damage.
Preoperative Assessment
Examination and Evaluation
The preoperative examination is thorough and in particular includes measurement of real leg-length discrepancy, Trendelenburg test, assessment of power of hip abduction and flexion, and palpation of the glutei to ensure the muscles are functioning. Preoperative patient and doctor derived evaluation of pain and function are important for reporting outcomes.
Radiography
Preoperative radiographic evaluation of the femoral component and femur is undertaken using an anteroposterior pelvis centered on pubis radiograph and a long-leg anteroposterior hip (Fig. 124.1C) and lateral/oblique hip radiograph showing the whole of the femur down to the supracondylar region.
Cemented Long-Stem Revision
Preoperative Planning
Careful preoperative planning is vital to the success of revision hip replacement. A general principle is to plan the most appropriate reconstruction for the individual patient needs, but to have other choices available intraoperatively.
Templating should be carried out for the acetabular component first and then the femoral component. The femur is templated to plan stem length, size, offset, depth of insertion, plug site, extent of bone grafting, and the need for proximal reconstruction. These may need to be modified according to intraoperative findings but provide a basis for planning. The surgeon should clearly delineate areas of major osteolysis, stress risers, femoral perforations and points of angulation or malrotation, all of these influencing the size and length of the stem required.
The template selected is one that best fits the proximal femur, leaving room for cement. It is not necessary to template
to achieve an even cement mantle. This allows for the use of the stems which are relatively large proximally. In patients with small femurs it is possible to insert a larger implant than the largest rasp that fits the proximal femur. For such cases, it is not necessary to completely seat the longer, revision rasps and in these situations the stem trials can be used to ensure fit within the canal. Because the long, polished stem is relatively forgiving, uneven and sometimes quite thin cement mantles can be tolerated when fitting the stem to a somewhat deformed femur.
to achieve an even cement mantle. This allows for the use of the stems which are relatively large proximally. In patients with small femurs it is possible to insert a larger implant than the largest rasp that fits the proximal femur. For such cases, it is not necessary to completely seat the longer, revision rasps and in these situations the stem trials can be used to ensure fit within the canal. Because the long, polished stem is relatively forgiving, uneven and sometimes quite thin cement mantles can be tolerated when fitting the stem to a somewhat deformed femur.
The femoral template is aligned so that it is centered in the diaphysis and then the template is moved so that the center of the femoral head and shoulder of the stem are appropriately positioned to restore the planned amount of leg length. While aligning the femoral template in the canal, the presence of incongruities or an excessive bow or angulation in the AP or lateral planes will become evident. After indicating the planned center of rotation on the radiograph, and the proper position of the femoral component, the optimal head position, and stem offset is determined. Limb length is predicted on the basis of the hip center and the height of the calcar and lesser trochanter, in conjunction with clinical measurement and preoperative radiographs. The appropriate relationship between the height of the tip of the trochanter, or other lateral landmark, and the center of femoral head rotation should be determined as well as potential difficulties in implant removal and insertion. If necessary, plan the level and type of femoral or trochanteric osteotomy and the bed for its reattachment. The need for proximal reconstruction and the extent of bone graft required should also be determined. These may have to be modified intraoperatively, but will provide a base for planning.
An important advantage of the collarless stem is that it can be adjusted proximally and distally to the required leg length. When templating, and intraoperatively, aim to achieve leg length without using the longer heads, which have a skirt. These are reserved for situations where an unplanned increase in leg length is required as the skirt can cause impingement against the liner leading to dislocation.
Surgical Technique
Specifics of Positioning, Draping, and Organization of Operating Room
Anesthesia by epidural catheter is routinely used for revisions and is often supplemented by a general anesthetic. Patients are placed in the lateral position, and anterior and posterior pelvic clamps are used to stabilize the pelvis. The pelvis is perpendicular to the operating table with the back parallel and the opposite hip flexed. A foam pad is placed between the knees and taped in place to allow knees and ankles to be palpated for leg-length determination. Small foam pads are used to cushion the underlying fibula head and lateral malleolus.
Preparation and draping is along standard lines with alcoholic chlorhexidine paint used to prepare the whole leg from the malleoli to nipple-line and across the midline, the groin being painted last. A large drape is placed over the contralateral leg to the groin, and another over the trunk above iliac crest. A U-drape is used to cutoff perineum but permitting maximal posterior access and leaving the iliac crest exposed. The leg is bagged with crepe bandage to just above the knee. Large paper or plastic disposable hip drapes are placed over the leg. An iodized Steri-Drape is folded double under the thigh and a large iodized drape over. Access should be available from the iliac crest and include the proximal two-thirds of the femur. The outer gloves are changed at this stage before starting incision. With the heels together, the positions of the flexed knees are compared as a guide to leg length.
Approach
Expose the hip joint using your approach of choice. More extensive exposure is generally required for revision surgery. An extensive exposure is recommended, especially in difficult revision cases. We would strongly recommend using a posterior approach. We do not usually use an extended trochanteric osteotomy but it can be used and if done, the osteotomy is reduced and wired prior to cementing. A straight distal skin incision centered over the greater trochanter and curving slightly posterior proximally toward the posterior one-third of the iliac crest is used with the hip flexed 20 degrees and adducted across the contralateral thigh.
There are key points during the exposure to which we pay particular attention. Firstly, as successful revision surgery is reliant on maintaining good abductor function, take time to clearly identify the gluteus medius muscle and tendon. The simplest way to do this is by performing the fasciotomy along the anterior margin of the gluteus maximus (Fig. 124.3A), identifying the anterior margin of maximus and developing the plane between the gluteus medius and gluteus maximus from anterior to posterior (Fig. 124.3B), eventually identifying clearly the plane between the main tendon posteriorly and the piriformis tendon (Fig. 124.3C,D). In this way the abductors will always be protected whereas, simply dividing gluteus maximus in the line of its fibers can cause devastating and irreparable damage to the medius in the common revision scenario where medius is adherent to maximus with scar tissue. We would always advise dividing the tendinous insertion of gluteus maximus from the femur during revision surgery to facilitate exposure and while doing this and while dividing the short external rotators, we place the foot on a padded, draped Mayo table so that the femur drops into some internal rotation allowing the sciatic nerve to fall away from the area of dissection. The sciatic nerve is identified in almost all cases, and having been visualized, its course is checked to make sure it is clear of the dissection. This does not require full exposure but at least palpation of the nerve course. In general, stay on bone during dissection. To control bleeding, use cutting diathermy frequently throughout the procedure.
Determine Leg Length
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree