The atlantoaxial motion segment, which is responsible for half of the rotational motion in the cervical spine, is a complex junction of the first (C1) and second (C2) cervical vertebrae. Destabilization of this joint is multifactorial and can lead to pathologic motion with neurologic sequelae. Posterior spinal fixation of the C1-C2 articulation in the presence of instability has been well described in the literature. Early reports of interspinous/interlaminar wiring have evolved into modern-day pedicle screw/translaminar constructs, with excellent results. The success of a C1-C2 posterior fusion rests on appropriate indications and surgical techniques.
The atlantoaxial motion segment is a complex junction of the first and second cervical vertebrae that is responsible for half of the rotational motion in the cervical spine. Destabilization of this joint is multifactorial and can lead to pathologic motion with neurologic sequelae. Static stability is conferred by both osseous and ligamentous contributions consisting primarily of the facet articulations, dens and fovea dentis, the facet capsule, and the transverse atlantal ligament. Dynamic stability arises from the multiple muscular attachments of the anterior arch and transverse process. Trauma, congenital malformation, inflammatory arthritides, and malignancy have all been implicated in the development of atlantoaxial instability. Since the first description of surgical treatment by Mixter and Osgood in 1910, multiple techniques have been described to provide atlantoaxial stability in an effort to protect the space available for the spinal cord and prevent basilar invagination.
Anatomic considerations
The first cervical vertebra (C1) consists of an anterior arch, a posterior arch, and two lateral masses, giving it a ringlike structure. The anterior tubercle on the anterior arch serves as an attachment site for the longus colli muscle; posteriorly, the fovea dentis serves as the articulation point for the odontoid process of the second cervical vertebra (C2). The posterior arch provides a smooth edge for the attachment of the posterior atlanto-occipital membrane. The sulcus arteriae vertebralis is present behind each superior articular process and represents the superior vertebral notch. The vertebral artery and the first spinal nerve reside within this sulcus. The undersurface of the posterior arch provides an attachment surface for the posterior atlantoaxial ligament. The lateral masses of C1 have an inferior and a superior articular facet; the superior facet surface forms a cuplike articulating surface for the corresponding condyle of the occiput. The inferior articular facet surfaces articulate with C2 and permit rotation of the head. Anteriorly, at the level of the superior facet the important transverse atlantal ligament traverses the C1 ring, dividing the vertebral foramen into an anterior part, which contains the dens, and a posterior part, which encases the spinal cord. On occasion, the sulcus for the vertebral artery on the dorsal aspect of the atlas may be completely covered by an anomalous ossification, termed the ponticulus posticus. The resulting foramen retains the vertebral artery and is referred to as the arcuate foramen. Young and colleagues retrospectively reviewed 464 lateral radiographs of the neck and determined a prevalence of 15.5% of the presence of this anomaly. The relevance of this finding is that some surgeons have advocated the starting point of a C1 lateral mass screw to be at the dorsal aspect of the posterior arch instead of the base of the lateral mass. The presence of an unidentified posticulus posticus may lead to iatrogenic injury to the vertebral artery.
The second cervical vertebra (C2) or axis forms a pivot by which the first vertebra rotates. The dens has an apex and neck at which it joins the body. An oval facet on its anterior surface allows articulation with the atlas. Posteriorly, neck of the dens is the insertion site of the transverse atlantal ligament. The apical odontoid ligament attaches along the apex, and caudally, along either side of the neck the alar ligaments attach, which connects the odontoid process to the occiput. The pedicles are covered by the superior articular surfaces that articulate with C1. The transverse processes are each perforated by the foramen transversarium via which the vertebral artery ascends at C6. After exiting the foramen of the axis, the artery courses laterally to pass through the foramen of the atlas. The vessel then courses posteromedially along the superior aspect of the atlas in the superior vertebral notch to enter the dura near the midline, before traveling through the foramen magnum to form the Circle of Willis. The left vertebral artery is dominant in 36% of patients, hypoplastic in 6%, and absent in 2%. The right is dominant in 23% of patients, hypoplastic in 9%, and absent in 3%. Equivalent right and left vertebral arteries are present in 41% of patients.
Classic Indications
Trauma
In the setting of fracture, most surgeons determine atlantoaxial stability based on the integrity of the transverse atlantal ligament. Jefferson fractures with combined lateral displacement of the C1 lateral masses on C2 of greater than 6.9 mm on an anterior-posterior radiograph of the odontoid process suggest that the transverse atlantal ligament has been torn. Results of nonoperative management of displaced fractures have been poor. There is controversy in the literature regarding appropriate surgical management. Proposed treatments include halo brace immobilization, traction, atlantoaxial fusion, and more recently, C1 ring osteosynthesis. Regardless of treatment method, postoperative radiographic assessment of stability is indicated.
Odontoid fractures represent 5% to 15% of all cervical spine injuries. Anderson-D’alonzo Type II odontoid fractures are the most common odontoid injury, and result in atlantoaxial instability requiring stabilization. Although treatment of odontoid fractures remains controversial, atlantoaxial arthrodesis is an accepted treatment option. In addition, placement of an odontoid screw in a morbidly obese patient or a patient with significant kyphosis may not be possible from an anterior approach, necessitating a posterior approach and atlantoaxial arthrodesis.
Traumatic rupture of the transverse ligament without fracture is rare. In adult patients with intact atlantoaxial ligaments the anterior atlanto-dens interval is 3 mm with no change during flexion or extension. Fielding and colleagues demonstrated that “acute shift of the first on the second cervical vertebra under load does not exceed 3 millimeters if the transverse ligament is intact,” and that following rupture the remaining structures are unable to stop further displacement. In this setting atlantoaxial fusion is indicated to protect the space available for the spinal cord.
Rheumatoid arthritis
Rheumatoid arthritis is a chronic autoimmune mediated inflammatory disorder characterized by synovial joint pannus formation and periarticular erosions. Following the hands and feet, the cervical spine is the most common site of involvement, often within 2 years of diagnosis. Three types of instability are seen, usually in progression with advancement of disease: atlantoaxial subluxation, basilar invagination, and finally subaxial subluxation. The typical presentation is that of neck pain with positional temporal or suboccipatal radiation. Radiographic evidence of instability typically precedes neurologic symptoms. If the disease has progressed to basilar invagination or subaxial subluxation, extended fusion is indicated. Atlantoaxial arthrodesis is indicated in patients with intractable pain, progressive neurologic deficit, or myelopathy in patients with instability. Some investigators have proposed surgery before the development of neurologic symptoms if the posterior atlanto-dens interval is less than 14 mm in the setting of atlantoaxial instability. Treatment prior to the development of myelopathy has been associated with improved outcomes.
Congenital malformation
Os odontoideum represents an independent smoothly corticated ossicle of variable size, which is separated from the hypoplastic odontoid peg. The etiology of os odontoideum remains controversial, with two distinct schools of thought. The congenital origin theory hypothesizes that the segmental anomaly present results from failure of fusion between the dens and the body of the axis. The traumatic origin theory suggests that os odontoideum represents a late diagnosis of previously unrecognized odontoid type II fracture followed by avascular necrosis, nonunion, and ossicle remodeling. Presentation may vary from an incidental finding, axial neck pain, or myelopathic deficits. In a recent review, Arvin and colleagues suggest that “patients with unstable os odontoideum or those with a fixed deformity causing compression of the upper cervical/medullary junction should be offered surgery.” Ventral or dorsal approach and fixation should be predicated on the direction of neurologic compression if present, as well as surgeon experience and comfort.
Technique
Dorsal Wiring
History
The first surgical treatment of atlantoaxial instability was described by Mixter and Osgood in 1910. These investigators reported using a braided silk suture looped around the posterior arch of the atlas under the spinous process of the axis as treatment for symptomatic atlantoaxial subluxation secondary to odontoid nonunion in a 15-year-old boy, with good results at 2-year follow-up. In 1939 Gallie reported “recurrence of displacement can be guarded against by fastening the two vertebrae together by fine steel wire passed around the laminae or spines … and … bone grafts laid in the spines or on the laminae and articular facets.”
Technique
The technique of modern dorsal wiring was described by Brooks and Jenkins in 1978. After careful exposure of the spinous process and laminae of the axis and subperiosteal dissection of the posterior arch of the atlas, the opposing surfaces of the atlas and axis are prepared for bone graft. A suture is then placed on each side of the midline from proximal to distal under the arch of the atlas and subsequently under each laminae of the axis. The suture is then used as a guide to direct the looped end of two doubled 20-gauge stainless-steel wires. Two rectangular full-thickness autogenous iliac crest bone grafts are placed on either side of the midline in the prepared intralaminar space. The construct is secured by twisting the wires dorsally.
The technique of Brooks and Jenkins was modified by Dickman and colleagues such that sublaminar wires need only be placed at a single level. Using this method a loop of #24 surgical steel is passed from distal to proximal under the posterior arch of the atlas. A single rectangular bicortical iliac crest bone graft with an inferior central notch is then placed over the spinous process of the axis dorsal to the free ends of surgical steel with the concavity opposed to the dura. The loop is then pulled caudally, where it is secured in a notch created on the inferior aspect of the C2 spinous process. One of the free ends of surgical steel is passed under the spinous process of the axis similarly to the loop, and compression is obtained by twisting the free ends 3 times per centimeter so that the graft, if trapped dorsal to the free wire, ends ventral to the loop. Postoperatively all patients were placed in halo immobilization for 3 months followed by a Philadelphia collar for 4 to 6 weeks.
Results
In their classic article Brooks and Jenkins reported osseous fusion of the atlantoaxial joint in 93% of cases (13/14) who were available for follow-up. One patient died 8 weeks postoperatively of unknown cause. These results have been verified by several subsequent reports on fusion. Using the Sonntag modification of the Brooks fusion, Dickman and colleagues reported osseous fusion in 89% of patients (31/35). Of note, a disproportionately high number (3/4) of these nonunions were treated for rheumatoid arthritis.
Complications and technical considerations
Complications of dorsal intralaminar and intraspinous wiring techniques were rare. Nonunion is a well-known complication of any arthrodesis procedure, and is discussed elsewhere in this article. Iatrogenic fracture of the posterior arch during wire tensioning necessitating extension of the fusion construct was reported by Brooks. Also concerning is the risk of dural tear or neurologic injury while passing sublaminal wires. This complication was not reported in the Brooks or Sonntag articles; however, other investigators have reported this at the axis. Space available for the spinal cord decreases at more caudal levels, and the theoretical advantages of the Sonntag modification are worth considering. Although early reports of these techniques demonstrated excellent fusion results, more recent reports have suggested nonunion rates of up to 30%. Furthermore, the biomechanical superiority of the transarticular method is well documented.
Transarticular Atlantoaxial Arthrodesis
Technique
Transarticular atlantoaxial fixation was first described by Magerl and Seemann in 1987. In this technique the patient is positioned prone with the neck in neutral and the head in a tucked position. A midline dorsal incision is created to expose the posterior elements of C1 to C3 with attention to the posterior aspect of the atlantoaxial facet joint. Before fixation, reduction of subluxation is performed with positioning or manual techniques such as the Halifax interlaminar clamp. Through bilateral stab incisions a Kirschner wire is then directed down the C2 pedicle across the facet joint toward a point 3 to 4 mm posterior to the anterior tubercle of C1. A cannulated drill bit is then passed over the Kirschner wire, taking care not to inadvertently advance the wire. The pilot hole is then taped, and a solid 3.5-mm or cannulated 4.0 mm cortical screw is then placed bilaterally. Use of a Herbert compression screw has also been described. This construct is then supplemented with intralaminar iliac crest autograft and dorsal wiring using a dorsal wiring technique or interlaminar clamp. Anomalous course of the vertebral artery, comminuted fracture, or other pathologic lesions made bilateral transarticular screw placement unsuitable in 7% to 17% of patients. Given the added stability of instrumentation, halo immobilization is usually avoided except in the instance of severe osteoporosis.
Results
Reports have documented osseous fusion in 96% to 99% of cases using this technique. Improvement of neck pain, anterior atlanto-dens interval, and neurologic symptoms were findings at long-term clinical follow-up in the majority of cases.
Complications and technical considerations
While the definition of screw malposition is variable in the literature, the reported incidence is 2% to 15%. Fortunately, the incidence of vertebral artery injury is low (2.4%), with several large series reporting no vertebral artery injury. Although the safety of the procedure has been well documented, the complex anatomy at the atlantoaxial junction and technical demands of the surgical procedure should not be underestimated. Apfelbaum reported one instance of bilateral vertebral artery injury resulting in death in a series of 40 patients, Marcotte and colleagues reported two cases of dural tears in a series of 18 patients, and Coric and colleagues reported transarticular screw-induced arteriovenous fistula. Preoperative imaging is paramount in detecting an anomalous vertebral artery course that would preclude screw placement. Paramore and colleagues assessed a series of computed tomography (CT) scans for determining the safety of potential screw trajectory, and concluded that 18% to 23% of patients “may not be suitable for posterior C1-2 transarticular screw fixation on at least one side.” Complete reduction of atlantoaxial subluxation and appropriate monitoring during screw insertion further reduce the risk of inadequate screw placement. When bilateral fixation is not possible, Song and colleagues demonstrated that adequate stability could be achieved using a unilateral transarticular screw with 100% osseous union in 19 cases.
Polyaxial Screw and Rod Fixation
Technique
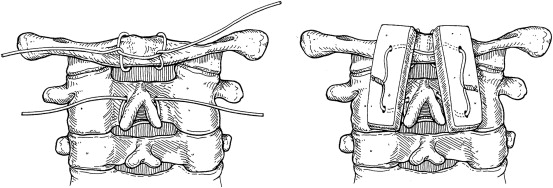
In 2001 Harms and Melcher described a novel posterior fixation method that minimized the risk of injury to the vertebral artery, and allowed intraoperative reduction and fixation of the atlantoaxial complex. A dorsal approach is used with subperiosteal dissection from the occiput to C3-C4. Exposure of the C1-C2 joint with particular attention to the superior surface of the C2 pars interarticularis is critical for placement of the C1 lateral mass screw. The C2 dorsal root ganglion is retracted caudally and straight or slightly convergent 3.5 mm C1 lateral mass screws are placed from an entry point at the middle of the junction of the C1 posterior arch and the midpoint of the posterior inferior aspect of the C1 lateral mass. C2 pedicle screws are placed from an entry point in the cranial and medial quadrant of the isthmus surface of C2 directed 20° to 30° in a convergent and cephalad direction predetermined by preoperative imaging. The C1 lateral mass screw is left proud to allow rotation of the polyaxial screw head and to prevent C2 nerve root irritation. Reduction of subluxation can be achieved under direct fluoroscopic guidance by positional techniques or manipulation of the instrumentation. Whereas Harms and Melcher recommended posterior C1 and C2 decortication and autogenous bone grafting for osseous fusion, Ni and colleagues suggested a modification such that bicortical iliac crest graft is compressed between the posterior arch of C1 and the lamina of C2 using the rod and screw construct for graft compression. The authors’ preferred fusion technique is to use a modified Gallie wiring with compression of corticocancellous allograft ( Fig. 1 ). The pedicle/lateral mass screw construct provides stability; however, the authors believe that fusion is afforded by wiring/corticocancellous compression grafting.
Results
Osseous fusion at 3 to 6 months of follow-up is reported as from 94% to 100% using the polyaxial screw and rod technique. A statistically significant improvement in postoperative neurologic status and subjectively reported neck has been reported.
Complications
Screw malposition has varied from 0% to 4% in the atlas and 0% to 7% in the axis. Four of the 28 patients presented by Stulik and colleagues suffered from paresthesias in the region innervated by the greater occipital nerve, with all but one eventually resolving. Terterov and colleagues reported symptomatic compression of the vertebral artery by the rod of a Harms-type construct. There are two reports of proximal rod migration through the base of the skull in the setting of atlantoaxial nonunion following the Harms technique.
The risk of injury to the vertebral artery during placement of screws for atlantoaxial fixation is highly associated with screw malpositioning. Unidentified anomalous course of the vertebral artery increases this risk. There have been reports of erosion on the C2 lateral mass and pars by the artery itself, and asymmetric grooving of the C2 pars. In a study by Abou Madawi and colleagues, 52% of their cadaveric specimens had an asymmetric course. Igarashi and colleagues reported that the differences of the pars width on the superior surface of C2 averaged 1.2 ± 0.9 mm, the pars width on the inferior surface averaged 1.0 ± 0.8 mm, and the pars height averaged 1.2 ± 1.0 mm.
C2 Translaminar Constructs
Leonard and Wright described a new technique for rigid screw fixation of the axis involving the insertion of polyaxial screws into the laminae of C2 in a bilateral, crossing fashion; they then incorporated these fixation points into atlantoaxial fixation or subaxial cervical constructs. This technique allows safer rigid fixation of C2, as the screws are not inserted near the vertebral artery. The caveat, however, is that unlike the transarticular or C1-C2 lateral mass/pedicles screw techniques of atlantoaxial fixation, this technique requires intact posterior elements of C2.
Technique
Patients are placed in the prone position with the head maintained in the neutral position using a head holder. The posterior arch of C1 is identified and the lateral masses are appropriately visualized. The spinous process, laminae, and medial lateral masses of C2 are then meticulously exposed. C1 lateral mass screws are placed using the Harms technique already described. The high-speed drill is used to open a small unicortical window at the C2 spinolaminar junction. Using a hand drill, the contralateral lamina is carefully drilled to a depth of 30 mm, with the drill angulated to match the contralateral laminar surface. A small ball-tipped probe is used to palpate the length of the drill hole to verify that no cortical breach into the spinal canal has occurred. A 30 mm polyaxial screw is carefully inserted along the same trajectory as the drill hole. The screw head thus sits at the spinolaminar junction on the right, with the length of the screw threads within the left lamina. Using the same technique a 30 mm screw is placed into the right lamina. After screw placement, all exposed laminar surfaces are decorticated and prepared for bone graft. The C1 lateral mass screws are connected to the C2 laminar screws with posterior rods.
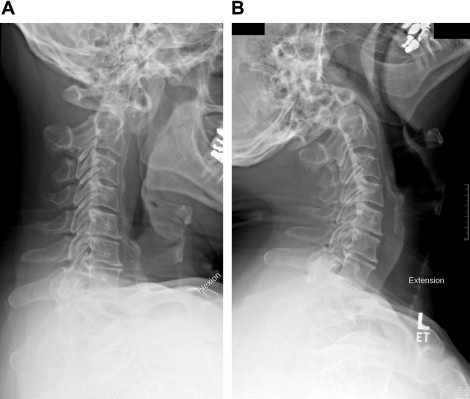
Case example
The patient is a 55-year-old man who had a long-standing history of right-sided radicular pain with axial neck pain. Plain radiographs revealed an os odontoideum and flexion-extension radiographs revealed evidence of instability of the C1-C2 articulation ( Fig. 2 ). CT scans revealed foraminal narrowing at C3-C4, C4-C5, and C5-C6. He underwent a C1-C2 posterior spinal fusion with modified Gallie wiring with structural allograft and right-sided foraminotomy of C3 to C6 ( Fig. 3 ). The patient tolerated the procedure well, and returned to follow-up ( Fig. 4 ) at 1 year with all symptoms completely resolved.