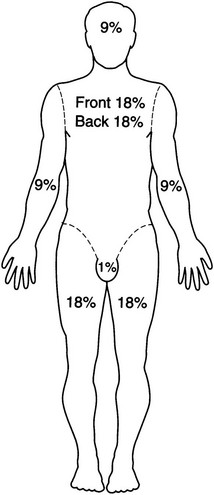
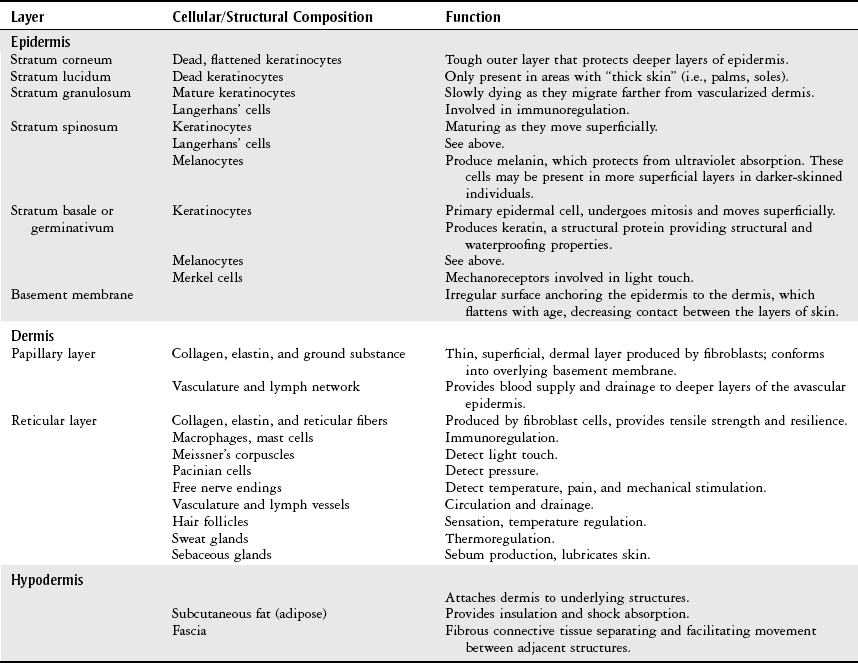
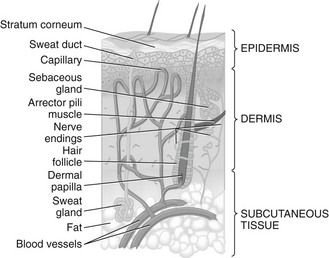
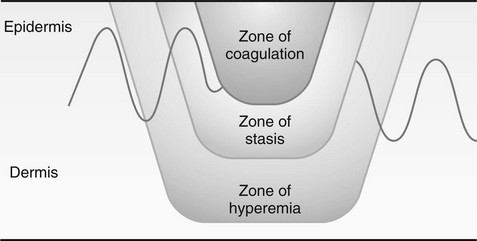
Chapter 12 Body Structure and Function: Normal Integument Burn Assessment and Acute Care Management of Burn Injury Physical Therapy Examination in Burn Care Factors That Can Delay Wound Healing Wound Assessment and Acute Care Management of Wounds The objectives of this chapter are to provide a fundamental review of the following: 1 The structure and function of the skin (integument) 2 The evaluation and physiologic sequelae of burn injury, including medical-surgical management and physical therapy intervention 3 The etiology of common types of wounds and the process of wound healing 4 The evaluation and management of wounds, including physical therapy intervention • Burns: Thermal, Electrical, Chemical, Ultraviolet, Ionizing, Radiation: 6C, 6E, 7B, 7C, 7D, 7E • Trauma Wounds: 4I, 4J, 7C, 7D, 7E • Surgical Wounds: 4I, 7A, 7C, 7D, 7E • Vascular Wounds (Arterial, Venous, Diabetic): 5G, 7A, 7B, 7C, 7D, 7E • Pressure Wounds: 7A, 7B, 7C, 7D, 7E Please refer to Appendix A for a complete list of the preferred practice patterns, as individual patient conditions are highly variable and other practice patterns may be applicable. Treating a patient with a major burn injury or other skin wound is often a specialized area of physical therapy.* All physical therapists should, however, have a basic understanding of normal and abnormal skin integrity, including the etiology of skin breakdown and the factors that influence wound healing. The integumentary system consists of the skin and its appendages (hair and hair shafts, nails, and sebaceous and sudoriferous [sweat] glands), which are located throughout the skin, as shown in Figure 12-1. Skin is 0.5 to 6.0 mm thick1,2 and is composed of two major layers: the epidermis and the dermis. These layers are supported by subcutaneous tissue and fat that connect the skin to muscle and bone. The thin, avascular epidermis is composed mainly of cells containing keratin. The epidermal cells are in different stages of maturity and degeneration and are therefore seen as five distinct layers within the epidermis. The thick, highly vascularized dermis is divided into two layers and is composed mainly of collagen and elastin. The epidermis and dermis are connected at the dermal-epidermal junction by a basement membrane. Table 12-1 reviews the cellular composition and function of each skin layer. TABLE 12-1 Normal Skin Layers: Structure and Function Data from Myers BA: Wound management: principles and practice, ed 3, Upper Saddle River, NJ, 2012, Pearson Education, p 4; Baronoski S: Integumentary anatomy: skin—the largest organ. In McCulloch JM, Kloth LC, editors: Wound healing: evidence-based management, ed 4, Philadelphia, 2010, FA Davis, p 1; Sussman C, Bates-Jensen B: Wound care: a collaborative practice manual for health professionals, ed 3, Baltimore, 2007, Lippincott Williams & Wilkins, p 87; Wolff K et al: Development and structure of skin. In Fitzpatrick’s dermatology in general medicine, ed 7, Columbus, 2008, McGraw-Hill; Bryant RA, Nix DP: Acute and chronic wounds: current management concepts, ed 4, St Louis, 2012, Mosby. FIGURE 12-1 Three-dimensional representation of the skin and subcutaneous connective tissue layer showing the arrangement of hair, glands, and blood vessels. (From Black JM: Medical-surgical nursing: clinical management for positive outcomes, ed 8, St Louis, 2009, Saunders.) The skin has a number of clinically significant variations: (1) men have thicker skin than women; (2) the young and elderly have thinner skin than adults3; and (3) the skin on different parts of the body varies in thickness, number of appendages, and blood flow.4 These variations affect the severity of a burn injury or skin breakdown, as well as the process of tissue healing. The integument has seven major functions5: 1. Temperature regulation. Body temperature is regulated by increasing or decreasing sweat production and superficial blood flow. 2. Protection. The skin provides a physical, chemical, and biological barrier to protect the body from microorganism invasion, ultraviolet (UV) radiation, abrasion, chemicals, and dehydration. 3. Sensation. Multiple sensory cells within the skin detect pain, temperature, and touch. 4. Excretion. Heat, sweat, and water can be excreted from the skin. 5. Immunity. Normal periodic loss of epidermal cells removes microorganisms from the body surface, and immune cells in the skin transport antigens from outside the body to the antibody cells of the immune system. An intact integumentum also creates a physical barrier, and the relatively acidic pH of the skin’s surface provides chemical protection from microorganism invasion.6 6. Blood reservoir. Large volumes of blood can be shunted from the skin to central organs or muscles as needed. 7. Vitamin D synthesis. Modified cholesterol molecules are converted to vitamin D when exposed to UV radiation. Skin and body tissue destruction occurs from the absorption of heat energy and results in tissue coagulation. This coagulation is depicted in zones (Figure 12-2). The zone of coagulation, located in the center of the burn, is the area of greatest damage and contains nonviable tissue referred to as eschar. Although eschar covers the surface and may appear to take the place of skin, it does not have any of the characteristics or functions of normal skin. Instead, eschar is constrictive, attracts microorganisms, houses toxins that may circulate throughout the body, and prevents progression through the normal phases of healing.3 The zone of stasis, which surrounds the zone of coagulation, contains marginally viable tissue which can easily be further damaged from processes such as hypoperfusion, edema, or infection. Proper wound care can minimize this conversion and preserve the integrity of the viable tissue in this zone. The zone of hyperemia, the outermost area, is the least damaged and heals rapidly unless additional tissue injury occurs.7–9 FIGURE 12-2 Zones of injury after a burn. The zone of coagulation is the portion irreversibly injured. The zones of stasis and hyperemia are defined in response to the injury. (From Townsend Jr CM, Beauchamp RD, Evers BM, Mattox KL: Sabiston textbook of surgery: the biological basis of modern surgical practice, ed 19, Philadelphia, 2012, Saunders.) The depth of a burn can be described as superficial, moderate partial thickness, deep partial thickness, or full thickness (Figure 12-3). Each type has its own appearance, sensation, healing time, and level of pain, as described in Table 12-2. First-degree burns have no significant structural damage and therefore no zone of stasis or coagulation. Differentiation between moderate and deep second-degree burns can be made based on the presence of the zones of coagulation, stasis, and hyperemia in the deeper burns while moderate second-degree burns will only have zones of stasis and hyperemia. Third-degree burns contain a significant and easily identifiable zone of coagulation as well.10 TABLE 12-2 Data from Wiebelhaus P, Hansen SL: Burns: handle with care, RN 62:52-75, 1999; Gomez R, Cancio LC: Management of burn wounds in the emergency department, Emerg Med Clin North Am 25:135-146, 2007; Arnoldo B, Klein M, Gibran MS: Practice guidelines for the management of electrical injuries, J Burn Care Res 27(4):439-447, 2006; Pham TN, Gibran NS, Heimbach DM: Evaluation of the burn wound: management decisions. In Herndon DN, editor: Total burn care, ed 3, Philadelphia, 2007, Saunders, p 119. FIGURE 12-3 The depth of burn injuries from (A) superficial to (D) full thickness. (From Walsh M, editor: Nurse practitioners: clinical skills and professional issues, Oxford, England, 1999, Butterworth-Heinemann.) A series of physiologic events occurs after a burn (Figure 12-4). The physical therapist must appreciate the multisystem effects of a burn injury—namely, that the metabolic demands of the body increase dramatically. Tissue damage or organ dysfunction can be immediate or delayed, minor or severe, and local or systemic.11 A summary of the most common complications of burns is listed in Table 12-3. The amount of total body surface area involved in the burn and the presence of inhalation injury are the primary risk factors for mortality after burn injury.12 TABLE 12-3 Systemic Complications of Burn Injury Data from Linares HA: The burn problem: a pathologist’s perspective. In Herndon DN, editor: Total burn care, London, 1996, Saunders. FIGURE 12-4 The physiologic sequelae of major burn injury. BUN, Blood urea nitrogen; Cl−, chlorine; Hct, hematocrit; K+, potassium; Na+, sodium; O2, oxygen; RBC, red blood cell; WBC, white blood cell. (Modified from Marvin J: Thermal injuries. In Cardona VD, Hurn PD, Bastnagel Mason PJ, et al, editors: Trauma nursing from resuscitation through rehabilitation, ed 2, Philadelphia, 1994, Saunders; Demling RH, LaLonde C: Burn trauma, New York, 1989, Thieme, p 99.) Thermal burns are the result of conduction or convection, as in contact with a hot object, liquid, chemical, flame, or steam. In order of frequency, the common types of thermal burns are scalds, flame burns, flash burns, and contact burns (Table 12-4).13 The severity of the burn depends on the location of the burn, the temperature of the source, and the duration of contact.14 TABLE 12-4 Thermal Burns: Types and Characteristics Data from Warden GD, Heimbach DM: Burns. In Schwartz SI, editor: Principles of surgery, vol 1, ed 7, New York, 1999, McGraw-Hill; Edlich RF, Moghtader JC: Thermal burns. In Rosen P, editor: Emergency medicine concepts and clinical practice, vol 1, ed 4, St Louis, 1998, Mosby. An electrical burn is caused by exposure to a low- or high-voltage current and results in varied degrees of visible cutaneous tissue destruction at the contact points, as well as less visible but massive damage of subcutaneous tissue, muscle, nerve, and bone.15 Tissue necrosis of these deeper structures occurs from the high heat intensity of the current and the electrical disruption of cell membranes.13 Tissue damage occurs along the path of the current, with smaller distal areas of the body damaged most severely. This pattern of tissue damage accounts for the high incidence of amputation associated with electrical injury.13,16 The severity of an electrical burn depends primarily on the duration of contact with the source, the voltage of the source, the type and pathway current, and the amperage and resistance through the body tissues.16 Electrical burns are characterized by deep entrance and exit wounds and arc wounds. The entrance wound is usually an obvious necrotic and depressed area, whereas the exit wound varies in presentation. The exit wound can be a single wound or multiple wounds located where the patient was grounded during injury.14 An arc wound is caused by the passage of current directly between joints in close opposition. For example, if the elbow is fully flexed and an electrical current passes through the arm, burns may be located at the volar aspect of the wrist, antecubital space, and axilla.13 Complications specific to electrical injury include13,17: • Cardiovascular: Cardiac arrest (ventricular fibrillation for electric current or systole for lightning), arrhythmia (usually sinus tachycardia or nonspecific ST segment changes) secondary to alterations in electrical conductivity of the heart, myocardial contusion or infarction, or heart wall or papillary muscle rupture. • As a result of the high risk of fatal arrhythmias in this population, the American Burn Association (ABA) recommends an electrocardiogram (ECG) be performed on all patients who sustain electrical injuries, and those with a documented loss of consciousness or presence of arrhythmia following injury should be admitted for telemetry monitoring.18 • Neurologic: Headache, seizure, brief loss of consciousness or coma, peripheral nerve injury (resulting from ischemia), spinal cord paralysis (from demyelination), herniated nucleus pulposus, or decreased attention and concentration. • Orthopedic: Dislocations or fractures secondary to sustained muscular contraction or from a fall during the electrical injury. • Other: Visceral perforation or necrosis, cataracts, tympanic membrane rupture, anxiety, depression, or posttraumatic stress disorder. Lightning, considered a form of very high electrical current, causes injury via four mechanisms19: 1. Direct strike, in which the person is the grounding site 2. Flash discharge, in which an object deviates the course of the lightning current before striking the person 3. Ground current, in which lightning strikes the ground and a person within the grounding area creates a pathway for the current 4. Shock wave, in which lightning travels outside the person and static electricity vaporizes moisture in the skin Chemical burns can be the result of reduction, oxidation, corrosion, or desecration of body tissue with or without an associated thermal injury.20 The severity of the burn depends on the type and concentration of the chemical, duration of contact, and mechanism of action. Unlike thermal burns, chemical burns significantly alter systemic tissue pH and metabolism. These changes can cause serious pulmonary complications (e.g., airway obstruction from bronchospasm, edema, or epithelial sloughing) and metabolic complications (e.g., liver necrosis or renal dysfunction from prolonged chemical exposure). A nonblistering sunburn is a first-degree burn from the overexposure of the skin to UV radiation.8 More severe burns can also occur due to UV exposure and would appear as described in Table 12-2. Ionizing radiation burns with or without thermal injury occur when electromagnetic or particulate radiation energy is transferred to body tissues, resulting in the formation of chemical free radicals.21 Ionizing radiation burns usually occur in laboratory or industrial settings, but can also be seen in the medical setting following radiation treatment, most often for cancer. The severity of the ionizing radiation burn depends on the dose, the dose rate, and the tissue sensitivity of exposed cells. Often referred to as acute radiation syndrome, complications of ionizing radiation burns include21: • Gastrointestinal: Cramps, nausea, vomiting, diarrhea, and bowel ischemia • Hematologic: Pancytopenia (decreased number of red blood cells, white blood cells, and platelets), granulocytopenia (decreased number of granular leukocytes), thrombocytopenia (decreased number of platelets), and hemorrhage The extent and depth of the burn determine its severity and dictate acute care management. Accurate assessment of the extent of a burn is necessary to calculate fluid volume therapy and is a predictor of morbidity.22 The extent of a burn injury is referred to as total body surface area (TBSA) and can be calculated by using the rule of nines, the Lund and Browder formula, or the palmar method. The rule of nines divides the adult body into sections, seven of which are assigned 9% of TBSA. The anterior and posterior trunks are each assigned 18%, and the genitalia are assigned 1% (Figure 12-5). This formula is quick and easy to use, especially when a rapid initial estimation of TBSA is needed in the field or the emergency room. To use the rule of nines, the burned area is drawn in on the diagram and the percentages are added for a TBSA. Modifications can be made if an entire body section is not burned. For example, if only the posterior left arm is burned, the TBSA is 4.5%. A modified version is available for use in children. The Lund and Browder formula divides the body into 19 sections, each of which is assigned a different percentage of TBSA (Table 12-5). These percentages vary with age from infant to adult to accommodate for relative changes in TBSA with normal growth. The Lund and Browder formula is a more accurate predictor of TBSA than the rule of nines because of the inclusion of a greater number of body divisions along with the adjustments for age and growth. TABLE 12-5 Lund and Browder Method of Assessing the Extent of Burns* *Values represent percentage of total body surface area. Adapted from McManus WF, Pruitt BA: Thermal injuries. In Feliciano DV, Moore EE, Mattox KL, editors: Trauma, Stamford, CT, 1996, Appleton & Lange, p 941; Lund CC, Browder NC: The estimation of areas of burns, Surg Gynecol Obstet 79:355, 1944. To estimate TBSA of irregularly shaped burns, ABA Practice Guidelines recommend preferential use of the Lund and Browder supplemented with the palmar method, in which size of the patient’s palm is used to estimate the size of the burn. The palm represents approximately 1% of TBSA.22,23 The assessment of burn depth provides a clinical basis in the decision of appropriate burn care or surgery and the expected functional outcome and cosmesis.24 Refer to Figure 12-3 and Table 12-2 to review the depth of tissue destruction in burn injuries. Although clinical observation remains the standard for burn depth estimation, there is often error or underestimation. Experimental technologies for more precise burn depth estimation include cell biopsy, vital dyes, fluorescein fluorometry, laser Doppler flowmetry, thermography, ultrasound, and nuclear magnetic resonance.13 A burn is considered to be a dynamic wound in that it can change in appearance, especially during the first few days following injury. Therefore exact classification of depth of injury cannot be made until the burn has fully developed.9 In addition, later conversion of a burn from a superficial to a deeper injury can occur as a result of inadequate burn management, edema, infection, inadequate fluid resuscitation, impaired perfusion, or excessive pressure from dressings or splints.1,25 In addition to the burn’s extent and depth, the presence of other associated injuries and premorbid medical conditions determines what level of care is optimal for the patient. The American Burn Association recommends medical care at a burn center if the patient has any of the following26: • Partial-thickness burns greater than 10% TBSA • Burns that involve the face, hands, feet, genitalia, perineum, or major joints • Third-degree burns in any age group • Electrical burns, including lightning injury • Burn injury in patients who have preexisting medical disorders that could complicate management, prolong recovery, or affect mortality • Burns and concomitant trauma (such as fractures) in which the burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, patients may be stabilized initially in a trauma center before being transferred to a burn unit. Physician judgment is necessary in such situations and should be in concert with the regional medical control plan and triage protocols. • Burns in children who are in hospitals without qualified personnel or equipment for the care of children • Burn injury in patients who require special social, emotional, or long-term rehabilitative intervention ABA Practice Guidelines define an inhalation injury as aspiration of superheated gases, steam, hot liquids, or noxious products of incomplete combustion.23 This inhalation, which may be related to burn injuries, can cause asphyxia, direct cellular injury, or both. The severity of inhalation injury is dependent on the inhalant and exposure time and significantly increases mortality. Inhalation injury is suspected based on a combination of history and physical exam and is confirmed with diagnostic studies such as a bronchoscopy.28 Injury can be suspected if the patient had a known exposure to noxious inhalants, especially in an enclosed space, or if the patient demonstrates any of the following: • Burns on the face, neck, or upper chest • Singed eyebrows or nose hair • Laryngeal or mucosal edema with possible loss of airway patency • Arterial blood gas levels consistent with hypoxia • The presence of soot in the mouth or sputum The oropharynx and tracheobronchial tree are usually damaged by thermal injury, whereas the lung parenchyma is damaged by the chemical effects of the inhalant. Thermal airway injury is characterized by immediate upper-airway mucosal edema, erythema, hemorrhage, and ulceration.13 Elective endotracheal intubation is often indicated with this type of injury, as progressive edema can readily lead to airway obstruction.30 The pathophysiology of inhalation injury generally occurs in three stages: (1) inhalation injury (0 to 36 hours after injury), (2) pulmonary edema (6 to 72 hours after injury), and (3) bronchopneumonia (3 to 10 days after injury). Pulmonary edema occurs from increased lung capillary permeability, increased bronchial blood flow, and impaired lymph function.31 De-epithelialization and exudate formation occurs throughout the airways, as well as decreased alveolar surfactant.13 Decreased lung compliance (functional residual capacity and vital capacity) and hypoxia are the primary effects of inhalation injury, each of which is dependent on the location and severity of the injury. Supplemental oxygen, elective intubation, bronchodilators, and fluid resuscitation are initiated to maximize gas exchange and reverse hypoxia.32–34 The inhalation of carbon monoxide (CO), which is a colorless, odorless, tasteless, combustible, nonirritating gas produced by the incomplete combustion of organic material, results in asphyxia. CO molecules displace oxygen molecules from hemoglobin to form carboxyhemoglobin and shift the oxyhemoglobin curve to the left, thereby decreasing the release of oxygen. In addition, CO molecules increase pulmonary secretions and decrease the effectiveness of the mucociliary elevator.35 Elevated carboxyhemoglobin levels can cause headache, disorientation, nausea, visual changes, syncope, coma, or death depending on the concentration and exposure time. CO poisoning is usually reversible with the use of 100% oxygen if the patient has not lost consciousness.13 After a burn, fluid shifts from vascular to interstitial and intracellular spaces because of increased capillary pressure, increased capillary and venular permeability, decreased interstitial hydrostatic pressure, chemical inflammatory mediators, and increased interstitial protein retention.36 This is compounded by evaporative water loss from a disruption of the skin.37 In burns of more than 20% TBSA, this fluid shift becomes massive and requires immediate fluid repletion.24 This fluid shift, referred to as burn shock, is a life-threatening condition because of hypovolemia and the potential for shock-induced renal failure (see Figure 12-4). Plasma, sodium-rich solutions, and other fluids are infused according to a formula derived from individual TBSA and body weight. The specific formula used varies according to hospital preference. During and after fluid administration, the patient is monitored closely for adequacy of fluid resuscitation. Heart rate, blood pressure, cardiac output, base deficit, urine output, and bowel sounds provide valuable information about the effectiveness of fluid resuscitation, as do peripheral body temperature, capillary refill, and mental status.36,38 Prevention of infection at the burn site(s) is crucial in the resuscitative and reparative phases of burn care. The patient with a major burn is considered immunocompromised because of the loss of skin and the inability to prevent microorganisms from entering the body. Infection control is achieved by the following24: • Observation of the patient for signs and symptoms of sepsis (see the Sepsis section in Chapter 13) • Minimization of the presence of microorganisms in the patient’s internal and external environment • Use of aseptic techniques in all interactions with the patient • Use of topical antimicrobial agents or systemic antibiotics, as needed A patient with a burn injury can experience pain as a result of any of the following: Patients may also experience fear from the injury and burn treatment, which can exacerbate pain. Analgesia, given intravenously, is therefore started as soon as possible. Opioids are the mainstays in pain management, supplemented by nonsteroidal antiinflammatory drugs (NSAIDs), mild analgesics, parenteral and inhaled anesthetic agents, and anxiolytics. Initial doses of opioids may exceed the standard weight-based recommendations in order to achieve adequate pain control. No evidence exists for any increased risk of addiction in this population as compared to others who require opioids for pain management.39 Refer to Chapters 19 and 21 for more information about pharmacologic agents. To neutralize the burn source, the patient’s clothing and jewelry are removed, and the burn is rinsed or lavaged. Once the patient is medically stable, the burn is debrided, cleaned, and dressed with the hospital’s or burn unit’s topical agent of choice. Topical antimicrobial agents may be used in an attempt to prevent or minimize bacterial growth. There are a variety of antimicrobial agents, each with their own application procedures, advantages, and disadvantages. Ideally, the antimicrobial agent of choice should penetrate eschar, work against a wide variety of microorganisms, have minimal systemic absorption, and not impede healing.40 The physician determines whether to cover the burn or leave it open, estimates the time frame for burn repair, and determines the need for surgical intervention. Circumferential burns of the extremities or trunk can create neurovascular and respiratory complications. Inelastic eschar paired with edema can cause increased tissue swelling in all directions with the result of decreased blood flow, nerve compression, impaired chest expansion, and increased compartment pressures. In the extremities, tissue ischemia and loss of limb can ensue if these conditions are not treated with escharotomy or fasciotomy. Escharotomy is the surgical incision through eschar to decompress tissue below the burn. Fasciotomy is the surgical incision through fascia to decompress tissue within a fascial compartment. Both procedures are typically performed at the bedside. Clinical indications for escharotomy or fasciotomy are decreased arterial blood flow, as determined by loss of Doppler flowmetry signal, or increased compartment pressure measurements (≥30 mm Hg).40 Tissue healing occurs over days to months according to the depth of the burn and is described in the Process of Wound Healing section. For a discussion of variables that can slow the process of healing, see the Factors That Can Delay Wound Healing section. After the burn has closed, a scar forms. A burn scar may be normotrophic, with a normal appearance when dermal collagen fibers are arranged in an organized parallel formation, or hypertrophic, with an abnormal raised appearance as a result of the disorganized alignment of dermal collagen fibers.41 Another form of abnormal appearance or pathologic scar is a keloid scar, which tends to extend beyond the boundaries of the primary wound (whereas a hypertrophic scar will stay within the boundaries of the wound).42 A keloid scar is more prevalent in people of color and presents as a prominent, raised scar as a result of excessive collagen accummulation.43 The cornerstone of present surgical management is early excision and grafting in burns that are unlikely to heal in a reasonable time frame through conservative treatment.44 Excision is the surgical removal of eschar and exposure of viable tissue to minimize infection and promote burn closure. Grafting is the implantation or transplantation of skin onto a prepared wound bed.45 Early burn closure minimizes scarring, infection, the incidence of multisystem organ failure, and morbidity. Table 12-6 describes the various types of excision and grafting. Table 12-7 describes the different artificial and biological skin substitutes available for use when there is a lack of viable autograft sites. Many of these are used in the management of other wound etiologies as well. TABLE 12-6 Types of Excision and Grafting Data from Miller SF, Staley MJ, Richard RL: Surgical management of the burn patient. In Richard RL, Staley MJ, editors: Burn care and rehabilitation: principles and practice, Philadelphia, 1994, FA Davis; Sheridan RL, Tompkins RG: Alternative wound coverings. In Herndon DN, editor: Total burn care, ed 3, Philadelphia, 2007, Saunders, p 239; Muller M, Gahankari D, Herndon DN: Operative wound management. In Herndon DN, editor: Total burn care, ed 3, Philadelphia, 2007, Saunders, p 117. TABLE 12-7 Skin Substitutes for the Treatment of Burns and Wounds Data from Muller M, Gahankari D, Herndon DN: Operative wound management. In Herndon DN, editor: Total burn care, ed 3, 2007, p 117; Greenhalgh DB: Wound healing. In Herndon DN, editor: Total burn care, ed 3, Philadelphia, 2007, Saunders, p 578; udllabs.com; transcyte.com/index.html; dermagraft.com; lifecell.com/health-care-professionals; ilstraining.com/imwd/imwd/imwd_it_02.html; apligraf.com; oasiswoundmatrix.com; kci1.com/KCI1/tissue-regeneration. Surgical excision and grafting are completed at any site if patient survival will improve. If morbidity is greater than 50%, the priority is for the excision and grafting of large flat areas to rapidly reduce the burn wound area.40 Grafting is otherwise performed to maximize functional outcome and cosmesis, with the hands, arms, face, feet, and joint surfaces grafted before other areas of the body.46 Permanent grafting is ideal; however, grafting may be temporary in order to provide short-term closure to assist in pain control, drainage management, and protection of the underlying wound tissue. Temporary grafting may be indicated in small wounds expected to heal secondarily or in large wounds for which an autograft would not last, or if permanent coverage is not available.47 Grafts, which typically adhere in 2 to 7 days, may not adhere or “take” in the presence of any of the following45,46: • Movement or shear of the graft on the recipient site • Infection, inadequate blood flow, or hematoma formation at the recipient site
Burns and Wounds
Preferred Practice Patterns
Body Structure and Function: Normal Integument
Structure
Function
Burns
Pathophysiology of Burns
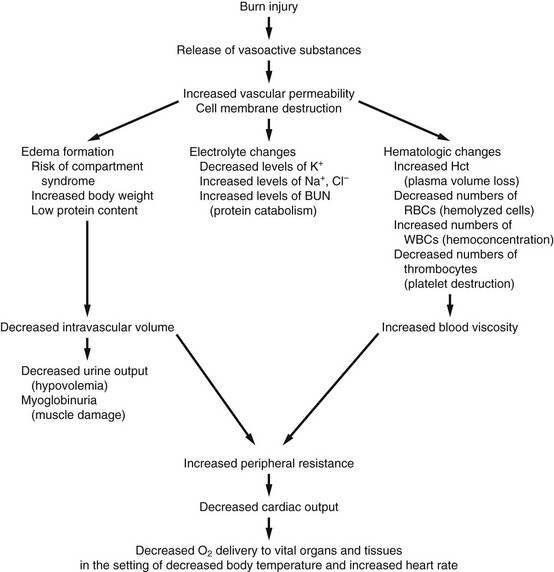
Physiologic Sequelae of Burn Injury
Body System
Complications
Respiratory
Inhalation injury, restrictive pulmonary pattern (which may occur with a burn on the trunk), atelectasis, pneumonia, microthrombi, and adult respiratory distress syndrome
Cardiovascular
Hypovolemia/hypotension, pulmonary hypertension, subendocardial ischemia, arrhythmias, anemia, deep venous thrombosis, and disseminated intravascular coagulopathy
Gastrointestinal/genitourinary
Stress ulceration, hemorrhage, ileus, ischemic colitis, cholestasis, liver failure, and urinary tract infection
Renal
Edema, hemorrhage, acute tubular necrosis, and acute renal failure
Types of Burns
Thermal Burns
Burn Type
Description
Characteristics
Scald burn
Spill of or immersion in a hot liquid, such as boiling water, grease, or tar
Often causes deep partial- or full-thickness burns.
Exposure to thicker liquids or immersion causes a deeper burn from increased contact time.
Immersion burns commonly cover a larger total body surface area than do spills.
Flame burn
Flame exposure from fire or flammable liquids, or ignition of clothing
Often causes superficial and deep partial-thickness burns.
Associated with carbon monoxide poisoning and inhalation injuries.
Flash burn
Explosion of flammable liquid, such as gasoline or propane
Often causes partial-thickness burns.
Burns may be distributed over all exposed skin.
Associated with upper airway thermal damage.
Most common in the summer and associated with the consumption of alcohol.
Contact burn
Exposure to hot objects
Often causes deep partial- or full-thickness burns.
Most common cause of serious burns in the elderly.
Electrical Burns
Lightning.
Chemical Burns
Ultraviolet and Ionizing Radiation Burns
Burn Assessment and Acute Care Management of Burn Injury
Classification of a Burn
Assessing the Extent of a Burn
Rule of Nines
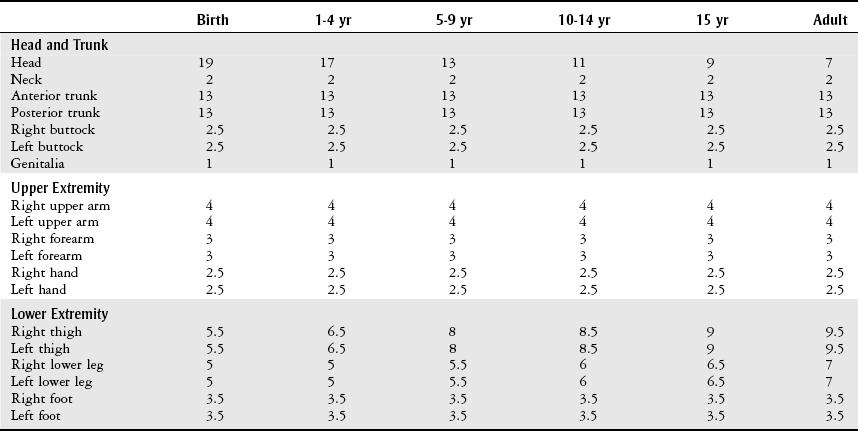
Lund and Browder Formula
Estimating the Extent of Irregularly Shaped Burns
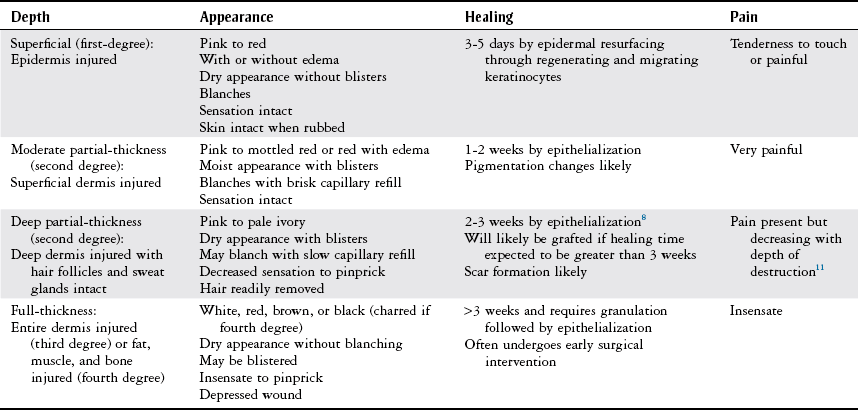
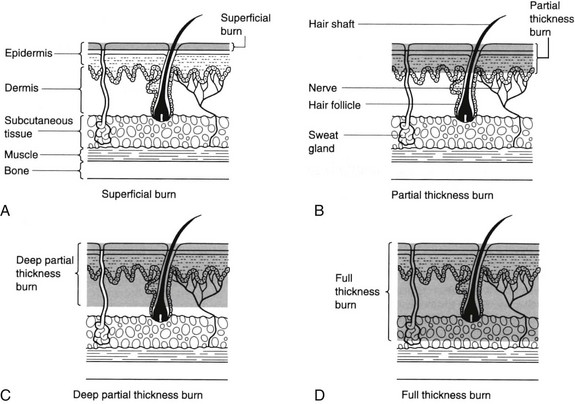
Assessing the Depth of a Burn
Acute Care Management of Burn Injury
Admission Guidelines
Inhalation Injury and Carbon Monoxide Poisoning.
Burn Care in the Resuscitative Phase.
Burn Management in the Reparative Phase.
Procedure
Description
Tangential excision
Removal of eschar in successive layers down to the dermis
Full-thickness excision
Removal of eschar as a single layer down to the subcutaneous tissue
Split-thickness skin graft (STSG)
Graft consisting of epidermis and a portion of dermis
Full-thickness skin graft (FTSG)
Graft consisting of epidermis and the entire dermis
Mesh graft
Graft placed through a mesher to expand the size approximately 3-4 times prior to placement on the recipient site
Sheet graft
Graft placed on the recipient site as a single piece without meshing
Autograft
Surgical harvesting of a patient’s own skin from another part of the body (donor site) and placing it permanently on the burn (recipient site)
Cultured epidermal autograft (CEA)
Autograft of unburned epidermal cells cultured in the laboratory, which provides epidermal replacement only
Composite skin graft
Autograft of unburned epidermal and dermal cells cultured in the laboratory with the intention of immediate replacement of both the dermis and epidermis
Allogenic graft/allograft
Temporary graft from donated human cadaver skin
Heterograft/xenograft
Temporary graft from another animal species, typically of porcine skin
Amnion graft
Temporary graft from placental membrane
Product
Description
Use
Biobrane (UDL Laboratories, Rockford, IL)
Temporary skin substitute.
Two-layered graft composed of nylon mesh impregnated with porcine collagen and silicone; the outer silicone layer is permeable to gases but not to fluid or bacteria.
Spontaneously separates from a healed wound in 7-14 days.
Clean, freshly debrided partial-thickness burns
Donor sites
Protect a meshed autograft
Limited success on full-thickness burns because of infection with residual necrotic tissue
Dermagraft (Advanced BioHealing, San Diego, CA)
Dermal substitute composed of human fibroblasts, extracellular matrix, and a bioreabsorbable scaffold.
Derived from newborn foreskin tissue.
Remains in wound, assisting in restoration of the dermal bed in preparation for re-epithelialization.
Full-thickness diabetic foot ulcers without underlying structure exposure
TransCyte (Advanced BioHealing, San Diego, CA)
Temporary skin substitute composed of a polymer membrane and newborn human fibroblast cells cultured on a porcine collagen-coated nylon mesh. The fibroblasts secrete human dermal collagen, matrix proteins, and growth factors.
Surgically excised full-thickness and deep partial-thickness thermal burns before autograft placement
Partial-thickness burns that require debridement but are expected to heal without formal grafting
AlloDerm (LifeCell, Branchburg, NJ)
Composed of chemically treated cadaver dermis with the epidermal antigenic cellular components removed so that it is immunologically inert.
Provides dermal and basement layer replacement.
Repair or replacement of damaged integument, no specific limitations to wound type
Can be applied to a debrided burn with an ultrathin split-thickness autograft immediately applied over it
Integra (Integra Life Sciences, Plainsboro, NJ)
Two-layered material composed of a disposable outer silicone film that acts as a barrier to evaporative water loss and bacteria, and an inner layer of bovine collagen and chondroitin 6-sulfate that becomes incorporated into the burn to form a neodermis. When the neodermis becomes vascularized, the silicone covering is removed and replaced with thin autografts.
Full-thickness burns or deep partial-thickness burns
Also used in the repair of scar contractures
GRAFTJACKET (LifeCell, Branchburg, NJ)
Acellular dermal matrix from donated human cadaver skin.
Superficial and deep integumentary defects
Apligraf (Graftskin)
(Organogenesis, Canton, MA)
Bilayered skin substitute containing bovine collagen and human fibroblasts (which produce additional growth factors and proteins for dermal regrowth) and keratinocytes (which reproduce to replace the epithelial surface).
Human cellular components are derived from neonatal foreskin.
Chronic venous leg ulcers and diabetic foot ulcers
OASIS Wound Matrix (Cook Biotech, West Lafayette, IN)
Bioresorbable matrix derived from porcine small intestinal submucosa.
Partial- and full-thickness wounds of most etiologies (including donor sites and grafts)
Not indicated for use in third-degree burns
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Burns and Wounds
Only gold members can continue reading. Log In or Register to continue