Fig. 22.1
The zonal classification of component fixation in revision TKA (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery. Morgan-Jones et al. [8]. (Figure 1))
22.3.1.1 Fixation in Zone 1: The Epiphysis (Joint Surface)
Zone 1 is compromised by all causes of implant failure, and further bone loss can occur at implant removal. To allow fixation in Zone 1, it is necessary to establish a stable surface, free of sclerotic bone, avascular membrane and loose cement debris. Where bone stock allows, flat aligned cuts with augmentation improve implant stability and fixation. Augmentation by cement, bone graft or metal augment is possible but in Zone 1 reliable fixation is only achieved with PMMA cement. Where augmentation is needed, fixation in at least one other zone is necessary. The geometry of the diaphysis and that of the epiphysis are not congruent; therefore, an offset is sometimes needed to optimise Zone 1 coverage and avoid medial overhang of the tray.
22.3.1.2 Fixation in Zone 2: The Metaphysis
Bone reacts to loading with increased bone density, and when unloaded, bone will be reabsorbed [9, 10]. Traditional revision knee replacement systems bypass the metaphysis concentrating on diaphyseal and joint surface (Zones 3 and 1) fixation. However, fixation in the metaphysis (Zone 2) allows fixation closer to the point of articulation and makes restoration of the joint line easier. The geometry of the metaphysis and that of the joint surface are similar therefore obviating the need for an offset on the tibial implant. Similarly, fixation in Zone 2 allows posterior translation of the femoral component and the use of shorter stems, to mitigate against femoral bowing which moves implants anteriorly. Failure to utilise Zone 2 can lead to uncontrolled biomechanical sheer stress and instability of augment fixation in Zone 1 potentially leading to early failure of the revision [11–13].
There are currently only two options for direct fixation in Zone 2, cement [14] or metaphyseal sleeves (DePuy Synthes) [15, 16]. Cement fixation in metaphyseal bone is not costly, is readily available and can be used with either cemented or uncemented stems. Metaphyseal sleeves have been available since 1975 but have been most widely used as part of the S-ROM Noiles, rotating hinge system which has shown good midterm results [15]. Metaphyseal sleeve fixation optimises load transfer to improve bone regrowth (“Wolff’s law”) and ongrowth [16]. Fixation closer to the joint space provides better restoration of joint line and axial/rotational fixation stability even in the presence of cortical or cancellous bone defects [17, 18]. Metaphyseal sleeves as part of mobile-bearing revision systems have been available for over 30 years but have only belatedly gained popularity, showing good early to midterm results [19–21]. The concept of metaphyseal sleeves was introduced more than 30 years ago and has shown good midterm results [17, 18]. If Zone 1 is sufficiently preserved to accept a worthwhile cement mantle, additional fixation in Zone 3 might not be necessary. However, insufficient data on stemless metaphyseal sleeve fixation exist for general use to be recommended.
Metaphyseal sleeves are the only method available that provides both bone reconstruction and direct implant fixation. Indirect metaphyseal fixation in Zone 2 is possible when reconstruction has been achieved first. As with Zone 1 augmentation, Zone 2 reconstruction can be achieved with cement and bone graft (bulk allograft or morsellised impaction graft) [22] or by the use of a trabecular metal cone (Zimmer) which acts as metal bone graft and is used as a reconstruction ring. Trabecular metal has a structure similar to cancellous bone and is highly biocompatible and osteoconductive [23, 24]. Once metaphyseal reconstruction is secure and stable, secondary Zone 2 fixation is achieved with bone cement. Trabecular metal cones offer the advantages of availability and intraoperative press-fit stability, allowing immediate weight bearing [25, 26]. Zone 2 reconstruction, however achieved, should be supported by secure Zone 3 fixation with either cemented or uncemented stems.
22.3.1.3 Fixation in Zone 3: The Diaphysis
Fixation by diaphyseal stems in Zone 3 will offload the metaphysis, protecting the implant/cement interface from potential failure. Cemented or uncemented stems can be used; both offer long-term survival, but both have individual limitations. In cemented stem fixation, bone resorption occurs in the metaphysis over time [27]. Using cementless stems seems to be beneficial for the bone of the metaphysis [28, 29]; however, radiolucent lines around the stems can be observed in many cases with time. The geometry of the diaphysis and that of the epiphysis are not congruent; therefore, an offset is occasionally needed. With this concept, an optimised coverage of the joint surface can be assured. However, it is still unclear whether a cemented or an uncemented fixation of the stems is advantageous, and optimal length and optimal thickness of the stems are also still unclear [30].
22.4 Reconstruction Options
Management options are based on the severity of defect and the chosen method of bone reconstruction, which range from bone cement, allograft and metal augmentation to megaprosthesis. Recently, new alloys with high porosity have been introduced with satisfactory short-term results [31, 32]; however, it should be recognised that all methods of managing bone loss have different pros and cons [33]. Selection of the best treatment method is based on many factors, including defect size and location, the patient’s age and health and ability to participate in the necessary postoperative rehabilitation. Metaphyseal sleeves and porous tantalum cones are a major addition in dealing with large, central, contained and uncontained defects. The use of stem extensions in cases of bone deficits is helpful in enhancing fixation and lessening stresses to weakened condylar bone [34].
22.4.1 Cement Augmentation
This has limited clinical use and is indicated for small defects 5–10 mm. The advantages of cement are economical (affordable) and universal availability. The disadvantages include difficulty with uncontained defects, early radiolucent lines due to poor fixation and a failure to reconstitute bone for future surgery. However, in the elderly, low-demand patients and for expediency, there remains a role for cement augmentation. Cement augmentation has been combined with metallic screw secured into the bone cortex as a reinforced hybrid construct [34], but this has not found widespread or sustained clinical use.
22.4.2 Bone Graft
When bone grafting, the host bone must be debrided to a viable layer and well cleaned. The graft must be contained and/or compressed and preferably both. The aim, whenever possible, is to produce graft that has inherent structural stability although it always needs protecting with stems. High complication rates have been reported which include graft-host non-union, aseptic loosening, periprosthetic fractures, infections and implant instability [35]. Allografts have several advantages. They are versatile and can be contoured to fill any shape and size (bulk or morcellised impaction grafts). Bone graft has the potential to restore bone stock provided that incorporation occurs, although this is always unpredictable [36, 37].
Disadvantages however are many. Excellent load transfer with bulk graft is seen although this may lead to collapse unless revascularisation and incorporation occur. Outcome is technique and surgeon dependent and remains biologically unpredictable. In many countries and institutions, the supply is limited and expensive. The risk of disease transmission is a real but statistically a minor concern. Failure to re-vascularise and incorporate will give an on-going risk of non-union and collapse. However, acceptable midterm results have been published by several authors for both massive allografts [38] and impaction bone grafting [39]. Other reports have been less favourable for both [40–43]. The risk of infection is minimised by the use of antibiotic-coated cancellous allograft [44].
Autografts have some advantage over allografts. It is more biologically active and carries no risk of disease transmission; contouring is easy with a lower risk of non-union. The disadvantages however are a limited supply and that they provide only small bulk and limited morcellised graft. Autografts are usually only appropriate for complex primary TKA. Bone substitutes are commercially available from many companies. The advantages are the widespread availability of material with both osteoconductive and osteoinductive properties. They are presented in various consistencies such as putties, pastes and injections. There are however major disadvantages of significant cost, uncertain integration and a lack of structural options.
In summary, bone grafting has a place in revision TKA in the chronologically and physiologically young patients to increase bone stock. It offers versatility for differing types of bone loss. Allograft offers bulk for large bone loss, whilst allograft, autograft or bone substitutes may be appropriate for smaller defects.
22.4.3 Prosthetic Augmentation
Most modern revision systems include a complete set of metallic augments and stems. These are designed to reconstruct in Zone 1 (joint surface) and Zone 2 (metaphysis) and support in Zone 3 (diaphysis).
Metal augments have the advantages of availability with no risk of disease transmission, shrinkage or collapse. They offer good load transfer, and cutting guides increase ease and accuracy of use. The disadvantages include limited sizes and shapes producing further host bone loss. Augmentation necessitates the need for diaphyseal stem fixation. Metal augments may be a poor choice in massive defects, modularity may increase debris and reconstruction without use of metaphyseal and diaphyseal bone may lead to early failure [8]. The role of cemented and uncemented stems continues to be debated, but the use of both can be supported [45, 46].
The new generation of metaphyseal implants has made a dramatic difference to bone reconstruction. The commonest options include metaphyseal sleeves (DePuy) [8, 19] or porous reconstruction cones (Zimmer) [47, 48]. Trabecular metal cones have shown good radiographic osseointegration at 1 year, mitigating against future collapse or implant migration [49]. Metaphyseal sleeves have a pedigree of over 30 years of biological fixation allowing physiological loading to help regenerate bone stock and secure long-term fixation [16–21, 50, 51]. Figures 22.2 and 22.3 demonstrate the use of uncemented, metaphyseal sleeves with diaphyseal stems providing multi-zonal fixation in significant bone loss.
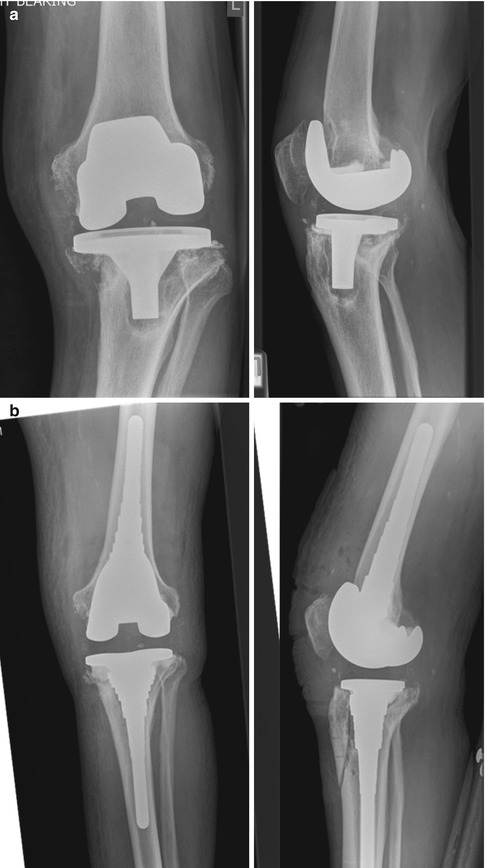
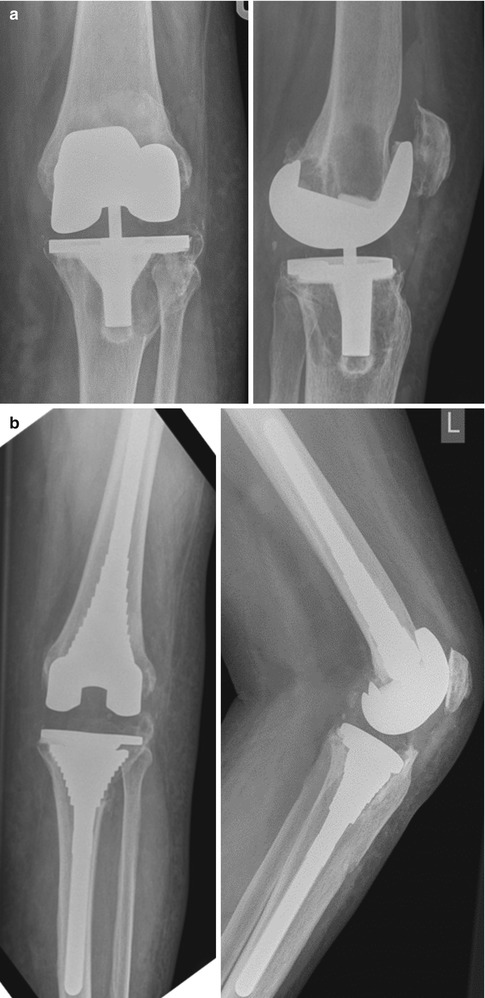
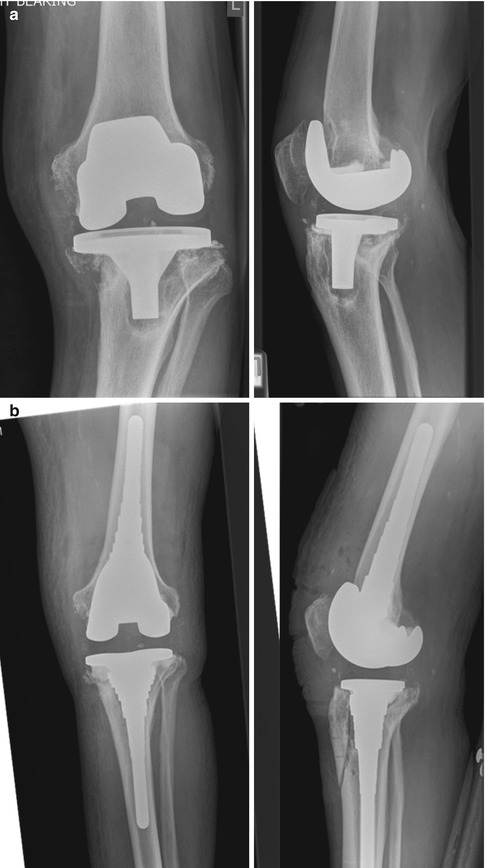
Fig. 22.2
(a) Failed TKA with polyethylene granuloma and aseptic loosening. AORI grade 3 tibial bone loss and grade 2 femoral bone loss. (b) Post-revision X-rays showing multi-zonal fixation: Zone 1 cement, Zone 2 metaphyseal sleeve, Zone 3 stem. Note the tibial crest osteotomy closed with intraosseous sutures
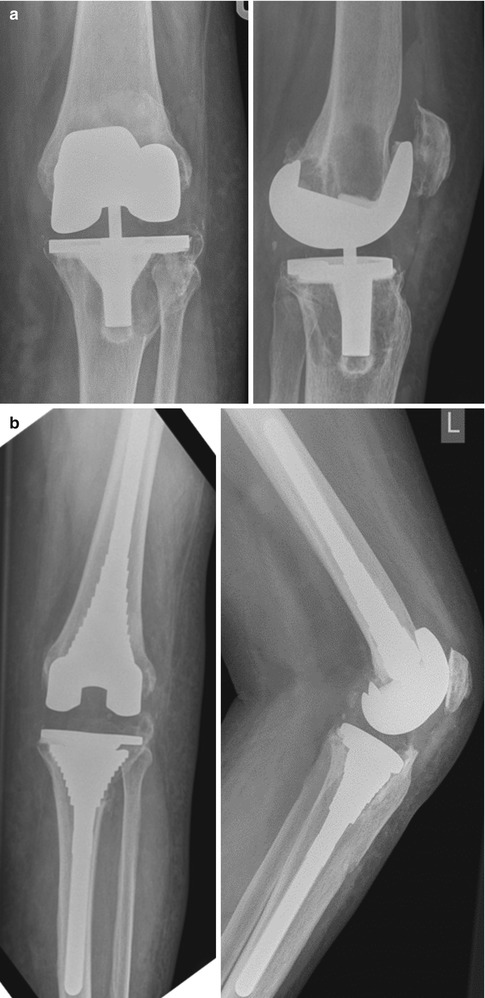
Fig. 22.3




(a) Poorly balanced primary TKA with excess constraint leading to polyethylene wear and bone loss secondary to polyethylene granuloma. AORI classification grade 3 tibia and grade 2 femur. (b) Post-revision X-rays with multi-zonal fixation: Zone 1 cement, Zone 2 metaphyseal sleeve, Zone 3 diaphyseal stem
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








