Fig. 8.1
The flexion axis of the fingers is perpendicular in extension and becomes oblique in flexion, which leads to an automatic rotation allowing the opposition between the thumb and the fingers (according to Kapandji)
This automatic rotation is anatomically related to the asymmetry of the joint surface and a differential tensioning of the collateral ligaments.
The amplitude of the interphalangeals in flexion is approximately 90° (depending on the person). This amplitude increases from the 2nd finger to the 5th finger.
There is 0° of extension, even though there can be tendencies to the recurvatum in the most lax patients.
The stability of the joint is related to various anatomical elements [3, 4]:
The collateral ligaments, spreading from the head of the 1st phalanx to the base of the 2nd phalanx, the volar plate and the flexor sheath. The principal fascicle is tensed between the head of the 1st phalanx and the base of the 2nd phalanx, with an insertion on the volar plate. The accessory fascicle is tensed from the head of the 1st phalanx to the volar plate and the flexor sheath. The collateral ligaments are tensed in extension (maximal tension in the accessory fascicle) and in complete flexion (phalangeal pulley wider frontwards than backwards). They are relatively relaxed in an intermediary position (Fig. 8.2) [5].
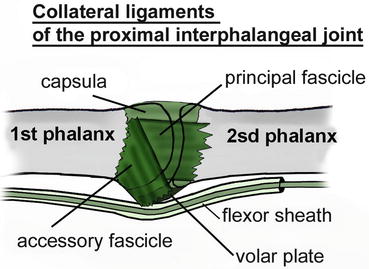
Fig. 8.2
Collateral ligaments of the proximal interphalangeal joint
The volar plate is a very resistant fibrocartilage, anchored between the 1st and 2nd phalanges on the palmar side by the “check reins”, which also are the insertion of the A3 pulley and flank the flexor sheath (Fig. 8.3). It’s tensed in extension and slides on the anterior side of the 1st phalanx in flexion (hinge system) to avoid its early abutment on the anterior side of the head of the 1st phalanx (Fig. 8.4).
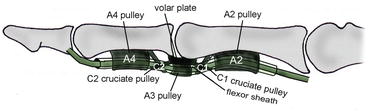
Fig. 8.3
Volar plate
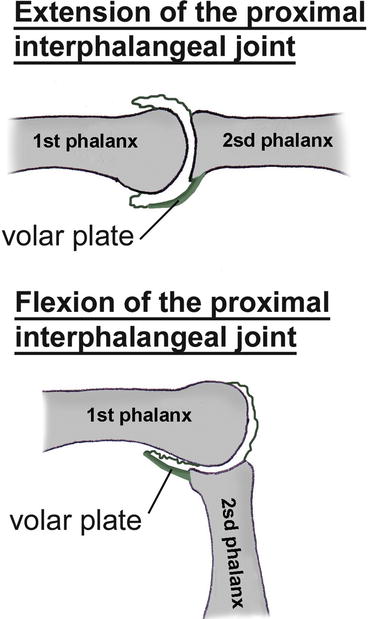
Fig. 8.4
Deployed in extension (tensioning position), the volar plate slides along the 1st phalanx during the flexion of the proximal interphalangeal joint, allowing a wider angular area
8.2 Volar Plate Sprains (Fig. 8.5) [6]

Fig. 8.5
Rehabilitation protocol of the volar plate sprains
8.2.1 Rehabilitation [7]
Volar plate injuries occur during a trauma in hyperextension (Fig. 8.6).
Fig. 8.6
Traumatism in hyperextension leading to volar plate injuries
The clinical signs are an important periarticular oedema, associated to an anterior hematoma and pain when palpating the anterior part of the joint [8].
The radiographies can highlight the presence of a little osseous fragment, corresponding to a tearing of the volar plate.
If the observed fragment is voluminous, its surgical reinsertion will be realized.
If not, the treatment is orthotic, combined with an early or immediate mobilization depending on the pain and trophic disorders. The immobilization mustn’t last longer than 48 h.
During the first 3 weeks, the orthotic treatment consists in realizing a “proximal interphalangeal stop” orthosis, placing the interphalangeal in extension. It will be worn during the night, while a syndactyly is worn during the day (Fig. 8.7).


Fig. 8.7
The “proximal interphalangeal stop” in extension is worn during the night (a). Diurnal syndactyly liberating the flexion creases of the proximal interphalangeal to maintain mobility (b)
The rehabilitation must be realized early and with very soft and progressive techniques in order not to “attack” the damaged tissues. As Madden reminds us, “tissues don’t know enthusiasm, but stress”.
8.2.1.1 Acute Phase (D0 to D21)
Fight Against Pain and Trophic Disorders
Draining massages from distal to proximal, following the neurovascular pedicles.
Electrotherapy: 1 Hz on the oedematous area or 100 Hz for a precise analgesic effect.
Gaseous cryotherapy allowing a very precise anti-oedematous effect on the interphalangeal joint (Fig. 8.8). Cryotherapy also has an interesting analgesic effect.

Fig. 8.8
Gaseous cryotherapy in front of the proximal interphalangeal joint, controlling the cutaneous temperature with an infrared thermometer
Pressotherapy: the device realizes a compression from distal to proximal that drains the hand oedema. A soft painless posture in extension can be realized during the treatment. In this phase, this technique can be badly tolerated by the patient, in which case we delay its application.
Compressive bandage during the night if the oedema is important and resistant to treatment (Fig. 8.9).

Fig. 8.9
Compressive bandage in case of important oedema
Put the hand in an elevated position at home, especially when there’s a global oedema of the hand (rare case).
Transcutaneous vibratory stimulations (frequency 50–100 Hz, amplitude >1 mm) are applied on the painful area, moving along the sensitive nerve concerned by the painful area. If there is pain when contacting with the device, we place it away from the painful area, still on the corresponding nerve. This type of mechanical vibration has a sensorimotor stimulation effect, limiting the risks of functional exclusion.
Progressive Recuperation of the Joint Amplitudes
Passive mobilizations in flexion and active mobilizations in extension, then active in flexion/extension. The soft passive mobilizations in flexion relax the joint, before asking the patient to do an active exercise, which can easily lead to pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








