Abstract
Objective
To assess care related pain during a program of functional restoration for chronic low back pain.
Patients and methods
Chronic low back pain patients were prospectively included in a program of functional restoration. Low back pain was recorded before and after each morning and afternoon sessions, all over the program of functional restoration, for equivalence study. Equivalence was admitted if 95% confidence interval of the difference in pain falled wholly in the interval ± 10/100 mm. Medication was recorded during the program. Progression of the patients during the program and 3-month effectiveness were also recorded for internal validity.
Results
Thirty-seven patients were included. They underwent a progression in load and spent energy during the program. Follow-up also indicated improvement of functional ability and quality of life. There was no variation in pain during the program however medication intake increased.
Conclusion
There was no significant care related pain during our program of functional restauration for chronic low back pain. This may be due to adaptation of the medication and suggests the importance of close medical management of patients during functional restoration.
Résumé
Objectif
L’objectif de ce travail était l’étude de la douleur induite au cours d’un programme de restauration fonctionnelle pour lombalgie chronique.
Patients et méthodes
Des patients lombalgiques chroniques ont été inclus de façon prospective dans un programme de restauration fonctionnelle de quatre semaines. La douleur lombaire a été recueillie au début et à la fin de chaque demi-journée de rééducation, tout au long du programme. L’analyse a été construite sur le mode d’une étude d’équivalence, avec pour hypothèse à rejeter une variation de la douleur après demi-journée de rééducation supérieure à 10/100. La médication, la progression effective par paliers hebdomadaires et l’efficacité de la restauration fonctionnelle à trois mois ont également été évaluées.
Résultats
Trente-sept patients on été inclus. Ils connaissaient une progression en charges déplacées et en dépense énergétique, ainsi qu’une évolution favorable en termes fonctionnel et de qualité de vie à trois mois. Aucune variation de la douleur n’a été notée en cours de programme. En revanche, une augmentation du recours aux antalgiques et aux antidépresseurs était notée en fin de programme.
Conclusions
La restauration fonctionnelle pour lombalgie chronique n’apparaît pas pourvoyeuse de douleur induite pour peu qu’elle comprenne une adaptation de la médication au cours du programme.
1
English version
1.1
Introduction
Care-related pain is an aspect of our medical practice that is often poorly known and understood . It may be defined as increased or triggered pain taking place during a diagnostically or therapeutically oriented medical act. Data on the subject in the framework of functional restoration for chronic low back pain are few and far between . Even though the principle of functional restoration for chronic low back pain is supported by a strong set of arguments combining a coherent theoretical proposition with demonstrated functional and professional efficacy, questions pertaining to induced pain appear altogether legitimate . Experience has shown that the answers to these questions interest not only the clinician, but also the patients to whom functional restoration is proposed, and for whose sake induced pain needs to be explored. Results could contribute to improved acceptance by candidates for functional restoration for chronic low back pain of a program likely to be optimized.
Up until now, to our knowledge no study has been elaborated and conducted for the purpose of evaluating tolerance and a fortiori the pain induced during functional restoration programs for chronic low back pain. At this time, these aspects can be apprehended only indirectly, taking into account the overall number of withdrawals from studies, the number of withdrawals due to recurring pain and, in an efficacy study, weekly measurement of pain undergone during the program . This state of the science has led us to carry out prospective work of which the principal, predetermined objective is the study of pain, in this case low back pain, during functional restoration addressing the latter. In order to ensure reliability with regard to the observation conditions and to consequently to the internal validity of the study, the authors have taken into close account the progress recorded over the course of a program of which the short-term efficacy has likewise been taken into consideration . From an explanatory standpoint, the medication taken during the functional restoration program has likewise been assessed.
1.2
Patients and methods
1.2.1
Inclusion
The chronic low back patients managed in the functional restoration center were prospectively included. The inclusion criteria were as follows: age above 17 years and below 66 years, non-specific low back pain for at least 3 months, comprehension of spoken and written French, adherence to the therapeutic project, and signature indicating informed consent to participation.
Low back pain could be associated with radiculalgia provided that its intensity was not greater than that of the back itself, which could also be associated with the presence of disc disease, discal hernia or posterior inter-apophysary arthritis. It was possible for the patients to have been operated (discectomy, laminectomy, arthrodesis) at least 6 months previously. They were recruited through hospital consultations in the physical medicine and rehabilitation, rheumatology and orthopedic surgery units and through consultations in town-based practices, as well.
1.2.2
Program
The functional restoration program was carried out in a rehabilitation center, during full-time hospitalization, 5 days a week for four weeks, in groups of three to five patients. It involved a physical medicine and rehabilitation physician, a psychiatrist, kinesiologists, occupational therapists, nurses, and nurses’ aides. The exercise program consisted in: relaxation, muscle strengthening, and aerobic activities from 9 am to 12 pm, and handling and supporting a load, relaxation and aerobic activities from 1 pm to 5 pm. No non-medical analgesic treatment was planned.
Upwards progression in muscle strengthening, load handling and aerobic activities was achieved according to predetermined weekly levels. Criteria for progression were the number of exercises by series, the load supported for muscle strengthening and handling, and the duration of the aerobic activities.
1.2.3
Evaluation
The patients included were evaluated before, during and after the functional restoration program, at 1 month and at 3 months.
Low back pain during the program was evaluated on a visual analog scale (VAS) from 0 to 100. Pain assessment took place four times a day, before and after the morning rehabilitation program, at 9 am and at 12 pm, as well as before and after the afternoon rehabilitation program, at 1 pm and at 5 pm, every day. Medication was evaluated on the first, the seventh, the twelfth, the seventeenth and the twentieth day of the functional restoration program. During each evaluation phase, intake of analgesics (Level I and Level II), anxiolytics and anti-depressant medicines was recorded. Prescription of muscle relaxants, which is relatively rare in our practice, was not evaluated. The physician in charge of medication during the program was not informed of the study methods and procedures.
As regards the study’s internal validity, the criteria of week-by-week upwards progression during the functional restoration program were: the daily load (in kg) moved during the muscle strengthening and handling phase, as well as daily energy expenditure (in kJ) during the aerobic activities . The energy expended was calculated from the power developed and the time spent each day on the ergonomic bicycle. The efficiency criteria for the functional restoration program were pain as measured on the VAS from 0 to 100 and the functional limitations evaluated on the Roland Morris and Quebec back pain disability scales , anxiety and depression as assessed on the HAD scale , quality of life as graded on the Dallas scale , and finally the patient’s perception of overall improvement in a binary yes/no mode. The different criteria were addressed before and after functional restoration, at 1 month and at 3 months. Professional activity was evaluated before functional restoration, at 1 month and at 3 months.
1.2.4
Statistics
Analysis of results was organized as an equivalence study in which the null hypothesis to be rejected was that of variation in pain after a half-day of rehabilitation . The number of participants was preliminarily calculated. The maximal acceptable difference in pain was 10 mm on the VAS. Equivalence was admitted if a 95% confidence interval (CI 95%) of the after/before difference was located in an interval of ±10, which corresponds to the initial postulate of delta = 10 and alpha risk = (1 − 0.95)/2, that is to say 0.025. For pain variance at 192 defined by a first group of 20 chronic low back pain patients and a beta risk of 20% conferring 80% power to the study, the number of patients to include was 40. In order to reach this objective, the inclusion period lasted for 8 months and proceeded at a rhythm of five patients a month. Under these conditions, the null hypothesis of a before/after difference equal to or above 10 mm was rejected, and the alternative hypothesis of absence of difference was accepted with a value of P < 0.025.
The second hypothesis being that since gradual weekly intensification of the program was the main factor liable to modify tolerance towards functional restoration, the pain differences after and before half-days of rehabilitation were expressed and analyzed as per-week means. Since the exercises scheduled for the morning were not identical to those planned for the afternoon, the distinction was maintained.
The differences in degree of recourse to medication during functional restoration were analyzed by comparing the treatments undergone on the first and last days of the program with a Chi 2 . A value of P < 0.05 was indicative of a significant difference between the two dates of evaluation.
Determination of the internal validity of the study was the objective of a descriptive analysis with regard to week-by-week progression during the functional restoration program and of a repeated-measures analysis of variance (ANOVA) pertaining to the efficiency criteria at 3 months. The daily loads and energy expenditures were expressed as per-week means. In the ANOVA of the efficiency criteria, a P value of < 0.05 was considered significant.
1.3
Results
Thirty-seven patients were included over a predefined period of eight months ( Table 1 ). Among the 14 preliminarily operated patients, 11 had undergone a discectomy; while three had had arthrodesis. All of the included patients actively participated in the functional restoration program. Gradual progress in terms of muscle strengthening, handling of objects and aerobic activities was documented from a sample consisting in ten of the patients ( Fig. 1 ) while the other evaluations involved the entirety of the population in the study. The numerical difference between total number of participants and number of participants analyzed is largely due to missing data and to the repeated-measures ANOVA pertaining to the efficiency criteria. Outcomes after functional restoration were characterized by markedly improved functional (Roland-Morris and Quebec scores) and quality-of-life (Dallas) indexes ( Table 2 ). Pain did not vary. Thirty-three out of thirty-six patients (91%) declared themselves improved (overall improvement: Yes) at the end of treatment. The proportion had been 25 out of 36 (69%) at 1 month and 20 out of 32 (62%) at 3 months. While 32 out of 37 patients (86%) were on sick leave prior to their participation in the functional restoration program, only seven out of 36 (19%) and five out of 32 (16%) were still on sick leave at respectively 1 month and 3 months.
| Number of patients | 37 |
| Age (standard deviation), years | 41.1 (1.4) |
| Female/male ratio, n | 15/22 |
| Pain duration (standard deviation), years | 5.6 (1.3) |
| Spinal surgery, n | 14 |
| Sick leave, n | 35 |
| Sick leave duration (standard duration), months | 13 (11.2) |

| Criteria | n | Before | After | 1 month | 3 months | P value |
|---|---|---|---|---|---|---|
| Pain | 32 | 46.1 (19.2) | 37.9 (23.2) | 40.0 (23.8) | 39.6 (23.3) | 0.1672 |
| EIFEL | 31 | 11.4 (4.4) | 6.7 (6.3) | 7.5 (7.3) | 8.3 (6.4) | < 0.0001 |
| Quebec | 30 | 35.6 (13.2) | 24.9 (16.8) | 24.8 (19.2) | 30.7 (19) | < 0.0001 |
| Dallas DA | 30 | 60.8 (12.5) | 49.0 (19.8) | 45.8 (25.5) | 53.7 (23.3) | 0.0008 |
| Dallas PL | 29 | 65.5 (15.4) | 48.8 (20.9) | 51.6 (22.6) | 53.1 (24.8) | < 0.0001 |
| Dallas AD | 31 | 36.4 (21.9) | 26.6 (22.4) | 25.3 (26.7) | 34 (25) | 0.0052 |
| Dallas S | 30 | 28.7 (23.6) | 20.5 (22.8) | 19.7 (26.1) | 22.7 (25.3) | 0.0131 |
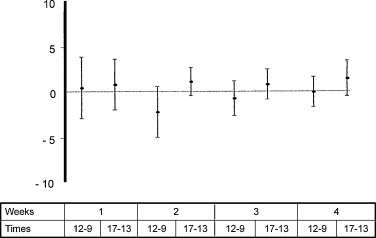
Whatever the week taken into account, pain did not vary before and after each half-day of functional restoration. The differences and their CI 95% remained within the equivalence interval of ±5 mm and all values in the confidence intervals for differences before/after half day of functional restoration contained zero ( Fig. 2 ).
The medication taken changed between the first day and the last day of the functional restoration program ( Table 3 ). The patients taking analgesics (mostly Level II) or anti-depressors were more numerous at the end of rehabilitation. The number of patients under anxiolytic treatment did not change.
| Medication | Day of evaluation | P value | ||||
|---|---|---|---|---|---|---|
| D1 | D7 | D12 | D17 | D20 | D0 versus D 20 | |
| Analgesics (level I) | 5/36 | 7/37 | 7/36 | 7/36 | 6/36 | 0.003 |
| Analgesics (level II) | 21/36 | 27/37 | 25/36 | 25/36 | 26/36 | |
| Anxiolytics | 14/37 | 18/37 | 14/36 | 14/36 | 16/36 | 0.223 |
| Anti-depressors | 10/37 | 12/37 | 13/36 | 14/36 | 13/36 | < 0.0001 |
1.4
Discussion
Our results indicate that active participation in a functional restoration program for chronic low back pain does not induce supplementary pain while it is proceeding, and that satisfactory tolerance can be at least partially explained by modified medication intake over the course of rehabilitation. The observed changes in medical treatment include recourse to analgesics (mostly Level II) and anti-depressors.
The pain induced by functional restoration for chronic low back pain had not previously been explored. No study had been designed with this objective specifically in mind. The existing data on tolerance with regard to functional restoration for chronic low back pain were drawn from clinical trials aimed at assessing the effectiveness of particular programs, and they remained fragmentary. In the relevant work, withdrawals from an ongoing study were estimated at 1 to 13% . The frequency of withdrawals attributed to recurring pain ranged from 2 to 6% . A longitudinal study described stable pain evaluated on the VAS during weekly monitoring of a four-week functional restoration program . As for our results, since they are based on information on pain gathered four times a day and on analysis of its variation throughout a rehabilitation program, they can hardly be compared with previously compiled data. That said, they are clearly in agreement with regularly reported satisfactory tolerance of functional restoration in chronic low back pain patients suffering from a severe disability .
Aside from this overall coherence, our results are further strengthened by the characteristics intrinsic to our study: scheduling, a schema in conformity with the alternative hypothesis of absent difference, precise determination of number of participants, prospective nature, internal validity control and monitoring. Internal validity is essential to an equivalence study such as ours ; it guarantees that the demonstrated lack of variation or difference is not due simply to lack of follow-up or poor effectiveness of the treatment(s) having been tested. In our study, all of the included patients actively participated, and adherence to the principle of week-by-week intensification was verified with a sample. Use of the sample so as to verify upwards progression appeared sufficient on account of the fact that program effectiveness, another internal validity criterion applicable to the study, was likewise evaluated, and the assessment covered the population in its entirety. The effects of our program were documented at 3 months in terms of functional limitations, quality of life, overall improvement and professional activity. The non-diminution of pain that we noted at the end of the program, at 1 month and at 3 months is in accordance with other observations .
As for non-recurrence of pain over the course of functional restoration, it may be due to an absence of nociceptive stimulation. The physical component of functional restoration might consequently be considered as a painless active principle. However, our weekly medication monitoring tends to lend credence to another perspective. The stability of pain throughout the program could be connected with the accompanying medication. In fact, medical treatment was modulated during the program according to the intensity of pain described in the four phases of evaluation and at any time in the diurnal cycle, particularly at the end of the day or in the night. As regards anxiolytics and anti-depressants, any decision to use them was dictated not only by pain and its neuropathic component, but also by the presence of states of anxiety and thymic depression with its different forms of clinical expression. We observed a heightened number of patients taking Level II analgesics and anti-depressors. This development was particularly pronounced at the end of the first week, and may have corresponded to the adjustment of previously insufficient treatments for painful and emotionally trying states. Given the nature of the analgesics and their rapidly active effects, they appear to have decisively contributed to pain stability throughout the program. That said, the anti-depressors at the end of the program may also have had an effect, as is suggested by the improvement of the anxiety–depression aspect of the Dallas score. In addition, our data show no modification in the number of patients taking anxiolytics, but this observation should be interpreted with caution insofar as it does not exclude a possible variation in anxiolytic dosage over the course of treatment; as a result, this parameter has not been taken into account. In any event, these different observations all demonstrate the need for rigorous medical supervision of chronic low back patients throughout the functional restoration program, and such supervision is indeed an integral part of overall patient management.
As for limits to our work, several points may be discussed. The 10 mm equivalence interval determining the sensitivity of our study does not necessarily exclude a difference in pain of lesser amplitude, and the clinical pertinence of such a variation is a question that should be raised. However, observation of our results indicates that the choice of a 5 mm equivalence interval would have led to the same conclusions. It would have included all the differences we observed along with their CI 95%. In our study, we analyzed possible variations in pain after a half-day of rehabilitation, but we did not do so following each physical exercise session, in which case repeated and constraining measurement procedures would have been required, and a major drawback would have consisted in not being able to use as a reference the initial state of rest. Our half-days of rehabilitation, on the other hand, were separated by a sufficiently lengthy time interval, namely the night or the lunch hour. The physical exercise sessions took place one after the other during the half-days, with breaks of at most a few minutes that hardly lent themselves to recovery of an initial stable or reposed state. As for the final limit to our study, it pertains to its external validity. Even though our inclusion criteria are by and large representative of those generally used in functional restoration for chronic low back pain, we need to take into account the fact that while our patients were suffering long-term pain and in 35 cases had been on sick leave for over a year, their initial VAS and Quebec scores were moderate. Our results would benefit from verification with regard to other populations.
1.5
Conclusion
We have confirmed the major interest of functional restoration in indications of disabling chronic low back pain. With our original data and given the limits of our observation conditions, we have shown that functional restoration is effective, and that as long as the physical program involves rigorous medical supervision, it does not entail recurrent or induced lumbar pain. This message could be of particular interest to potential functional restoration candidates whose fears as to the feasibility of this type of management are less well-founded than they are perhaps inclined to believe.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
La douleur induite est une réalité souvent méconnue dans nos pratiques . Elle peut être définie comme l’augmentation ou le déclenchement d’une douleur au cours d’un acte à visée diagnostique ou thérapeutique. Les données la concernant dans le cadre des programmes de restauration fonctionnelle pour lombalgie chronique sont extrêmement parcellaires . Même si le principe de restauration fonctionnelle pour lombalgie chronique repose sur un argumentaire solide allant de la cohérence de la proposition thérapeutique à la démonstration d’efficacité en termes fonctionnel et professionnel, le questionnement à propos de la douleur induite dans ce contexte paraît légitime . L’expérience montre qu’il intéresse non seulement le clinicien mais également les patients se voyant proposer une telle prise en charge. L’exploration de la douleur induite paraît en ce sens utile. Ses résultats pourraient contribuer à l’amélioration de l’acceptation par les patients candidats à la restauration fonctionnelle pour lombalgie chronique ainsi qu’à l’optimisation des programmes eux-mêmes.
À ce jour et à notre connaissance, aucune étude n’a été élaborée et conduite dans le but d’évaluer la tolérance et a fortiori la douleur induite au cours des programmes de restauration fonctionnelle pour lombalgie chronique. Ces dimensions ne sont pour l’instant appréhendables qu’indirectement, à partir du nombre de sorties d’études global, du nombre de sorties d’étude pour recrudescence douloureuse et, dans une étude d’efficacité, à partir d’une mesure hebdomadaire de la douleur en cours de programme . Cet état de fait nous a conduit à réaliser un travail prospectif ayant pour objectif principal prédéterminé l’étude de la variation de la douleur, en l’occurrence lombaire, en cours de restauration fonctionnelle pour lombalgie chronique. Afin d’apporter les garanties de la fiabilité des conditions d’observation et en conséquences celles de la validité interne de l’étude, ce travail a pris en compte la progression effective au cours du programme de restauration fonctionnelle et l’efficacité à court terme de ce dernier . Dans une perspective explicative, la médication au cours du programme de restauration fonctionnelle a également été évaluée.
2.2
Patients et méthodes
2.2.1
Inclusion
Les patients lombalgiques chroniques pris en charge dans le centre en restauration fonctionnelle ont été inclus de façon prospective. Les critères d’inclusion étaient les suivants : âge supérieur à 17 ans et inférieur à 66 ans, lombalgie commune depuis au moins trois mois, compréhension du français parlé et écrit, adhésion au projet thérapeutique, signature du consentement éclairé à la participation.
La lombalgie pouvait être associée à une radiculalgie pour peu que l’intensité de celle-ci ne fût pas supérieure à celle de la lombalgie. La lombalgie pouvait être associée à la présence de discopathie, hernie discale ou arthrose inter-apophysaire postérieure. Les patients pouvaient avoir été opérés (discectomie, laminectomie, arthrodèse) mais ce depuis au moins six mois. Ils étaient recrutés via les consultations hospitalières de médecine physique et réadaptation, rhumatologie et chirurgie orthopédique ainsi que via les consultations de villes.
2.2.2
Programme
Le programme de restauration fonctionnelle était réalisé en centre de rééducation, en hospitalisation complète, cinq jours par semaine pendant quatre semaines, en groupe de trois à cinq patients. Il comprenait l’intervention d’un médecin de médecine physique et de réadaptation, d’un psychiatre, de kinésithérapeutes, d’ergothérapeutes, d’infirmiers et d’aides soignants. Le programme d’exercices physiques comprenait : assouplissements, renforcement musculaire et activités aérobie de neuf heures à 12 heures; manutention, assouplissement, renforcement musculaire et activité aérobie de 13 heures à 17 heures. Il ne prévoyait pas l’usage de traitements antalgiques non médicamenteux.
La progression des patients en renforcement musculaire, manutention et activités aérobies se faisait par paliers hebdomadaires prédéterminés. Les critères de cette progression étaient le nombre d’exercices par série et la charge pour le renforcement musculaire et la manutention, ainsi que la puissance développée et la durée pour les activités aérobie.
2.2.3
Évaluation
Les patients inclus ont été évalués avant, pendant et après le programme de restauration fonctionnelle, à un mois et à trois mois.
La douleur lombaire en cours de programme a été évaluée sur une échelle visuelle analogique (EVA) de 0 à 100. Ce critère a été renseigné quatre fois par jour, soit avant et après la matinée de rééducation, à neuf heures et à 12 heures, ainsi qu’avant et après l’après midi de rééducation, à 13 heures et à 17 heures, chaque jour. La médication a été évaluée les premier, septième, douzième, dix-septième et vingtième jours du programme de restauration fonctionnelle. À chacun de ces temps d’évaluation, les prises d’antalgique de niveau I, d’antalgique de niveau II, d’anxiolytique et d’antidépresseur ont été notées. La prescription des myorelaxants, peu répandue dans notre pratique, n’a pas été évaluée. Le médecin en charge de la médication au cours du programme n’était pas informé des modalités de l’études.
Pour la validité interne de l’étude, les critères de progression hebdomadaire effective au cours du programme de restauration fonctionnelle étaient la charge quotidienne mobilisée en kg pendant le renforcement musculaire et la manipulation, ainsi que l’énergie quotidienne dépensée en kJ pendant les activités aérobie . L’énergie dépensée a été calculée à partir de la puissance développée et du temps passé sur bicyclette ergonomique chaque jour. Les critères d’efficacité du programme de restauration fonctionnelle étaient la douleur évaluée sur EVA de 0 à 100, la limitation fonctionnelle évaluée par l’échelle de Roland-Morris et l’échelle de Québec , l’anxiété et la dépression évaluées par l’échelle HAD , la qualité de vie évaluée par l’échelle de Dallas , ainsi que l’amélioration globale perçue par le patient en mode binaire oui/non. Ces critères ont été renseignés avant et après restauration fonctionnelle, à un mois et à trois mois. L’activité professionnelle a été évaluée avant restauration fonctionnelle, à un mois et à trois mois.
2.2.4
Statistiques
L’analyse des résultats a été planifiée sur le mode d’une étude d’équivalence où l’hypothèse nulle à rejeter était celle d’une variation de la douleur après une demi-journée de rééducation . La taille de l’effectif a été calculée au préalable. La variation maximale acceptée pour la douleur était de 10 mm sur l’EVA. L’équivalence était admise si l’intervalle de confiance à 95 % (IC 95 %) de la différence après–avant était compris dans un intervalle ±10, ce qui correspond au postulat initial d’un delta = 10 et d’un risque alpha = (1 − 0,95)/2, soit 0,025. Pour une variance de la douleur de 192 définie à partir d’un premier groupe de 20 patients lombalgiques chroniques et un risque béta de 20 % conférant à l’étude une puissance de 80 %, le nombre de patients à inclure était de 40. La durée de la période d’inclusion a ainsi été définie à huit mois afin de satisfaire à cet objectif, au rythme de cinq patients par mois. Dans ces conditions, l’hypothèse nulle d’une variation après–avant d’au moins 10 mm était rejetée et l’hypothèse alternative d’une absence de variation retenue avec une valeur de p < 0,025.
La seconde hypothèse étant que l’intensité du programme augmentant par palier hebdomadaire était le facteur principal susceptible de modifier la tolérance à la restauration fonctionnelle, les différences de douleur après–avant demi-journées de rééducation ont été exprimées et analysées en moyennes par semaine. La nature des exercices n’étant pas totalement identique en matinée et en après midi au cours du programme, cette distinction a été préservée.
La variation de recours à la médication lors de la restauration fonctionnelle a été analysée par comparaison des traitements pris le premier jour et le dernier jour du programme, à l’aide du test du Chi 2 . Une valeur de p < 0,05 attestait d’une différence significative entre les deux temps d’évaluation.
La validité interne de l’étude a fait l’objet d’une analyse descriptive concernant la progression hebdomadaire effective au cours du programme de restauration fonctionnelle et d’une analyse de variance (Anova) sur mesures répétées pour les critères d’efficacité à trois mois. Les charges et la dépense d’énergie quotidiennes ont été exprimées en moyennes par semaine. Pour l’analyse de variance des critères d’efficacité, la valeur de p considérée comme significative était < 0,05.
2.3
Résultats
Trente-sept patients ont été inclus sur la période prédéfinie de huit mois ( Tableau 1 ). Parmi les 14 patients préalablement opérés, 11 avaient eu une discectomie et trois avaient eu une arthrodèse. Tous les patients inclus ont suivi le programme de restauration fonctionnelle. La progression effective en renforcement musculaire, manutention et activités aérobie a été documentée à partir d’un échantillon de dix d’entre eux ( Fig. 1 ). Les autres évaluations ont intéressé l’ensemble de la population d’étude. Les écarts entre l’effectif total et l’effectif analysé sont liés aux données manquantes et à l’analyse en Anova pour mesures répétées des critères d’efficacité. L’évolution après restauration fonctionnelle était marquée par une amélioration des indices fonctionnels (scores de Roland-Morris et de Quebec) et de qualité de vie (scores de Dallas) ( Tableau 2 ). La douleur ne variait pas. Trente-trois patients sur trente-six (92 %) se déclaraient améliorés (amélioration globale oui) en fin de traitement. Cette proportion était de 25 sur 36 (69 %) à un mois et de 20 sur 32 (62 %) à trois mois. Alors que 32 patients sur 37 (86 %) étaient en arrêt de travail avant le programme de restauration fonctionnelle, seulement sept sur 36 (19 %) et cinq sur 32 (16 %) gardaient ce statut à un mois et trois mois.







