INTRODUCTION
Burn care and injury management continue to advance throughout the developed world, leading to improved survival and rehabilitation of individuals who suffer burn injuries. These individuals require a comprehensive approach to care to help them achieve full independence and maximum recovery from their injuries. Current estimates suggest that more than 1.2 million individuals in the United States require care for burn injuries annually, and this number is significantly higher in many other countries throughout the world. Successful rehabilitation of a person with a burn injury requires a team approach in which each member provides essential resources and skills to help the individual transition from being a “victim” of a burn to being a functionally independent “survivor.”
EPIDEMIOLOGY
Burns cause approximately 60,000 hospitalizations and over 6000 deaths annually in the United States. Burn injuries are most common among males (∼70% of cases) between the ages of 16 and 40 years; however, both young and old are highly susceptible to burn injury. Burns are the second most common form of abuse among children aged 1–12 years, and the second leading cause of accidental death among adults older than 60 years.
Mortality from major burns has been significantly reduced in North America. Nonetheless, according to the American Burn Association National Burn Repository, the mortality rate for the median lethal dose (LD50) for burns is 80%. This median is even higher in the pediatric population between the ages of 1 and 15 years, where the rate reaches just over 95%. Several negative predictors influence burn survival, including the presence of inhalation injury, increased age, presence of other medical comorbidities (eg, diabetes mellitus or chronic obstructive pulmonary disease), and higher overall surface area injury.
The most common burn injuries affect approximately 10% of total body surface area (TBSA) and are the result of flame contact or scald. Of patients with these types of burns, approximately 95% survive their injuries and hospitalizations. Burns can also result from electrical contact, chemical contact, radiation exposure, and, to a lesser degree, various skin syndromes. Depending on the cause, patients with these injuries will require varying amounts of wound care, surgery, rehabilitation, and aftercare to recover.
PATHOPHYSIOLOGY
Human adult skin is the largest organ in the body, with a surface area of approximately 2 m2, an overall depth of approximately 2 mm, and a weight of approximately 6 lb. The skin comprises three primary layers—epidermis, dermis, and hypodermis (subcutaneous tissue)—and serves many key functions, including thermoregulatory, neurosensory, immunologic, evaporative, metabolic (eg, oxygen, nitrogen, and carbon dioxide diffusion), and protective. Equally as important is its role in physical identity.
The uppermost layer is the epidermis, composed primarily of five layers of thin, avascular, keratinized epithelium having as its primary role the protective (germ- and injury-resistant) function of the skin. The deeper dermal layer is composed of two layers: an upper papillary dermis, composed of loose areolar connective tissue, and a deeper reticular layer, composed of dense elastic and collagen fibers and housing many glands and vessels. This layer is connected to the underlying hypodermis and provides the mechanical strength that enables the dermis to attach to the underlying tissues. The hypodermis is the insulating layer to the underlying subcutaneous structures.
Burn injuries affect the skin in three histologic zones extending away from the center of injury in two directions (out and down). Injuries to each zone produce characteristic histologic changes, ranging from hyperemia to stasis to coagulation. The zone of hyperemia is the outermost zone of injury (the area least affected by direct injury). Injury to this zone results in vasodilation and minimal cellular death. In minor burns, this may be the only zone of injury. The zone of stasis is closer to the center of the burn site and experiences a deeper injury. Burns to this zone result in greater cell necrosis if concomitant factors such as vascular constriction, edema, and vascular thrombosis or ischemia are not addressed during the resuscitation process. The zone of coagulation is closest to the direct injury and experiences the deepest destruction. Burns to this zone produce cells that are completely necrotic and will require surgical intervention to effectively replace and repair the damaged tissues.
CLINICAL FINDINGS
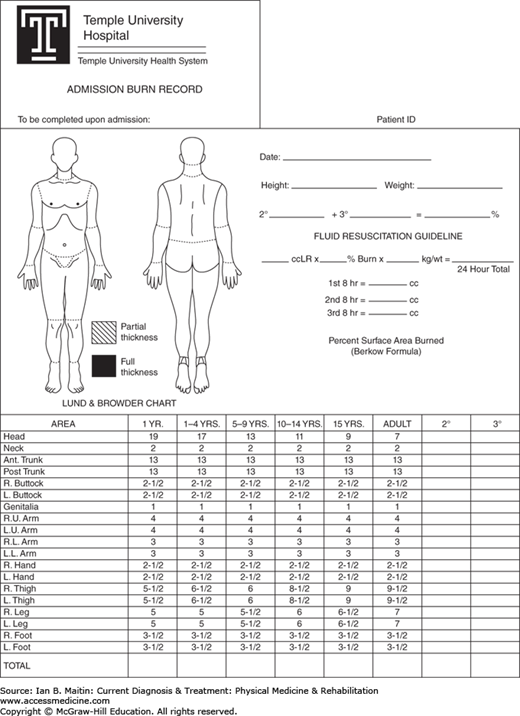
Burns are classified according to the depth of injury to the skin and the total surface area of the body that is affected. These two classifications are important because the greater the size, the more potential complications and contractures can arise, and the larger the depth of injury, the greater the mortality rate will be. Various methods have been promoted for calculation of the TBSA. A well-known method of estimation is the so-called Rule of Nines, which divides the body into various segments, each accounting for 9% of the surface area. Although widely used, this method has been found to undercalculate size differences based on age. (For example, the head represents a larger proportion of the body in children than in adults.) More routinely, burn size estimation is calculated using diagrams, such as the Lund and Browder chart (Figure 25–1). Additionally, calculation can be performed using the palm method, in which the palmer surface of the patient’s hand represents approximately 1% of TBSA.
Computer modeling systems are currently being developed that will incorporate overall body mass into the calculation processes; however, these are not yet available. Thus, assessment is still routinely performed by direct visual inspection of the burn. Most importantly, it is the location of the burn injury, in addition to the depth, that tends to be most predictive of the overall rehabilitative needs of the patient. In areas with highly mobile joints or articular surfaces such as the face and hands, joint surfaces are more likely to heal with scar hypertrophy, leading to further contractures and loss of overall function.
Burn depth is classified as superficial, partial-thickness, full-thickness, and subdermal. These classifications are also referred to as first degree, second degree, third degree, and fourth degree, respectively. Partial-thickness burns (second degree) can be further subdivided into either superficial or deep categories. Depth of injury is important from a wound-healing perspective, because it correlates strongly with the formation of scar tissue and the potential for subsequent contracture development.
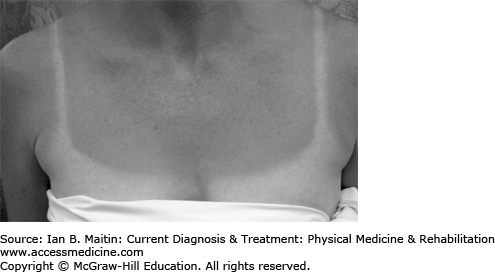
A superficial burn involves only the epidermal surface and leaves the epidermis intact (Figure 25–2). This type of burn is usually erythematous and painful, does not contain blisters, has characteristics similar to “sunburn,” and will heal spontaneously in less than a week, usually without any scarring.
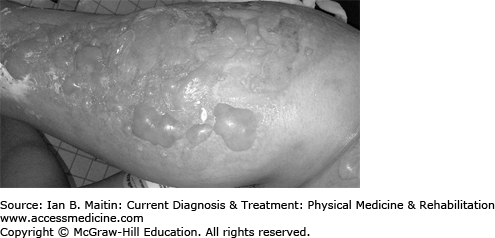
A superficial partial-thickness burn involves both the epidermis and dermis. This type of burn is quite painful, appears moist and pink, has many blisters, and blanches with pressure (Figure 25–3). Superficial partial-thickness burns usually heal spontaneously in 2 weeks, with minimal scaring or loss of function; however, some pigment changes can occur.
A deep partial-thickness burn also involves both the epidermis and dermis, and usually extends more deeply into the dermal structures. This type of burn is also painful but is not as tender as more superficial burns. The burn site may blister, but the overall appearance is red and less moist, with some areas that appear pale or slightly white. This type of burn should be monitored, because such burns, if allowed to heal spontaneously for more than 3 weeks, are much more likely to produce contractures and loss of function due to the prolonged inflammatory wound process. This type of injury may require a skin graft to improve the rate of healing and to limit the potential for contraction or loss of function.
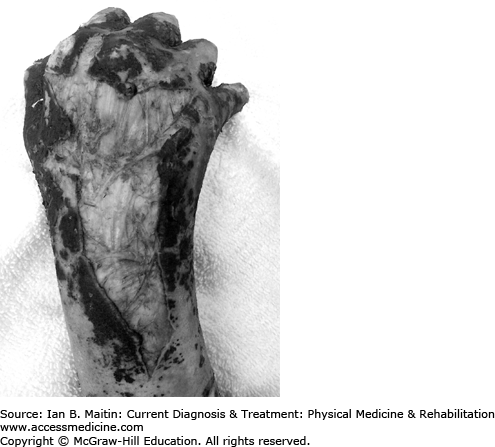
A full-thickness burn injury involves the loss of the epidermis and the entire dermis. These burns are pale and leathery in appearance, dry, insensate, and have taut and relatively inflexible skin (Figure 25–4). Full-thickness burns require skin grafting and cause scarring and higher loss of function if not effectively managed throughout the rehabilitation process. A subdermal burn involves destruction of the epidermis and dermis and extends more deeply into the fat, muscle, tendon, and bone (Figure 25–5). This type of injury usually results in significant loss of function and may necessitate amputation of appendages if tissue necrosis is significant.
COMPLICATIONS IN BURN INJURY
Burns that result from electrical injuries typically account for 5% of annual burn admissions in the United States and are divided into high-voltage (> 1000 V) and low-voltage (< 1000 V) injuries. Both types of injury pose unique challenges. In an electrical injury, the current travels the path of least resistance through the body, which can cause significant peripheral and central nervous system damage as well as potentially life-threatening arrhythmias and myocardial necrosis, with little apparent cutaneous injury. Moreover, the presentation of these symptoms may be delayed, which further impacts the rehabilitation process and may lead to permanent functional impairments. High-voltage injuries are also more readily associated with amputation and increased length of hospital stay. Lightning strikes are a rare type of high-voltage electrical injury that can pose significant complications both acutely and at a late stage; these include encephalopathy, myelopathy, ocular complications (macular holes and cataracts), and hearing loss.
In heterotopic ossification, new bone forms in tissues that normally do not ossify. The incidence in the general burn population is relatively rare (between 1% and 3%). Heterotopic ossification can occur in burned or unburned areas and affect all major joints; however, most commonly the posterior elbow is affected, followed by the shoulder and hip. Pathogenesis is not completely understood. Risk factors that have been suggested include delayed wound closure, long periods of immobilization with vigorous remobilization, resistance to physical therapy, and genetic predisposition. Recent reports indicate that the extent of burn area is not a determining factor; in fact, heterotopic ossification has been noted in patients with burns involving less than 10% of TBSA.
Early symptoms include pain and joint swelling, along with reluctance to move the affected joint. Clinical observation and bone scans can enable diagnosis at an earlier stage than radiographic changes, and ossification is often detected by physical and occupational therapists during rehabilitation.
Treatment and prevention of heterotopic ossification remains controversial. Current recommendations suggest early excision and grafting, and obtaining radiographs immediately upon observation of unusual swelling at a joint accompanied by a patient’s reluctance to move a joint freely. Once heterotopic bone or calcification is confirmed by radiographs, restricting joint exercise to gentle passive and assisted active range of motion (ROM), only, is recommended. Surgical resection is indicated when ROM is significantly decreased and should be performed only when scars are mature, the patient is well, and bone growth is mature or suspected neurovascular compromise is present. However, heterotopic ossification can recur even after surgical resection.
Peripheral neuropathy in burns has been found to seriously impair rehabilitation and tends to correlate highly with electrical burns, full-thickness burns, burn involvement of greater than 20% of TBSA, and individuals older than 20 years of age. There are several types of neuropathy in burns, including mononeuropathies, peripheral polyneuropathies, and patterns that resemble mononeuritis multiplex. In deeper and larger TBSA injuries, axonal injury is more prevalent than demyelinating neuropathies. Median sensory neuropathies are the most common peripheral nerve abnormality after burn injury. If electrodiagnostic testing is necessary in a burn patient, the practitioner should bear in mind that skin changes after burn injury (including thickened hypertrophic scars) can alter the results of both nerve conduction testing and electromyography; caution should therefore be exercised in the interpretation of test results.
Most patients (nearly 90%) develop severe itching after a burn injury. This itching, even with small burns, is very distressing to patients, often affects daily living activities, and can cause skin breakdown and loss of sleep. Itching can be worse in extreme heat, during physical activity, and in times of stress. The exact mechanism of itching is not understood but may be related to increased mast cell and histamine presence in the burn scar and increased nerve endings and substance P. The treatment for pruritus is based on trial and error and always includes the use of skin moisturizers several times per day. Trials of diphenhydramine hydrochloride and other antihistamines, gabapentin, doxepin, and analgesics, as well as cool compresses, loose clothing, and massage, may also be tried to relieve burn itch. Additionally, advising that itching is part of the “normal” healing process may assist patients in coping with this complication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree