Chapter 4 Burns and Plastic Surgery
Burns
Introduction
• The assessment and treatment of patients following a burn injury requires management by a dedicated burns team.
• Physiotherapists are an integral part of the team, which also includes; nurses, doctors, plastic surgeons, social workers, dieticians, psychologists and the patient.
• A team approach is regarded as the best way for the assessment and specialist care of these patients as the different role each team member plays contributes to the total care and outcome of the burn patient (Leveridge 1991).
• Injuries depend on the cause and extent of damage, with many being life changing physically, emotionally and psychologically. The injuries also affect the individual’s family.
• Management is geared to anticipating potential problems through the assessment of the patient.
• A burn injury comprises of damage to the skin of varying depths and can lead to complete skin loss with or without damage to the underlying tissues. Along with this an individual may present with other signs and symptoms affecting the respiratory, cardiovascular, orthopaedic and neurological systems.
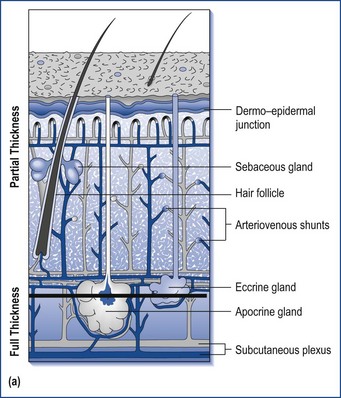
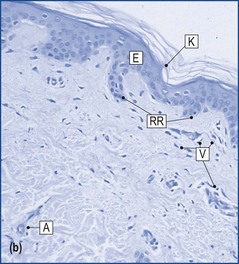
• The depth of skin damage is very important in deciding how the burn will be managed; this is normally conservative management with dressings or management with surgery (Richard and Staley 1994) (Figure 4.1a and 4.1b).
Classification of burns
Partial thickness burn
• Superficial dermal – Tissue damage means leakage of fluid between the layers of epidermis, resulting in blister formation, surrounded by erythema.
• Deep dermal – Tissue destruction involves the epidermis and superficial layers of the dermis.
Full-thickness burn
• These burns are not painful.
• They can involve muscle, tendon and bone.
• Skin loss means that there are no accessory skin structures such as hair follicles to epithelialise.
• Healing will therefore only occur by the epithelium migrating from the edge of the burn wound.
• It is only possible for a very small burn to heal in this way.
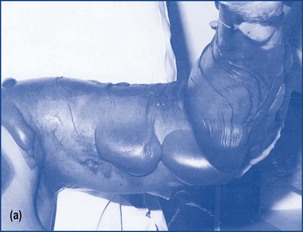
• Appears white, waxy looking, or charred black (Figure 4.3).
• Requires management by excision of necrotic tissue and skin grafting (Settle 1996).
Causes of burns
• Burns can be caused by excessive heat or cold, by chemicals, ultraviolet light or radiation.
• The most common causes of burns requiring hospital treatment are:
History
• Details of how the injury occurred, duration of contact, protection offered by clothing and first aid given can all provide an indication of the type and depth of a burn.
• As burns occur in traumatic circumstances it is important to ensure that other associated traumatic injuries have been eliminated, e.g. fractures, nerve injuries, spinal and head injuries.
Burns charts
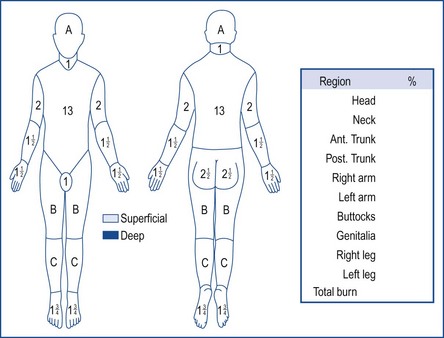
• These are used to record the distribution of the burns and are normally completed by an experienced burns doctor.
• Lund and Browder charts (Figure 4.4) are used to record total body surface area (TBSA) and the depth of the burns, which are documented as partial-thickness (PTB) or full-thickness burns (FTB) (Herndon 2007).
• The larger the total burn surface area, the worse the prognosis for the patient.
• It is important to calculate accurate TBSA, as this will guide the amount of fluid replacement that is required to stabilise the patient.
• The ‘rule of nines’ is another method of gauging the TBSA. This divides the body surface into 11 areas, each making up 9% of the total, apart from the perineum which is allocated 1% (Porter 2008).
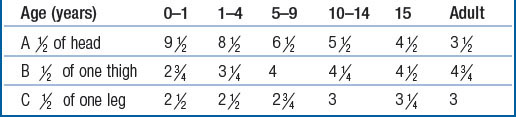
• There are separate charts for paediatrics. This takes into account the ratio of different body regions to the TBSA, which changes with age (Table 4.1).
Pathological changes
Burns shock
• The unique pathological changes include burns shock. This is the inability of the circulatory system to provide oxygen and nutrients and to remove metabolites (Settle 1986).
• The risk of burns shock is due to a decrease in circulatory plasma volume or hypovolaemia caused by plasma leaking from damaged capillaries.
• There is loss of proteins and electrolytes from the blood and there is an increase in blood viscosity.
• The body compensates by shutting down blood supply to the skin, abdominal organs and the kidneys.
• The massive fluid loss and risk of septicaemia gives rise to major cardiovascular instability. If left untreated the fall in cardiac blood pressure can lead to vital organ failure.
• The severity of shock is related to the surface area of skin damage.
• The BP, CVP, haematocrit, urine output and heart rate must be monitored during the acute burn period (Leveridge 1991). Volume of fluid transfusion is adjusted as required to maintain balance.
• The problems of sepsis, massive fluid loss, cardiovascular instability and high airway pressures mean that in order to treat the lung injury, physiotherapists have to repeatedly re-assess the consequences of their treatment in the context of the multi system problems (Keilty 1993).
Assessment for fluid resuscitation
• Fluid resuscitation will need to be commenced if the TBSA is; >10% in children and >15% in adults (Settle 1996).
• The amount of fluid will need to be calculated, so that it will restore and maintain adequate perfusion of blood to all body tissues. Thirty-six-hour fluid resuscitation is subdivided into numerous periods with the patient being regularly reassessed at the end of each period. Developing signs of shock suggest inadequate fluid management.
Initial findings
• Burns with a TBSA of more than 10% in children and 15% in adults, those with suspected inhalation injury or burns on specific areas of the body, e.g. hands and feet, are generally treated in a specialised burns unit or centre (Porter 2008).
• The specialist burns unit approach leads to improved patient care and provides support for each member of the team in working situations that can be stressful.
• Therapy intervention begins within the first 24–48 hours following admission; therapists have an important role throughout all stages of recovery, to give encouragement, instil confidence and gain co-operation of the patient to enable the patient to be managed effectively.
• Assessment of burns requires good organisational skills, due to the complexity of these injuries.
• The main problems that are likely to be found include:
• Following admission wounds will be cleaned, debrided and dressed and the process of fluid resuscitation and stabilisation will begin.
• Large burns are life-threatening due to fluid loss, excessive cooling, poorly maintained body temperature and risk of infection.
• Surgeons are responsible for overall evaluation of the burn and patient resuscitation at this stage.
• The therapist will begin their assessment of the patient according to the TBSA of the burn, pre-existing medical conditions and the patient’s respiratory status. It is important to confirm details of the injury.
• Information may be obtained from medical notes or charts, other members of the burns team, e.g. doctors, the patient and their family.
• The patient will be nursed in a side room, possibly on an intensive therapy unit (ITU).
• The room temperature is kept higher than normal, at 28°C or more to regulate the patient’s subnormal temperature due to burns shock and the loss of the thermoregulation function of the skin, in order to counteract the shutting down of the peripheral circulation.
• There will be strong odours due to plasma leaking from wounds, necrotic tissue and any infections, e.g. Pseudomonas.
• The patient may be ventilated, following an inhalation injury, or if there is excessive head or neck swelling.
• The patient may be sedated or alert and anxious.
• They may have dressed burns and/or exposed burns with associated erythema, blisters, and yellow/white skin, blackened tissues. Dressings may be bulky, to absorb the oozing from wounds.
• Hands may be in flammazine bags, permitting exercise without the restriction of dressings.
• Swelling may be pronounced, altering facial appearance and possibly reducing vision (Figure 4.5).
Inhalation injury
• Smoke inhalation is the primary cause of fire-related deaths, increasing mortality by 20% (Shirani et al 1987).
• Inhalation injuries can be due to thermal damage to the upper respiratory tract, or by chemical damage from the inhalation of toxic particles or fumes, such as cyanide.
• The airway responds by producing mucosal oedema, erythema and ulceration.
• The resultant damage affects the body’s ability to maintain the ventilation/perfusion balance.
• Secondary damage can occur in response to inflammation, which leads to increased vascular permeability, in turn leading to exacerbation of pulmonary oedema, increasing respiratory resistance and reducing lung compliance.
• Patients with inhalation burns are at risk of developing pneumonia, which can increase the mortality rate by up to 40% (Shirani et al 1987).
• A patient having three of the following clinical factors will in all probability have a significant inhalation injury. These may be difficult to diagnose on first admission. They should be recorded in physiotherapy records.
• Factors indicating an inhalation injury:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree