CHAPTER SIX Case studies in neurological physiotherapy
Case study 1: Acute Stroke 100
Case study 2: Stroke Rehabilitation, Upper Limb Hypotonicity 102
Case study 3: Stroke Rehabilitation, Gait Disturbance 103
Case study 4: Head Injury, Acute Phase 105
Case study 5: Head Injury, Long-term Rehabilitation 107
Case study 6: Spinal Cord Injury at C3 109
Case study 7: Spinal Cord Injury at T5 112
Case study 8: Multiple Sclerosis, Relapsing–Remitting 115
Case study 9: Multiple Sclerosis, Secondary Progressive 117
Case study 10: Parkinson’s Disease 119
Case study 11: Guillain–Barré Syndrome 122
Case study 12: Motor Neurone Disease 124
Introduction
In neurological physiotherapy the evidence base for treatment interventions is a developing one (Pomeroy & Tallis 2002). Moves have been made by a number of researchers to identify what constitutes neurological physiotherapy. Studies by Ballinger et al (1999), Davidson & Waters (2000), Lennon & Ashburn (2000) and Lennon (2003), have begun to address this issue mainly in the form of surveys and focus groups. These studies have sought to isolate the components of neurological physiotherapy treatment and what concept of treatment physiotherapist’s professed to use. Previous studies by Nilsson & Nordholm (1992), Carr et al (1994), and Sackley & Lincoln (1996) as cited in Davidson & Waters (2000), identified that the main approach used by physiotherapists in the United Kingdom, although eclectic in nature, was based on the Bobath concept. This was supported by Davidson & Waters (2000) who reported that the majority of physiotherapists questioned (88%), professed to use the Bobath approach, although the majority of these also used other approaches in the treatment of their clients. The second most popular approach was identified as the Motor Re-learning Programme (MRP), though this was practised by only 4% of the respondents.
CASE STUDY 1 Acute stroke
Subjective assessment
PC
68-year-old male admitted via A&E following collapse at home
CT scan shows infarct of right middle cerebral artery
HPC
Ambulance called and patient transferred to A&E
Left sided weakness, reduced tone and reduced reflexes
DH
Simvastatin – for atherosclerosis
Commenced on IV antibiotics and IV fluids in A&E along with 300 mg aspirin
Objective assessment
Referred by ward staff to assess chest and initial bed mobility.
Observation
Positioned in bed with IVs in situ in right upper limb
Falling to the left with left upper limb hanging over the edge of the bed
Conscious and responsive, but drowsy, appears to recognise basic commands
No attempts to communicate, making eye contact only
CASE STUDY 2 Stroke rehabilitation, upper limb hypotonicity
Subjective assessment
PC
72-year-old female with right-sided hemiplegia primarily affecting the upper limb following CVA 6/52
Low tone in upper limb proximally with subluxation of glenohumeral joint
Objective assessment
Independently mobile on ward, returned to previous level of function with regard to mobility.
Sitting
Left scapula protracted, but can align with verbal prompting
Right scapula – reduced tone evident with scapula protracted and medially rotated
Right humerus medially rotated with significant subluxation evident
Unable to recruit activity at shoulder girdle or glenohumeral joint
Increased tone noted at elbow flexors with associated reaction evident on activity
Increased tone of right wrist and finger flexors – increasing with any activity
Questions
CASE STUDY 3 Stroke rehabilitation, gait disturbance
Subjective assessment
PC
55-year-old male admitted via A&E following collapse
CT scan showed sub-arachnoid haemorrhage (SAH) of the left anterior cerebral artery (ACA)
HPC
Complained of sudden intense headache while doing DIY at home
Collapsed and ambulance called – transferred to A&E
On arrival CT scan conducted which showed extensive SAH
Angiogram completed which showed ruptured berry aneurysm on the ACA
Transferred to regional neurosurgical unit, where urgent coiling procedure was completed
Following surgery transferred to ICU (3 days) followed by Neurosurgical HDU (6 days)
Transferred to neurological rehabilitation unit 3/52 post surgery
Continues to be closely monitored due to high risk of re-bleed in sub-acute phase
Objective assessment
Sit to stand
Weight bearing left > right with overuse of left upper limb evident
Decreased activity tibialis anterior with ankle remaining in plantarflexion throughout transfer
Questions
CASE STUDY 4 Head injury, acute phase
The following patient is on intensive care following admission via A&E 2 weeks ago.
Subjective assessment
PC
28-year-old male, admitted to ICU with extensive head injury following an assault
Ventilated and sedated, though sedation is being reduced as ventilator weaning commences
HPC
On admission GCS = 5, with some respiratory distress evident
Decision taken to sedate and ventilate
CT scan showed diffuse injury with development of oedema. No repeat CT scan conducted as yet
Now medically stable and sedation is being reduced and ventilator weaning commencing
Objective assessment
Increased tone in upper limbs bilaterally, with upper limbs demonstrating severe flexor patterns
Flexion at wrists, fingers and elbows with adduction and internal rotation at shoulder joints
CASE STUDY 5 Head injury, long-term rehabilitation
Subjective assessment
PC
22-year-old female, suffered a head injury 4 years ago following an RTA in which she was a passenger
On starting work, complained of high levels of fatigue. This has now settled
Complains of right leg feeling weak, with a fear of her knee giving way if walking any distance
HPC
MRI scan showed damage to the temporal and parietal lobes on the left due to a blunt piercing trauma
Underwent extensive surgery and rehabilitation at the time of injury
CASE STUDY 6 Spinal cord injury at C3
Subjective assessment
HPC
Sustained an incomplete disruption of C3 15/12 ago following a motorbike accident
Tracheostomy tube changed during chest infection, communicates effectively by staff lip reading
Objective assessment
You are asked to focus your attention on seating and positioning difficulties.
Passive movement
Passive movements performed to all upper limb joints
Shoulder extension difficult to assess due to positioning in bed
Nursing staff present report that this has become an increasing problem since chest infection and they are concerned about skin integrity. Patient reports hand position causing concern though wants to be able to sit out in wheelchair so that he can spend more time with his sons
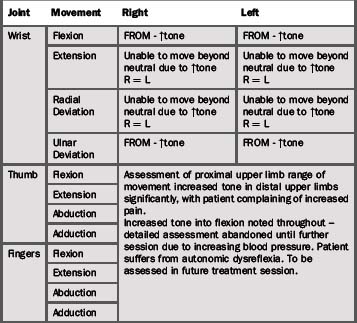
CASE STUDY 7 Spinal cord injury at T5
Subjective assessment
PC
Wearing brace which needs to be worn for 3/12 to maintain alignment at fracture site
Recently transferred to rehabilitation unit for intensive rehabilitation
Transferring with assistance of one or two with banana board
Anxious to be discharged – university course recommences in 2 months time and wants to return
HPC
Sustained a complete disruption of spinal cord at T5
No sensory function or motor function present below nipple line
Surgical intervention required to stablise anteriorly and posteriorly following injury
Becoming increasingly frustrated with lack of independence
Objective assessment
Brace in situ throughout assessment.
Lying to sitting
With assistance from one, able to push through upper limbs to move into long sitting
Unsupported sitting
Able to maintain sitting posture through overuse of upper limbs to increase base of support
Overuse of thoracic and cervical extension to maintain sitting posture
Unable to move within base of support in sitting or release upper limbs to enable function
CASE STUDY 8 Multiple sclerosis, relapsing–remitting
You have been asked to see the following lady in an out-patient setting by the multiple sclerosis (MS) specialist nurse following a recent relapse.
Subjective assessment
PC
Recent relapse mainly affected right lower limb, recovery slower than with previous relapses
Confidence affected considerably
Unable to drive at present as patient ‘does not trust’ right leg when braking
HPC
GP referred to consultant neurologist, who diagnosed MS following a number of investigations
Reviewed 6 monthly by Consultant and 3 monthly by MS nurse
Good recovery initially, though remaining symptoms have persisted
Objective assessment
Arrives for therapy session mobilising with husband, reports ‘linking’ as feels unsafe mobilising outside own home independently. Husband reports that his wife has been maintaining her balance by holding on to furniture while walking around the home.
Standing posture
Pelvis – anterior tilt, with increased lumbar lordosis
Centre of gravity falling posterior to the knee joint
Shoulders elevated bilaterally, unable to release upper limbs to ‘relax’ into standing posture
Gait
Decreased step length evident, with decreased heel strike on left and no heel strike on right
Decreased stance phase on right lower limb
Circumduction of right lower limb during swing phase, with decreased dorsiflexion during swing
Elevated shoulder girdles bilaterally, unable to release upper limbs to achieve reciprocal arm swing
CASE STUDY 9 Multiple sclerosis, secondary progressive
You have been asked to see the following gentleman at home by the home care team, who have reported increasing difficulty with transfers on visits to assist with personal care.
PC
Uses a powered wheelchair for indoor and outdoor mobility
Currently using a banana board with the assistance of one for all transfers
SH
Previously worked as a solicitor. Retired 10 years ago due to deteriorating health
Lives alone in a large detached bungalow, adapted to allow wheelchair access throughout. Level access shower and ramped access in situ
Divorced 12 years ago, two grown children live locally and are very supportive of their father
Objective assessment
Posture in sitting
Uses powered wheelchair for mobility indoors and outdoors
Seated in power-chair for 11 hours per day on average
Postural management system to provide lateral trunk support at ribcage
Retraction at right hip and increased tone throughout lower limbs
Pelvis in posterior tilt, increased tone in abdominals – unable to release to achieve anterior tilt
Transfers
Currently transferring with banana board with the assistance of one
Assessed with two due to moving and handling safety concerns raised by home care staff
Lateral trunk support removed to allow movement of trunk in sitting
Transfer attempt abandoned due to risks perceived to staff members
Patient reported that transfers were much more difficult later in the day due to levels of fatigue, though at time of assessment, participation not affected
Questions
CASE STUDY 10 Parkinson’s disease
Subjective assessment
HPC
Diagnosed 10 years ago, following a number of falls outdoors
Monitored primarily by Parkinson’s disease specialist nurse 6 monthly at clinic. Appointments are arranged to coincide with daughters visits
Reports difficulty getting in and out of daughter’s car when attending last clinic appointment
Objective assessment
Supported sitting
Kyphotic sitting posture, with protracted and depressed shoulder girdles
Mask-like face and considerable pill rolling tremor. No other added movements noted
Sitting in deep armchair, with low seat height – feet raised on stool to prevent ankles swelling
Difficulty adjusting position in sitting. Unable to initiate weight transfer to alter base of support. Chair cushion very soft contributing to difficulties