Fractures of the capitellum
Bryan et al. (1985)
Coronal shear fractures
McKee et al. [2]
Articular fractures of the distal humerus
Ring et al. [3]
Predominantly articular fractures
Davies et al. [6]
Capitellar and trochlea fractures
Dubberley et al. [5]
Apparent capitellar fractures
Ring [4]
Initially they were defined as “isolated fractures of the capitellum” and were classified according to Broberg and Morrey in three types [1]: Type I fracture, also called “Hahn-Steinthal fractures,” that consists of a single and large hemispherical osseous fragment involving the entire capitellum with a good subchondral bone, Type II also called “Kocher-Lorenz” which consists of an osteochondral fracture with minimal subchondral bone, and Type III consisting of a comminuted or compression fracture of the capitellum (Fig. 23.1).
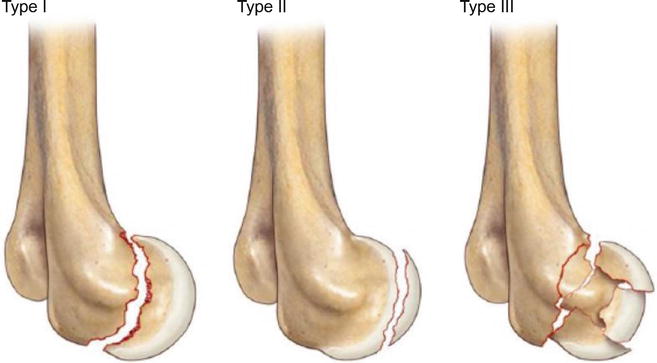
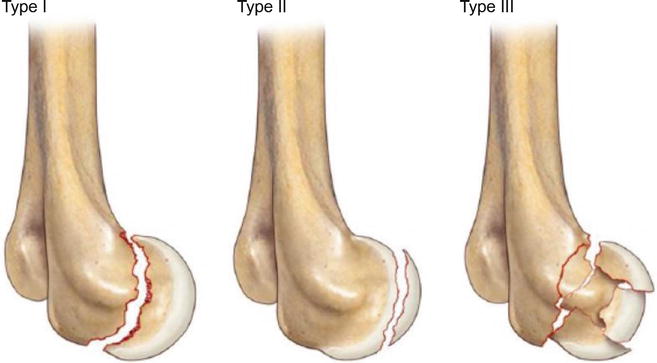
Fig. 23.1
Classification of capitellar fractures according to Broberg and Morrey in three types [1]: Type I, single and large hemispherical osseous fragment involving the entire capitellum with a good subchondral bone. Type II, osteochondral fracture with minimal subchondral bone. Type III, comminuted or compression fracture of the capitellum
Afterward, as also the trochlea was sometimes involved, a fourth type was added to the previous classification [2] and named “coronal shear fractures.”
Some years later Ring [3] defined generically all these types of fractures “articular fractures of the distal humerus.” He noted in fact that these lesions are often not only coronal shear fractures of the capitellum and the trochlea, but they more frequently involve or extend to the lateral epicondyle, the lateral column, the posterior part of the trochlea, and the medial epicondyle, as well as in a subsequent progression of severity caused by the energy and the mechanism of trauma.
To emphasize the important concept that isolated capitellar fractures, as seen on plain X-rays, are uncommon, and very often they present an involvement of the lateral portion of the trochlea at least, Ring proposed the name of “apparent capitellar fracture” [4].
Later Dubberley proposed the name of “capitellar and trochlea fractures” [5] and a new classification system based on the extension of the fracture on the coronal plane, the presence of fragmentation, and posterior comminution as prognostic factors (Figs. 23.2 and 23.3).
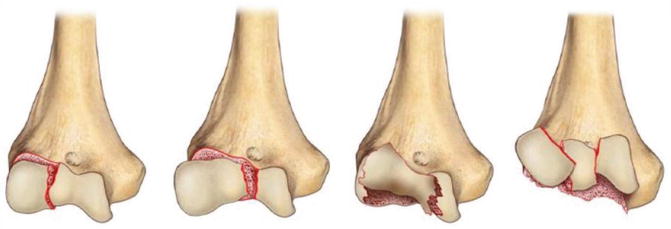
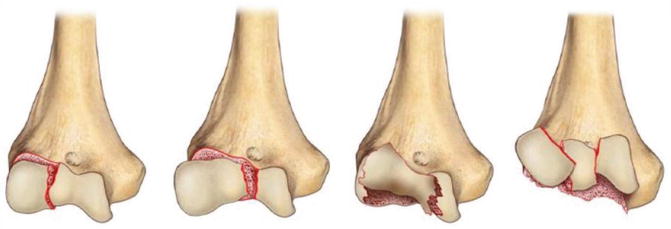
Fig. 23.2
Dubberley proposed the name of “capitellar and trochlea fractures” [5] and a new classification system based on the extension of the fracture on the coronal plane, the presence of fragmentation 78, and posterior comminution as prognostic factors
Fig. 23.3
Conservative treatment of displaced capitellar and trochlear fractures leads invariably to poor results. Clinical case: (a, b) Pre-operative CT Scan, (c, d) clinical result with flexion and extension limitation
The Dubberley and AO/ASIF classifications are currently widely accepted.
According to the AO/ASIF classification, these fractures are grouped as 13 – B3 (distal part of the humerus, partial articular, on the frontal plane), with B3.1 indicating capitellar fractures, B3.2 trochlear fractures, and B3.3 capitellar and trochlear fractures [7].
Recent evidences support the idea that isolated fractures of the capitellum are rare: a portion of the trochlea (the lateral) is involved in almost 80 % of the cases [3, 5, 8, 9]. Lateral collateral ligament injuries are associated up to 40 % of cases, and radial head fracture is reported from 10 to 30 % of cases [5, 10].
23.3 History and Physical Examination
If an athlete presents with elbow pain, joint effusion, and flexion impairment after a direct or indirect trauma, a thorough investigation is mandatory to exclude an articular fracture.
On plain X-ray, mostly in the anteroposterior views, these types of fracture can be difficult to identify. Capitellar fractures extending to the trochlea may be detected by a pathognomonic radiographic feature visible on the lateral view and called “double-arc sign.” It is formed by the subchondral bone of the capitellum and the lateral trochlear ridge, typically rotated and displaced in a proximal direction.
CT scan is essential for a correct comprehension of the fracture pattern and thus for the surgical planning. It allows to correctly identify the degree of involvement of the capitellum and the trochlea, the columns, the posterior trochlea, and also the presence of posterior impaction or comminution which affect surgical fixation, rehabilitation, and prognosis. Moreover CT scan can clearly show possible associated lesions, like radial head or proximal ulnar fractures.
23.4 Treatment Options (Evidence Based)
Several methods have been described for the treatment of capitellum and trochlea fracture, including conservative treatment, simple excision, open reduction and internal fixation (ORIF), arthroscopic reduction and internal fixation (ARIF), and elbow replacement (total elbow arthroplasty or distal humeral hemiarthroplasty).
Nowadays it is well known that conservative treatment of displaced capitellar and trochlear fractures leads invariably to poor results (Fig. 23.4).
Fig. 23.4
Fractures involving the capitellum and a small part of the trochlea (Type 1 of Dubberley classification) can be treated through a Kocher approach preserving the lateral collateral ligament (a). With greater involvement of the trochlea, with or without fragmentation (Type 2 and 3 of Dubberley classification), the extensile posterolateral approach described by Morrey is necessary (b). When the posterior trochlea and the medial epicondyle are involved, a trans-olecranic approach is recommended (c)
If the severity of the comminution of the capitellum precludes any attempt of ORIF, fragment excision performed either with open technique or arthroscopically can be a reasonable salvage option.
In this situation it is important to remember that the capitellum does not contribute significantly to the ulnohumeral joint stability when all the other stabilizers are intact. On the contrary, the whole trochlea articular surface is necessary for a normal elbow kinematics, even when all the other stabilizers are intact [11].
However, thanks to the great improvement in surgical approaches and fixation techniques, nowadays, it is possible to perform ORIF in the majority of cases.
The first option is fixation with screws. If the fragments are too small, or the subchondral bone is not thick enough to accept one or more screws, resorbable pins can be used.
If posterior comminution is present (Dubberley/AO type B fractures), every single case should be carefully evaluated intraoperatively. It is therefore necessary to have different fixation devices available in theater, in addition to the screws, such as Kirschner wires, resorbable pins, anatomical plates, bone graft, external fixator, and prosthesis.
The prosthetic replacement, by total elbow arthroplasty or distal humerus hemiarthroplasty, is not indicated for young patients and athletes and its indications and results will not be discussed in this chapter.
23.4.1 Surgical Technique
If olecranon osteotomy is not indicated, our preferred approach is a lateral skin incision, centered over the lateral epicondyle and extended from the anterior aspect of the lateral column to approximatively 2 cm distal to the radial head.
Proximally the distal and anterior part of the lateral column is exposed, while distally the Kocher interval is developed, preserving the LUCL. With the elbow flexed, it is possible to have a good exposure of the capitellum and the lateral part of the trochlea by placing a large and blunt Hohmann retractor beneath the anterior capsule and the brachialis muscle, just over the medial column.
If a bigger part of the anterior trochlea is involved, an extensive lateral exposure with elbow subluxation is indicated. If also the posterior trochlea and/or the medial epicondyle are involved, then olecranon osteotomy is necessary.
Regardless of the chosen approach, the articular fragments are carefully reduced and temporarily fixed with Kirschner wires placed along the fracture margin in order to avoid interference with subsequent placement of the screws; if the fragments don’t reduce, the posteroinferior aspects of the distal lateral column and trochlea should be inspected for impaction and comminution. Definitive fixation of the capitellar and trochlear fragments is then achieved with screws, ideally at least two with divergent directions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








