CHAPTER EIGHT Case studies in a musculoskeletal out-patients setting
Introduction
Musculoskeletal problems are very common, and can be encountered in hospital emergency departments, orthopaedics, and out-patient physiotherapy (Carter & Rizzo 2007). It is not uncommon for in-patients who are admitted for another problem to be referred and treated in the ward or in the out-patient department for a musculoskeletal problem. The prevalence of specific conditions can vary between the different groups in the community. For example, sporting injuries are more likely to occur in the younger groups, whereas degenerative conditions such as osteoarthritis are more likely to occur as people progress in years.
Musculoskeletal problems can result in pain and functional limitations (disability), and represent a major burden to the society due to associated health care costs and loss of productivity (National Health Priority Action Council 2004). Musculoskeletal conditions, including arthritis, cause more disability than any other medical condition and affect one-third of all people with disability. Since part of the chronic disease burden is attributed to risk factors such as physical inactivity (Bauman 2004) people with musculoskeletal conditions are often referred to physiotherapy out-patients for management of their conditions.
As in other areas of physiotherapy practice, musculoskeletal assessment and treatment requires a systematic clinical reasoning approach (Edwards et al 2004). The clinical reasoning approach used in this chapter considers: (i) differential diagnoses based on assessment and clinical presentation; (ii) intervention based on the best evidence available; (iii) constant evaluation of therapy outcomes; (iv) adjustment of intervention programme in line with diagnosis and stage of progress; and (v) referring to or working together with other disciplines to exclude and or address confounding problems. In assessing and treating common musculoskeletal conditions and measuring progress it is important to use outcome measures that are valid and reliable, and that consideration must be given to impairments of body structure and function as well as activity limitation and participation restriction, such as ability to return to work. The World Health Organization’s International Classification of Functioning, Disability and Health (ICF) provides a useful framework for physiotherapists in out-patients to assess patient functioning (Jette 2006). Referral to or working with other disciplines may involve tests such as X-rays or dynamic ultrasound scans, or the provision of orthotics to improve biomechanics. In addition to specific techniques, treatment may require education, ergonomic advice and the instruction of a home exercise programme to improve outcomes on function and pain.
There is an emerging and increasing body of research on the effectiveness of physiotherapy that provides the clinician in out-patients with an evidence base for their practice (Herbert et al 2001). For example, there is high level evidence that therapeutic exercise can benefit clients across broad areas of physiotherapy practice (Morris & Schoo 2004, Taylor et al 2007). In prescribing exercises it can be important to know whether the exercise programme is performed correctly and adhered to by the client. Conditions such as back problems or tendinopathies may be negatively affected by incorrect activity performance. Additional problems that can affect health outcomes are incorrect belief systems and mental health problems. For instance, people with osteoarthritis may think that movement harms the joint, but by not moving they put themselves at risk of developing problems associated with physical inactivity (e.g. increased morbidity and mortality due to cardiovascular problems or falls) (Philbin et al 1996). Also, people with chronic pain may be depressed and are, therefore, less likely to be interested in performing exercises, and may benefit from counselling (e.g. motivational interviewing). Screening patients for problems such as fear-avoidance behaviour and anxiety (Andrews & Slade 2001), asking about past and current exercise performance, motivating them if needed (Friedrich et al 1998) and demonstrating the prescribed exercises can assist in determining the likelihood of correct and consistent programme performance (Friedrich et al 1996b, Schneiders et al 1998).
CASE STUDY 1 Jaw pain
Subjective examination
HPC
Left sided headaches off and on for 3/12
Increasing pain of the left temporomandibular joint (TMJ) last 2/12
Pain at night, at rest, and when opening the mouth or chewing
CASE STUDY 2 Headache
Subjective examination
HPC
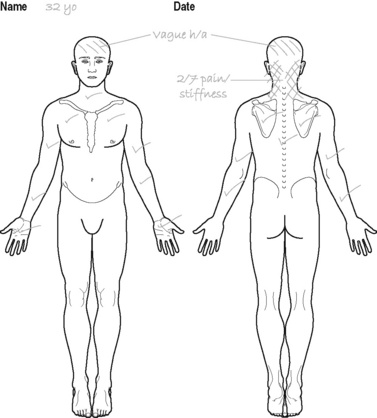
Gradual onset of headaches and cervical pain about 3/52 ago
Cannot recall precipitating incident
Headaches becoming more frequent (now daily) and lasting longer (up to 3 hours)
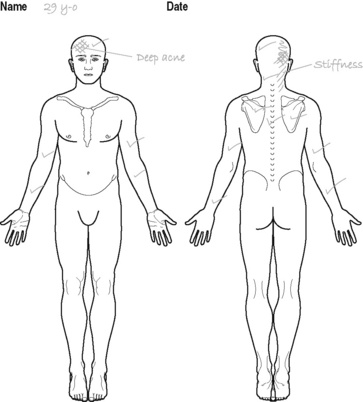
Has deep ache (non-throbbing) radiating from the back of the occiput to the right frontal region. Also complaining of stiffness like pain in the right side of the cervical spine. Neck pain and headache seem related (see Figure 8.1)
General health
In good health, no weight loss
No complaints of dizziness, no nausea or vomiting
Assessed as being depressed, has been taking antidepressants over the last 3/12
Physical examination
Palpation
Hypo-mobility of upper cervical joints on the right, with reproduction of local cervical pain
Increased muscle tone in right upper trapezius and right levator scapulae
Movements
Active movements
Right cervical rotation equals 60° with slight stiffness in neck
Left cervical rotation equals 75–80°
Neurodynamic testing
Upper limb neurodynamic/tension test (base test): In 90° shoulder abduction and full external rotation, right elbow extension lacks 40° while left lacks 30°. Reproducing local neck pain, which is eased with cervical lateral flexion towards the right
CASE STUDY 3 Neck pain – case one
Subjective examination
HPC
Prolonged sitting (all day) at a conference 3/52 previously
Noticed onset of left lower cervical and interscapular pain at the end of the day
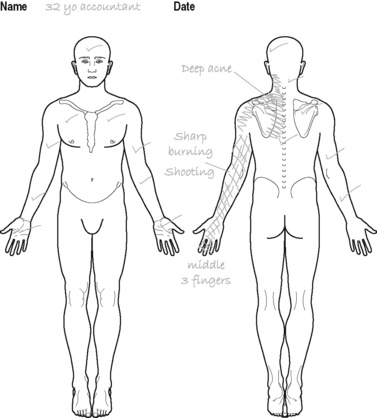
On waking the next morning pain had spread to the posterior aspect of the arm and forearm as far as the middle three fingers (see Figure 8.2)
Medical history
High cholesterol, overweight, sedentary lifestyle
Minor neck complaints that usually settled within 2 or 3 days
Aggravating factors
Sitting for more than 10 minutes increases neck pain. More than 30 minutes increases arm pain
Looking up or to the left increases neck and arm pain
Lifting briefcase with left hand aggravates neck and interscapular pain
Physical examination
Cervical active movements in sitting
Right rotation produces a stretching in the left cervical region at 75°
Left rotation reproduces left neck and interscapular pain at 40°
CASE STUDY 4 Neck pain – case two
Subjective examination
Aggravating factors
Turning head to either side, especially if movement is quick
Travelling in car – took 20 minutes to settle after 30-minute car trip
General health
Taking non-prescription analgesics every 4 hours on advice of doctor. No other medications
Physical examination
Palpation
Generalized tenderness to light palpation of cervical spine (central, left and right)
Increased muscle spasm left and right paraspinal muscles
Further detailed palpation not possible because therapist wary of exacerbating symptoms
CASE STUDY 5 Thoracic pain
Subjective examination
Subject
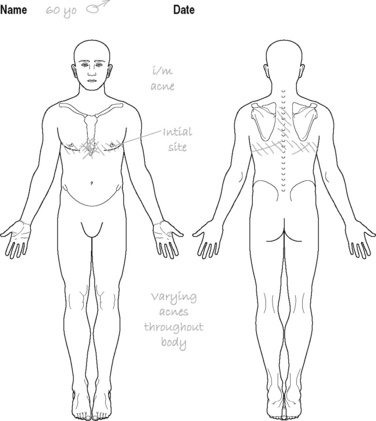
Presents with bilateral lower thoracic pain with radiation of symptoms anteriorly to the lower sternal area (see Figure 8.4)
Medical history
Noticed 5 kg of weight loss in previous 4/52 that could not be explained by other factors
Physical examination
Thoracic active movements in sitting
Thoracic rotation feels stiff but no pain reproduced
Flexion is normal in range and reproduces a stretching feeling in the mid thoracic area
CASE STUDY 6 Low back pain – case one
Subjective examination
HPC
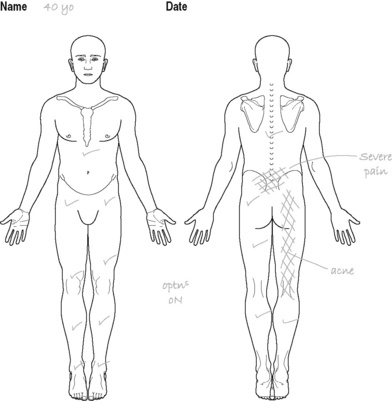
Next morning severe low back pain with aching pain radiating down the back of the right leg to just below the knee. Has no pins and needles or numbness (see Figure 8.5)
Aggravating factors
Finds it difficult to put shoes and socks on in the morning
After driving to work (about 40 minutes) found leg pain had worsened
Can only sit for about 15 to 20 minutes at a time at work
Night
Pain gradually eases after initial discomfort
Is waking at night but finds can get back to sleep quite quickly when changes position
Daily pattern
Back stiff and aches getting out of bed first thing in the morning but eases after shower
Back pain is worse by the end of the day, and leg pain is more constant by the end of the day
Attitude/expectations
Very keen not to miss club Stableford golf competition this weekend (in 3/7)
Intending to cope with work as best he can. Very busy at work so reluctant to take time off
Physical examination
CASE STUDY 7 Low back pain – case two
Subjective examination
HPC
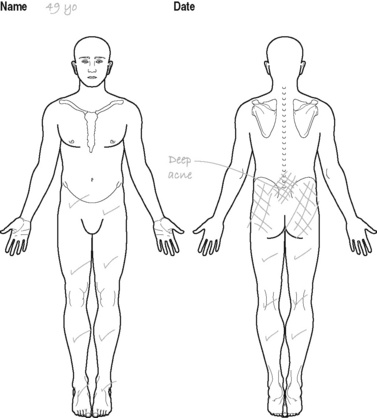
Complaining of increasing back pain over the last 14/12. Back pain is in the central low back region and radiates into both gluteal regions – no leg pain (see Figure 8.6). Has been off work for the last 6/12 with no improvement in pain
Has had manipulative physiotherapy involving manipulation, mobilisation and traction with no benefit. Also tried chiropractic without benefit
Aggravating factors
Prolonged walking or standing (more than 15 minutes) increases ache
Prolonged sitting (more than 15 minutes) increases ache
Unable to do weekly shopping or housework as these activities aggravate the ache
Easing factors
Lying down but only for about 30 minutes, as gets stiff when lying in one position for too long
General health
Has gained weight over the last 14/12 (about 6 kg)
Assessed as being depressed, has been taking antidepressants over the last 3/12
Investigations
X-ray shows mild bilateral degeneration of the L4–5 facets
CT scan shows a minor disc bulge at L4–5 and L5–S1 with no nerve root involvement
Attitude/expectations
Has reduced activity level to avoid aggravating back
Believes that if she can find the right practitioner then they will fix her
Very concerned with the CT scan report and the diagnosis of disc pathology
Has been more short-tempered with family and friends since her back problem began
Physical examination
Observation
Exhibits pain behaviours including grimacing, and placing hand on back
Changes position regularly when sitting and standing
Palpation
Central palpation of the lumbar spine at L1, L2, L3, L4 and L5 painful
Unilateral pressures are painful left and right at L1, L2, L3, L4 and L5
CASE STUDY 8 Shoulder pain
Subjective examination
Daily pattern
Constant nagging pain that worsens during activities as mentioned above (see aggravating factors)
Attitude/expectations
Wants better duties within the factory as some of her colleagues have managed to do
Objective examination
Standing with arms relaxed
Shoulders protracted and depressed (right > left)
Right shoulder abducted and elbow flexed
Functional and other testing, including ROM
Painful arc when abducting arm (90–115° abduction) with audible click (VAS rises to 6 during this impingement)
Hawkins and Kennedy impingement test (compressing the subacromial tissues by internal rotation in 90° shoulder flexion) was positive (Ginn 2003) and VAS rises to 8
Apprehension test for shoulder stability and SLAP lesion tests were negative, indicating integrity of joint capsule, labrum and ligaments (Brukner et al 2001e, Ginn 2003, Hoppenfield 1986)
Pain on resistance against external rotation and abduction (VAS rises to 8)
CASE STUDY 9 Elbow pain
Subjective examination
HPC
Right lateral elbow pain off and on for at least 5/12. Insidious onset
Worsened 4/52 ago when his nail gun broke down and he was forced to use a hammer all day
General health
No other health problems reported. Not using any medication or receiving any other medical care
Attitude/expectations
Is disappointed that his elbow problem hasn’t improved over time as his other injuries did
Experiencing increasing problems at work. Is afraid that he will lose his job
Expects that it may take some time since he wants to stay at work
Objective examination
Palpation
Lateral epicondyle extremely painful with some palpable swelling
Tenderness extensor carpi radialis brevis and longus
Thickening in extensor carpi radialis brevis (ECRB)
Difficult to palpate for tenderness of capitellum radii due to surrounding tissue swelling and pain
Functional testing, including ROM and strength
Elbow extension showed pain in at end of ROM (VAS rises to 6)
Forearm pronation/supination showed full ROM (VAS rises to 5)
Reduced grip strength (VAS rises from 4 to 9 during firm gripping)
Difficulty opening pushing door handle and opening door (VAS rises to 7)
Difficulty lifting an object with palm of hand facing down (VAS rises to 8)
CASE STUDY 10 Hand weakness and pain
Subjective examination
PMH
Knee arthroscopy with partial left medial menisectomy 12 years ago after tennis injury, recovered well
Aggravating factors
Gripping (tennis racquet after 1 set, a feeling of weakness)
Packing up play equipment at kindergarten
Easing factors
Gets a little relief from changing position and shaking out wrist
Aspirin (started aspirin 2/52 ago on advice of GP), may have helped a little
Attitude/expectations
Enjoys her regular exercise (especially tennis) so is keen to get the problem fixed
Physical examination
Palpation
Slight reduction to light touch on the palmar surface of the right thumb and 1st and 2nd finger
Movement (right side)
Wrist extension = 55°, no pain
Wrist supination = 90° from mid-prone, no pain
Wrist pronation = 90° from mid-prone, no pain
Finger MCP flexion OK, no pain
CASE STUDY 11 Groin pain
Subjective examination
Aggravating factors
Running, especially when sprinting and when cutting (changing direction)
Kicking, especially when taking a corner
Daily pattern
Symptoms are dependent on activity. Now affecting whenever tries to run or kick a ball
Attitude/expectations
Concerned that the problem appears to be getting worse. Had thought it would just go away
Physical examination
Observation
In standing, no obvious wasting or pelvic asymmetry
With walking, observed excessive pelvic tilting (obliquity) in the frontal plane
Palpation
Tender to palpation at tendon attaching to right medial inferior pubic ramus
Trigger point tenderness to muscle belly distal to medial inferior pubic ramus
Movement
Right hip flexion = 130°, no pain = left
Right hip extension = 25°, no pain = left
Right hip abduction = 45°, pain (VAS = 3), left = 55°
Functional testing
 Squeeze test (patient supine with hip flexed 45°, examiner places fist between patient knees, and asks patient to bilaterally adduct) reproduced right groin pain (VAS = 4)
Squeeze test (patient supine with hip flexed 45°, examiner places fist between patient knees, and asks patient to bilaterally adduct) reproduced right groin pain (VAS = 4) Right hip quadrant (passive hip flexion, adduction and internal rotation) only very slight pain, similar to discomfort when tested on the left side
Right hip quadrant (passive hip flexion, adduction and internal rotation) only very slight pain, similar to discomfort when tested on the left side Thomas test (slight restriction on right compared to left with only slight reproduction of pain (VAS = 0.5) when hip flexion resisted)
Thomas test (slight restriction on right compared to left with only slight reproduction of pain (VAS = 0.5) when hip flexion resisted)Questions
CASE STUDY 12 Hip and thigh pain
Subjective examination
Night
Wakes up frequently, particularly when lying on right side, or on left side with right hip in adduction and knee resting on the mattress
Objective examination
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree