Capitellum and Trochlea Fractures
David Ring
Jesse B. Jupiter
INTRODUCTION
Recent studies confirm that apparent capitellum fractures frequently involve the anterior trochlea (termed coronal shear) and often involve impaction of the posterior lateral column and the posterior and medial trochlea (1,2,3,4,5,6,7 and 8). In other words, they are often complex articular fractures of the articular surface without fracture of the columns of the distal humerus.
These fractures can be challenging to repair by virtue of (a) small entirely articular fragments, (b) limited subchondral bone, (c) small-sized fragments, (d) multiple fragments, and (e) little or no unfractured humerus to which the fracture fragments can be repaired. Involvement of the posterior humerus (posterior lateral column behind the trochlea and the posterior trochlea) has been associated with a substantial risk of nonunion (2). In our opinion, this is related to avascular necrosis with a greater risk for infection (2,3,6).
The most complex fractures may be considered for hemiarthroplasty (prosthetic replacement of the distal humeral articular surface) in older or more infirm patients with lower functional demands because the columns and the medial collateral ligament are usually intact. Total elbow arthroplasty is also an option in low-demand or infirm patients, as is nonoperative treatment or the so-called “bag of bones” technique.
PREOPERATIVE PLANNING
History and Physical Examination
Fracture of the capitellum and trochlea can occur as a fracture dislocation, so patients should be asked about any potential self-reduction or reduction by a health care provider. Complex fractures typically involve fracture of the lateral epicondyle, but fracture dislocations will also have a medial collateral ligament avulsion from the medial epicondyle (1,2).
Ulnar neuropathy is sometimes diagnosed during the recovery process, so it is worthwhile to carefully examine and document nerve function at the time of injury.
The patient’s functional demands and overall health will influence treatment as much as the fracture pattern and complexity. Circumstances such as lower limb injuries and the need for weightbearing through the upper limb for ambulation might also be important.
Imaging Studies
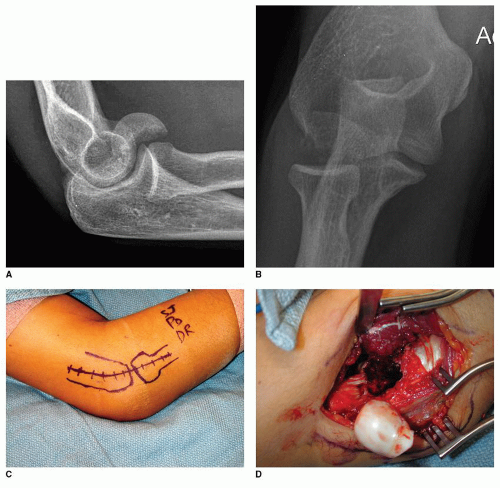
Computed tomography (CT) provides useful information, particularly for more complex fractures. We find 3D reconstructions more intuitive, and there is some evidence that they can improve the reliability of diagnosis of certain fracture characteristics (9) (Fig. 9-1). It is helpful to be prepared for the size and extent of the trochlea fracture (involvement of the posterior or medial trochlea in particular) and any fracture of impaction of the posterior aspect of the lateral column (Fig. 9-1B and C). The extent of fragmentation can also help with planning of either fixation techniques or the decision to use a prosthesis. One thing to look for carefully is stable impacted fracture fragments (Fig. 9-1B). These fragments are out of position but may not appear fractured in surgery because they are not easily moved and the fracture lines are not obvious (analogous to plastic deformation in children). It may not be possible to fully reduce all the fracture fragments until these fragments are realigned.
Timing of Surgery
It is more important that a surgeon who is familiar with these fractures treats the patient with adequate preparation (e.g., CT scan) and appropriate equipment available than it is to do the surgery soon after injury. A delay of up to 2 weeks to get all of this organized is reasonable. The exception is the rare open fracture. It is difficult to stage the treatment of open fractures because some of the important articular fragments are completely devitalized and benefit debridement, irrigation, and repair at the time of open fracture treatment to limit colonization and the potential for infection.
SURGERY
Positioning/Surgical Approaches
The majority of capitellum/trochlea fractures can be treated through an extended lateral exposure, which is easiest with the patient supine and arm supported on a hand table (Figs. 9-2, 9-3 and 9-4). When
there is involvement of the posterior or medial part of the trochlea, an olecranon osteotomy provides better access and visualization (Fig. 9-5).
there is involvement of the posterior or medial part of the trochlea, an olecranon osteotomy provides better access and visualization (Fig. 9-5).
For simple fractures, a lateral skin incision is sufficient (Fig. 9-2C). For more complex fractures, a posterior skin incision allows the surgeon to convert to an olecranon osteotomy when necessary (Fig. 9-3A




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree